This cohort study assesses the association between surgeon sex and health care costs following common elective and emergent surgical procedures.
Key Points
Question
Is there an association between surgeon sex and costs of surgical care?
Findings
In this population-based cohort study of 1 165 711 patients, patients treated by female surgeons had lower health care costs at 30 days, 90 days, and 1 year following surgery compared with those treated by male surgeons.
Meaning
In this study, patients treated by female surgeons had lower health care costs following surgery.
Abstract
Importance
Prior research has shown differences in postoperative outcomes for patients treated by female and male surgeons. It is important to understand, from a health system and payer perspective, whether surgical health care costs differ according to the surgeon’s sex.
Objective
To examine the association between surgeon sex and health care costs among patients undergoing surgery.
Design, Setting, and Participants
This population-based, retrospective cohort study included adult patients undergoing 1 of 25 common elective or emergent surgical procedures between January 1, 2007, and December 31, 2019, in Ontario, Canada. Analysis was performed from October 2022 to March 2023.
Exposure
Surgeon sex.
Main Outcome and Measure
The primary outcome was total health care costs assessed 1 year following surgery. Secondarily, total health care costs at 30 and 90 days, as well as specific cost categories, were assessed. Generalized estimating equations were used with procedure-level clustering to compare costs between patients undergoing equivalent surgeries performed by female and male surgeons, with further adjustment for patient-, surgeon-, anesthesiologist-, hospital-, and procedure-level covariates.
Results
Among 1 165 711 included patients, 151 054 were treated by a female surgeon and 1 014 657 were treated by a male surgeon. Analyzed at the procedure-specific level and accounting for patient-, surgeon-, anesthesiologist-, and hospital-level covariates, 1-year total health care costs were higher for patients treated by male surgeons ($24 882; 95% CI, $20 780-$29 794) than female surgeons ($18 517; 95% CI, $16 080-$21 324) (adjusted absolute difference, $6365; 95% CI, $3491-9238; adjusted relative risk, 1.10; 95% CI, 1.05-1.14). Similar patterns were observed at 30 days (adjusted absolute difference, $3115; 95% CI, $1682-$4548) and 90 days (adjusted absolute difference, $4228; 95% CI, $2255-$6202).
Conclusions and Relevance
This analysis found lower 30-day, 90-day, and 1-year health care costs for patients treated by female surgeons compared with those treated by male surgeons. These data further underscore the importance of creating inclusive policies and environments supportive of women surgeons to improve recruitment and retention of a more diverse and representative workforce.
Introduction
Physician sociocultural characteristics, such as sex, are associated with outcomes important to surgical patients and may influence value-based surgical care delivery. Recent evidence has shown that patients treated by a female surgeon had significantly lower rates of death, rehospitalization, and adverse events after surgery compared with similar patients undergoing the same surgeries by a male surgeon.1 Furthermore, there is an important interaction between the sex of the treating surgeon and the patient.2 Women undergoing surgery showed significantly better short-term survival and fewer adverse postoperative events when undergoing surgery with a female surgeon compared with a male surgeon.2 In contrast, male patients have more similar outcomes after surgery by a female or male surgeon.
While the metrics studied to date represent important clinical outcomes, there is a pressing need to evaluate a broader scope of outcomes in health care delivery. Value-based surgical care aims to maximize patient outcomes while minimizing health system costs.3 Value-based care incentivizes efficiency of health care delivery with alignment between pricing of care and patient outcomes.4 To our knowledge, no study has examined the association between surgeon sex and health care costs for patients undergoing surgery.
Thus, the objective of this study was to compare health care costs for patients undergoing common surgeries performed by female and male surgeons. In addition, we further examined the association between surgeon-patient sex concordance and health care costs.
Methods
Overview
The design of this study is consistent with prior work examining patient-level clinical outcomes.1,2,5,6 We conducted a population-based, retrospective cohort study of adults undergoing common surgeries in Ontario, Canada, between January 1, 2007, and December 31, 2019. Ontario residents receive insurance for physician and hospital services through a single government payer, the Ontario Health Insurance Plan. We included patients undergoing 25 common elective and emergent procedures across the spectrum of all surgical subspecialties, including both open and laparoscopic approaches, to ensure generalizability (eTable 1 in Supplement 1). Multidisciplinary consultation was used to select the studied procedures, ranging from low to high perioperative risk. This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline7 and the Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) statement.8 The study protocol was approved by the Mount Sinai Hospital Research Ethics Board. Informed consent was waived by the Mount Sinai Research Ethics Board and ICES given the use of anonymized administrative data records.
Data Sources
We linked the Ontario Health Insurance Plan database (physician billings, laboratory tests, and out-of-province physicians9), the Canadian Institute for Health Information (CIHI) Discharge Abstract Database (hospitalizations10), the CIHI National Ambulatory Care Reporting System (emergency department visits), the Registered Persons Database (demographic information11), and the Corporate Provider Database (physician characteristics). These data sets were linked using unique encoded identifiers and analyzed at ICES.
Cohort Derivation
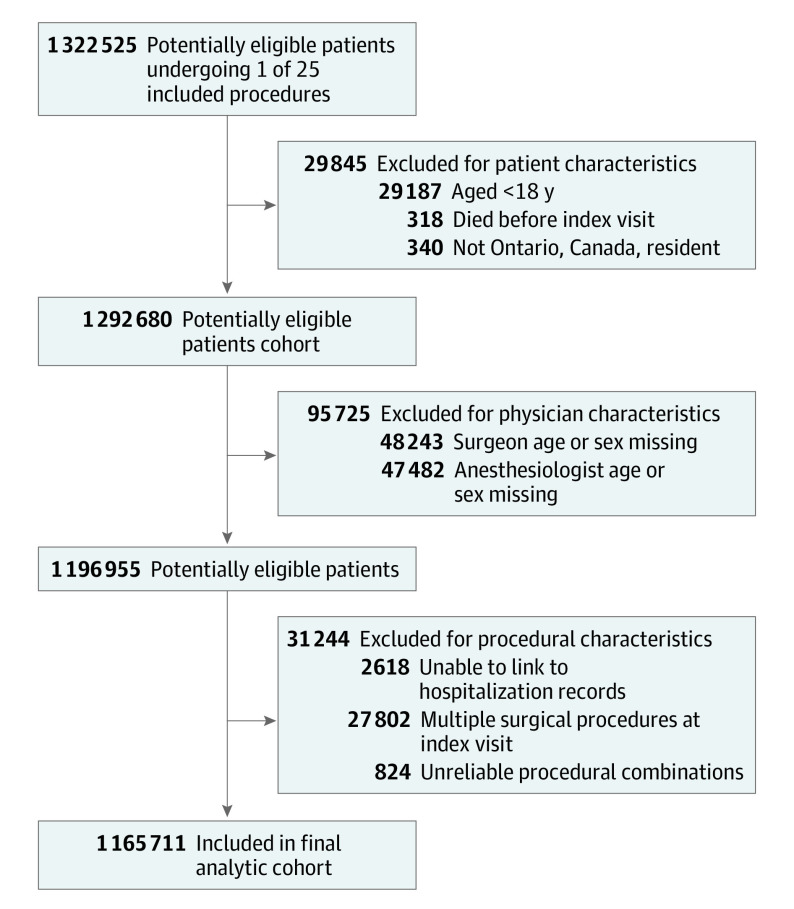
We identified patients who underwent 1 of the 25 index procedures for whom the treating physicians could be identified. We excluded patients younger than 18 years, those who were not Ontario residents, those for whom the date of death preceded the date of surgery, and those for whom we could not reliably ascertain the treating institution. We further excluded those for whom we could not determine the sex or age of the treating surgeon or anesthesiologist, as each of these have been shown to have an association with perioperative outcomes.1,5,12 Finally, we excluded patients with multiple concomitant surgical procedures and those with unusual combinations of surgical specialty and procedure (eg, urology and abdominal aortic aneurysm repair), as these represent uncommon situations or miscoding that would diminish generalizability (Figure 1).
Figure 1. Cohort Derivation.
Outcomes
We examined total health care costs for included patients at 30 days, 90 days, and 1 year following surgery. The primary outcome was total costs at 1 year following surgery. In addition to total costs, we specifically examined a subset of cost categories (inpatient care, postdischarge continuing care, prescription medications, and physician professional fees).
Patient-level costs were determined using costing methods developed for health care administrative data in Ontario,13 an approach that has been extensively validated and used across health care contexts, including surgical care, chronic disease, critical care, spinal cord injury, and trauma.14,15,16,17,18 Costs are calculated using the CIHI resource intensity weight value and multiplying it by cost per weighted case, which is averaged across the province.13,19,20 All dollar figures are inflation adjusted to 2020 Canadian dollars.
Exposure
Physician sex was determined from the Corporate Provider Database, derived from physician self-report at the time of credentialing or registration with the Ontario Ministry of Health. Due to the data set, we were unable to assess surgeon self-reported gender. Primarily, we assessed the association between surgeon sex and patient-level health care costs. Secondarily, we considered the association between patient-surgeon sex concordance and costs. In keeping with prior work by some of us,2 we considered a multilevel categorical variable with the 4 combinations of patient and surgeon sex: male patient and male surgeon, female patient and male surgeon, male patient and female surgeon, and female patient and female surgeon.
Covariates
Patient age, sex, geographic location (local health integration networks21), geographically derived socioeconomic status, rurality, and general comorbidity (Johns Hopkins Aggregated Diagnosis Groups)22 were obtained. We also collected data regarding surgeon sex, age, years in practice, specialty, and surgical volume. Surgical volume was determined for each surgeon and procedure by identifying the number of identical procedures that the operating surgeon performed in the previous year, operationalized in quartiles. We additionally collected data regarding anesthesiologist sex, age, years in practice, and annual case volume, as these have been associated with short-term perioperative outcomes.5,12 Hospital institution identifiers were used to account for facility-level variability. We defined a surgical procedure as emergent or elective using the CIHI Discharge Abstract Database. All same-day surgical procedures were considered elective. The duration of surgery (in minutes) was also collected.
Statistical Analysis
Descriptive statistics were used to compare the characteristics of patients, surgeons, anesthesiologists, and hospitals according to the sex of the surgeon. As traditional statistical measures are likely to demonstrate significant differences where no clinically important difference exists due to large sample size, we performed between-group comparisons using standardized differences, with a clinically important difference defined as greater than 0.10.23
We used multivariable generalized estimating equations (GEEs) with an independent correlation structure and a negative binomial distribution with a log link to calculate both patient-level adjusted mean costs and adjusted relative risk, stratified by surgeon sex and patient-surgeon sex dyads and accounting for the aforementioned patient-, surgeon-, anesthesiologist-, and hospital-level covariates (determined a priori) and procedure year; clustering on the specific procedure performed was done to compare costs for patients undergoing the same procedure. When GEE negative binomial models did not converge (as was the case for subsets of costs, including inpatient costs, postdischarge care costs, and prescription medication costs), ordinary negative binomial models were used. Adjusted means costs were obtained with the LSMean option in proc genmod in SAS, version 6.1 (SAS Institute Inc). To obtain the difference in adjusted means, the NLMeans macro was used. The unit of analysis was the patient. We assessed model assumptions, including collinearity, and found no violations.
We performed a priori determined subgroup analyses to assess for heterogeneity of effect according to patient-, surgeon-, anesthesiologist-, procedure- (including urgency and complexity), and facility-level characteristics. We further performed sensitivity analysis by adding the duration of surgery as a covariate among the subset of patients with complete data on this variable.
Statistical significance was set at P < .05 based on a 2-tailed comparison. Analysis was performed from October 2022 to March 2023.
Results
Of the 1 322 525 patients who underwent 1 of the 25 index procedures for whom the treating physicians could be identified, 156 814 were excluded (details given in Figure 1). Among the 1 165 711 included patients, 151 054 were treated by a female surgeon and 1 014 657 were treated by a male surgeon. Female surgeons were younger, and their patients were also younger, were more likely to be female, and had fewer comorbidities compared with those treated by male surgeons (eTable 2 in Supplement 1). There were also differences in surgical specialties: patients treated by female surgeons were more likely to have undergone general, obstetric or gynecologic, or plastic surgeries, while those treated by male surgeons were more likely to have undergone cardiac, neurosurgical, orthopedic, or urologic procedures. Patients treated by male physicians were more likely to have a surgeon in the top quartiles of surgical volume. The median surgical duration was longer among patients treated by female surgeons (118 minutes; IQR, 82-169 minutes) than male surgeons (103 minutes; IQR, 74-144 minutes).
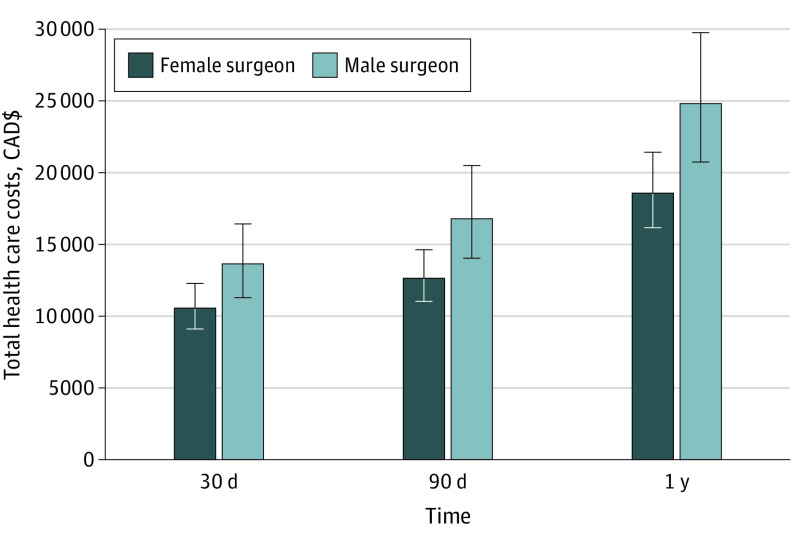
Across the cohort, following multivariable regression accounting for patient-, surgeon-, anesthesiologist-, and hospital-level covariates, 1-year adjusted total health care costs were significantly higher for patients treated by male surgeons (adjusted mean cost, $24 882; 95% CI, $20 780-$29 794) than those treated by female surgeons (adjusted mean cost, $18 517; 95% CI, $16 080-$21 324) (adjusted absolute difference, $6365; 95% CI, $3491-$9238; adjusted relative risk, 1.10; 95% CI, 1.05-1.14) (Figure 2). Similar patterns were seen at 30 days (adjusted absolute difference, $3115; 95% CI, $1682-$4548; adjusted relative risk, 1.09; 95% CI, 1.05-1.13) and 90 days (adjusted absolute difference, $4228; 95% CI, $2255-$6202; adjusted relative risk, 1.10; 95% CI, 1.06-1.14) following surgery (Table 1 and Table 2). Examining specific cost categories, we observed a higher adjusted relative risk (ARR) for surgeon sex and inpatient costs (ARR, 1.15; 95% CI, 1.13-1.16) and postdischarge continuing care (ARR, 1.08; 95% CI, 1.06-1.11) than for prescription medications (ARR, 1.04; 95% CI, 1.02-1.06) or physician costs (ARR, 1.08; 95% CI, 1.04-1.12).
Figure 2. Association Between Surgeon Sex and Health Care–Related Costs for Patients Undergoing Common Surgical Procedures in Ontario, Canada.
Error bars indicate 95% CIs. The 2020 CAD to USD conversion was approximately 1.34 CAD per 1 USD.
Table 1. Multivariable-Adjusted Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Surgeon Sex.
| Period and outcome | Adjusted mean cost, $ (95% CI) | Adjusted mean difference in cost, $ (95% CI) | |
|---|---|---|---|
| Male surgeons | Female surgeons | ||
| Within 30 d | |||
| Total health care costsa | 13 592 (11 250 to 16 423) | 10 477 (9018 to 12 173) | −3115 (−4548 to −1682) |
| Inpatient costsa | 8416 (6452 to 10 978) | 6309 (4772 to 8340) | −2108 (−3182 to −1033) |
| Postdischarge care costsb,c | 969 (960 to 977) | 453 (443 to 463) | −515 (−528 to −502) |
| Prescription medication costsb | 79 (79 to 80) | 51 (50 to 51) | −29 (−30 to −28) |
| Physician costsd,e | 2646 (2224 to 3148) | 2169 (1914 to 2458) | −477 (−759 to −195) |
| Within 90 d | |||
| Total health care costsa | 16 898 (13 924 to 20 507) | 12 670 (10 937 to 14 677) | −4228 (−6202 to −2255) |
| Inpatient costsb | 8574 (8541 to 8608) | 6407 (6342 to 6473) | −2167 (−2241 to −2094) |
| Postdischarge care costsb,c | 1626 (1612 to 1639) | 725 (709 to 741) | −901 (−922 to −880) |
| Prescription medication costsb | 229 (227 to 230) | 152 (150 to 154) | −77 (−79 to −74) |
| Physician costsa,e | 3064 (2619 to 3584) | 2494 (2250 to 2765) | −569 (−888 to −251) |
| Within 1 y | |||
| Total health care costsa | 24 882 (20 780 to 29 794) | 18 517 (16 080 to 21 324) | −6365 (−9238 to −3491) |
| Inpatient costsa | 11 600 (9073 to 14 830) | 8256 (6498 to 10 490) | −3344 (−4779 to −1908) |
| Postdischarge care costsb,c | 2837 (2813 to 2862) | 1265 (1238 to 1292) | −1572 (−1608 to −1536) |
| Prescription medication costsb | 872 (867 to 877) | 612 (603 to 622) | −260 (−271 to −249) |
| Physician costsc,e | 4289 (3712 to 4955) | 3586 (3228 to 3984) | −702 (−1076 to −329) |
Results from generalized estimating equation negative binomial modeling with clustering based on procedure fee code, adjusted for surgeon age, annual case volume, and years in practice; anesthesiologist age, annual case volume, and years in practice; patient age, comorbidity, rurality, and income quintile; and hospital status.
Results from ordinary negative binomial modeling, adjusted for surgeon age, annual case volume, and years in practice; anesthesiologist age, annual case volume, and years in practice; and patient age and comorbidity.
Includes National Rehabilitation Reporting System, Continuing Care Costs, long-term, and Home Care Database.
Results from generalized estimating equation negative binomial modeling with clustering based on procedure fee code, adjusted for surgeon age, annual case volume, and years in practice; anesthesiologist age, annual case volume, and years in practice; and patient age and comorbidity.
Includes fee-for-service billings payable through the Ontario Health Insurance Plan for general practitioners and specialist physicians.
Table 2. Multivariable-Adjusted Relative Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries Treated by Male Surgeons vs Female Surgeonsa.
| Costs | Within 30 d | Within 90 d | Within 1 y | |||
|---|---|---|---|---|---|---|
| ARR (95% CI) | P value | ARR (95% CI) | P value | ARR (95% CI) | P value | |
| Total health care costs | 1.09 (1.05-1.13) | <.001 | 1.10 (1.06-1.14) | <.001 | 1.10 (1.05-1.14) | <.001 |
| Inpatient costsb | 1.15 (1.13-1.16) | <.001 | 1.16 (1.14-1.17) | <.001 | 1.15 (1.13-1.16) | <.001 |
| Postdischarge care costsb | 1.08 (1.06-1.11) | <.001 | 1.13 (1.11-1.16) | <.001 | 1.14 (1.11-1.17) | <.001 |
| Prescription medication costsb | 1.04 (1.02-1.06) | <.001 | 1.03 (1.01-1.05) | <.001 | 1.03 (1.02-1.05) | <.001 |
| Physician costs | 1.08 (1.04-1.12) | <.001 | 1.07 (1.04-1.12) | <.001 | 1.06 (1.03-1.09) | <.001 |
Abbreviation: ARR, adjusted relative risk.
Using generalized estimating equation modeling with clustering based on procedure fee code (negative binomial regression with log link), adjusted for surgeon age (continuous), annual case volume (quartiles), specialty, and years of practice (continuous); anesthesiologist age (continuous), sex, annual case volume (quartiles), and years of practice (continuous); patient age (continuous), sex, comorbidity (categorical), rurality (rural vs urban), and income quintile; local health integration network; hospital status (academic vs community); and index year.
Results are from ordinary negative binomial models because the generalized estimating equation negative binomial models did not converge.
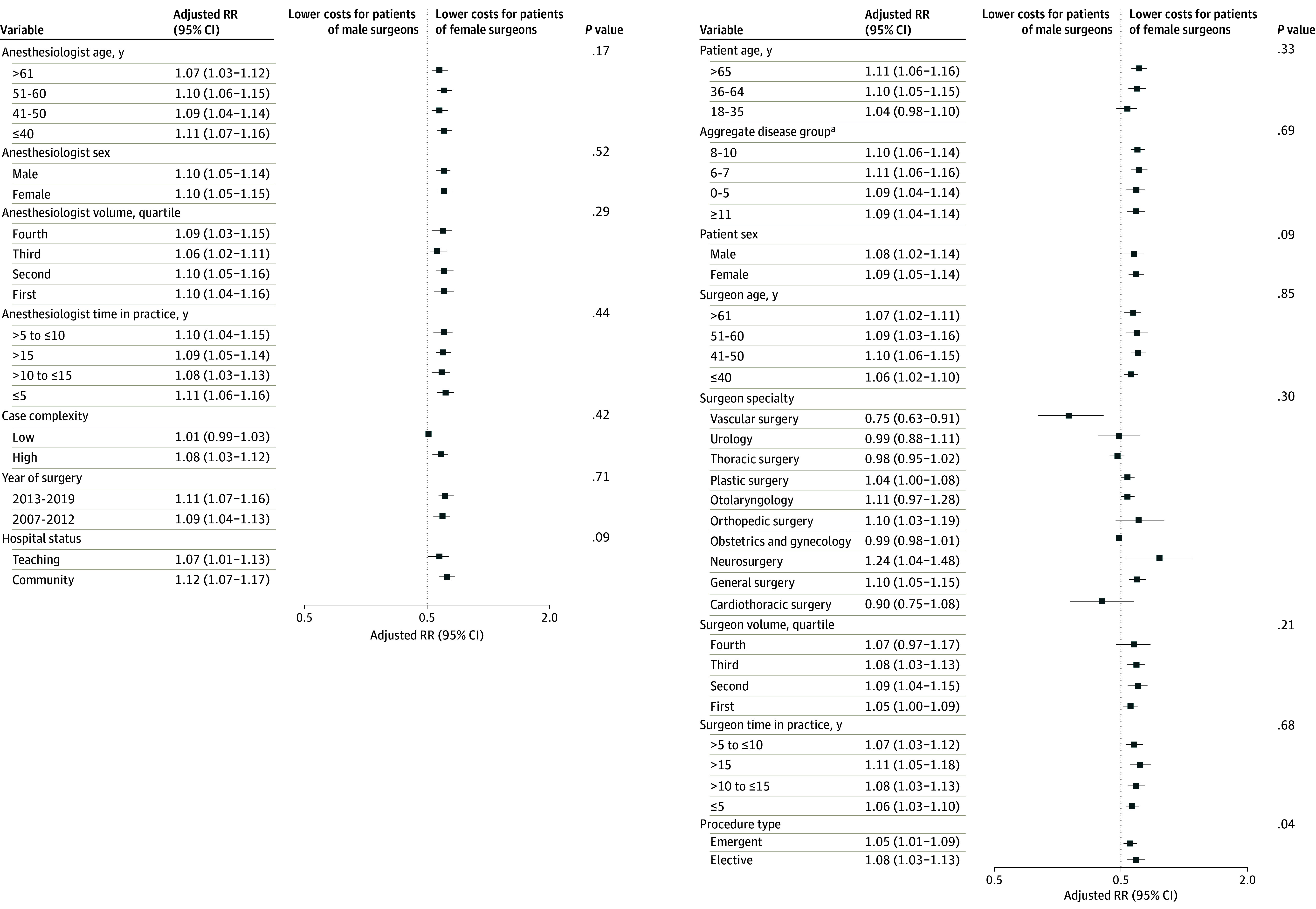
In subgroup analyses assessing total health care costs at 1 year following surgery, there was no evidence of effect modification when analyses were stratified according to surgeon specialty, age, volume, or years in practice; hospital status; case complexity; patient age, sex, or comorbidity; anesthesiologist age, sex, volume, or years in practice; or era of surgery (Figure 3). However, the ARR was higher for elective surgeries (ARR, 1.08; 95% CI, 1.03-1.13) than for emergent procedures (ARR, 1.05; 95% CI, 1.01-1.09) (test for subgroup differences P = .04).
Figure 3. Subgroup Analysis Assessing the Association Between Surgeon Sex and Total Health Care Costs at 1 Year, Stratified by Surgeon, Patient, Anesthesiologist, Procedure, and Hospital Characteristics.
When adjusting for the same aforementioned covariates, 1-year adjusted total health care costs were highest for male patients treated by male surgeons (adjusted mean cost, $28 869; 95% CI, $23 172-$35 966) followed by male patients treated by female surgeons (adjusted mean cost, $25 050; 95% CI, $18 945-$33 123), female patients treated by male surgeons (adjusted mean cost, $21 751; 95% CI, $17 931-$26 385), and female patients treated by female surgeons (adjusted mean cost, $16 324; 95% CI, $14 311-$18 619) (eTable 3 in Supplement 1). For both female and male patients, across all time points, total health care costs were higher for patients treated by male surgeons than those treated by female surgeons (eTables 3-5 in Supplement 1).
Similar patterns were observed when we examined crude costs (eTables 6 and 7 in Supplement 1). Sensitivity analyses including surgical duration as a covariate (1 100 193 patients [94.3%]) were consistent with the primary analysis, demonstrating slightly higher ARRs (eTables 8 and 9 in Supplement 1).
Discussion
In this large, population-based multidisciplinary cohort study, total health care costs were significantly lower among patients treated by female surgeons than among patients treated by male surgeons. This association was observed across multiple time points and subgroup analyses defined by surgeon, patient, procedure, anesthesiologist, and hospital groups. When combined with prior work assessing rates of adverse postoperative outcomes,1 the available data support better clinical outcomes and lower health care costs for patients treated by female surgeons. Additionally, we noted that costs of care were lower for female patients compared with men undergoing the same surgical procedures.
To our knowledge, this is the first study to assess the association between surgeon sex and patient-surgeon sex concordance with health care costs following common elective and emergent surgical procedures. Multiple prior studies1,24,25 have assessed the association between surgeon sex and short-term surgical outcomes. In the study most comparable to this one, patients treated by female physicians had better outcomes, including mortality, complications, reoperation, and readmission, after surgery.1 Similar differences in patient outcomes according to physician sex have been seen among patients with myocardial infarction in emergency departments26 and those admitted to internal medicine services with general medical diagnoses.27 However, these studies did not investigate the association between physician sex and costs of care.
While the present study demonstrated differential health care costs based on surgeon sex, the underlying reasons are unknown. Observations from examining subsets of health care costs in this cohort revealed important drivers of differential costs: inpatient and postdischarge continuing care costs showed the greatest difference between patients treated by female surgeons and those treated by male surgeons. Many factors are likely to contribute to these costs, which may include differences in the preoperative and perioperative practices of surgeons, surgical decision-making, and the use of intraoperative equipment or technologies. Given prior data showing higher rates of adverse postoperative outcomes among patients treated by male surgeons,1 management of these complications likely contributes to additional costs through higher health care needs and longer inpatient stays.28,29 Early evidence suggests different practice patterns between female and male physicians, with women demonstrating greater guideline concordance, patient-centric care, and open communication styles.30,31,32,33,34 Further qualitative research is needed among surgeons to better understand how decision-making and practice style affect patient recovery after surgery and costs of care.
Despite the consistency of our findings across multiple subgroup analyses and generalizability seen in patient outcomes across health care settings, it is possible that our results may represent residual confounding or be due to chance alone. More important, we used GEEs with clustering according to the specific procedure performed to allow comparisons between patients undergoing the same procedures by male or female surgeons. Beyond this, we used robust case-mix adjustment accounting for patient factors, including age, sex, geographic location, socioeconomic status, rurality, and general comorbidity, as well as important surgeon, anesthesiologist, procedure, and hospital characteristics. We used negative binomial regression modeling, 1 of several accepted approaches for modeling cost data.35 Additionally, the differences in patient populations between male and female surgeons may reflect surgical decision-making, with female surgeons potentially having better patient selection preoperatively. Thus, residual differences may represent the causal pathway rather than confounding, but this observational study could not assess causation. Although this more proximally would explain improved clinical outcomes, the cost of managing complications28,29 means that this may additionally affect health care costs.
Considering the importance of surgical care, these findings may have important health system implications. Among the sample of 1 165 711 patients undergoing 25 different procedures over a 13-year period in Ontario, extrapolation of the per-cost difference between female and male surgeons corresponds to a cost difference of CAD $3.14 billion over a 30-day horizon (2020 USD $4.21 billion), CAD $4.37 billion over a 90-day horizon (2020 USD $5.86 billion), and CAD $6.72 billion over a 1-year horizon (2020 USD $9.01 billion). In the US, annual expenditures for surgical care exceeded USD $120 billion as of 2014.36 Thus, the relative difference in total health care costs following surgery between patients treated by female and male surgeons of approximately 10% (ARR, 1.10) demonstrated here represents potentially large cost savings.
Strengths and Limitations
This study has notable strengths that bolster both the external and the internal validity. First, we were able to provide generalizable results, as we used a large, population-based data set in a universal health care system and included all surgical subspecialties as well as both elective and emergent procedures. Second, we used a robust and validated approach to health care costing that leveraged administrative data to allow for comprehensive ascertainment of health care costs. This is particularly important for the assessment of long-term outcomes, as over time, patients are increasingly likely to seek care at institutions other than the one in which they initially underwent surgery. Third, this study is generalizable to many countries with public funded health care. The findings are also relevant to insurance-based privatized health systems, including in the US, which share similar models of surgical training and practice and a focus on improving value in health care delivery.
There are inevitable limitations due to the observational nature of this study. First, due to the administrative data sets used, we captured binary biologic sex and were unable to assess either patient or surgeon gender. Furthermore, we were unable to capture other potentially important aspects of identity, including race and ethnicity, professional hierarchy, and disability, or other potentially important unmeasured physician sociocultural factors, individual characteristic traits, unconscious bias, and communication styles, which may have resulted in confounding. Additionally, the use of health administrative data precluded us from assessing qualitative differences in practice patterns either between male and female surgeons broadly or among individual surgeons specifically. Second, we used 1 of several accepted modeling strategies for cost data; while model fit parameters indicated that this was an appropriate choice, there are alterative approaches.35 Third, while we accounted for the procedure performed (defined by billing codes), we were unable to capture granular metrics of case complexity, and thus, there may have been heterogeneity in complexity within procedure types that we were unable to capture. Fourth, we accounted for the role of anesthesiologists in the analysis but could not account for the potential effect of other team members (ie, residents, nurses) who are not captured in administrative data sets. Fifth, due to limitations of the data sets used, we were unable to granularly assess intraoperative resource and equipment use or waste. Sixth, while we used GEEs to account for procedure-level clustering for total health care costs at each time point, these models did not converge for several specific cost categories and we instead report ordinary negative binomial models.
Conclusions
This large, population-level cohort study found significantly lower short- and long-term costs of care for patients treated by female surgeons compared with male surgeons. These data further underscore the importance of creating inclusive policies and environments supportive of women surgeons to improve recruitment and retention of a more diverse and representative workforce. Furthermore, they justify work to better understand the personality traits and practice behaviors that underpin these sex-based differences in outcomes. Together, these actions are vital for offering the highest value care for all patients undergoing surgery.
eTable 1. List of Included Procedures
eTable 2. Baseline Characteristics of Study Cohort, Stratified by Surgeon Sex
eTable 3. Multivariable Adjusted Total Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Dyad
eTable 4. Multivariable Adjusted Relative Total Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Dyad
eTable 5. Multivariable Adjusted Health Care Costs For Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Concordance
eTable 6. Crude Costs, Stratified by Surgeon Sex
eTable 7. Crude Costs, Stratified by Patient-Surgeon Sex Concordance
eTable 8. Sensitivity Analysis of Multivariable Adjusted Models Assessing the Association Between Surgeon Sex and Total Health Care Costs, Further Including Operative Duration as a Covariate
eTable 9. Sensitivity Analysis of Multivariable Adjusted Models Assessing the Association Between Patient-Surgeon Sex Concordance and Total Health Care Costs, Further Including Operative Duration as a Covariate
Data Sharing Statement
References
- 1.Wallis CJ, Ravi B, Coburn N, Nam RK, Detsky AS, Satkunasivam R. Comparison of postoperative outcomes among patients treated by male and female surgeons: a population based matched cohort study. BMJ. 2017;359:j4366. doi: 10.1136/bmj.j4366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallis CJD, Jerath A, Coburn N, et al. Association of surgeon-patient sex concordance with postoperative outcomes. JAMA Surg. 2022;157(2):146-156. doi: 10.1001/jamasurg.2021.6339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Porter ME. What is value in health care? N Engl J Med. 2010;363(26):2477-2481. doi: 10.1056/NEJMp1011024 [DOI] [PubMed] [Google Scholar]
- 4.NEJM Catalyst. What is value-based healthcare? 2017. Accessed February 12, 2023. https://catalyst.nejm.org/doi/full/10.1056/CAT.17.0558
- 5.Wallis CJD, Jerath A, Kaneshwaran K, et al. Association between surgeon and anesthesiologist sex discordance and postoperative outcomes: a population-based cohort study. Ann Surg. 2022;276(1):81-87. doi: 10.1097/SLA.0000000000005495 [DOI] [PubMed] [Google Scholar]
- 6.Satkunasivam R, Klaassen Z, Ravi B, et al. Relation between surgeon age and postoperative outcomes: a population-based cohort study. CMAJ. 2020;192(15):E385-E392. doi: 10.1503/cmaj.190820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573-577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 8.Benchimol EI, Smeeth L, Guttmann A, et al. ; RECORD Working Committee . The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams JI, Young W. A summary of studies on the quality of health care administrative databases in Canada. In: Goel V, Williams J, Anderson G, et al. , eds. Patterns of Health Care in Ontario, Canada: The ICES Practice Atlas. Canadian Medical Association; 1996:339-345. [Google Scholar]
- 10.Juurlink DN, Preyra C, Croxford R, et al. Canadian Institute for Health Information Discharge Abstract Database: A Validation Study. Institute for Clinical Evaluation Sciences; 2006. [Google Scholar]
- 11.Iron K, Zagorski BM, Sykora K, Manuel DG. Living and dying in Ontario: an opportunity for improved health information. ICES Investigative Report; 2008. Accessed April 11, 2023. https://www.ices.on.ca/publications/research-reports/living-and-dying-in-ontario-an-opportunity-to-improve-health-information/
- 12.Hallet J, Jerath A, Turgeon AF, et al. Association between anesthesiologist volume and short-term outcomes in complex gastrointestinal cancer surgery. JAMA Surg. 2021;156(5):479-487. doi: 10.1001/jamasurg.2021.0135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wodchis WPBK, Nikitovic M, McKillop I. Guidelines on person level costing using administrative databases in Ontario. Working Paper Series. Vol 1. Health System Performance Research Network; 2013. https://hdl.handle.net/1807/87373
- 14.Munce SE, Wodchis WP, Guilcher SJ, et al. Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord. 2013;51(1):64-69. doi: 10.1038/sc.2012.81 [DOI] [PubMed] [Google Scholar]
- 15.Wodchis WP, Austin PC, Henry DA. A 3-year study of high-cost users of health care. CMAJ. 2016;188(3):182-188. doi: 10.1503/cmaj.150064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaudhuri D, Tanuseputro P, Herritt B, D’Egidio G, Chalifoux M, Kyeremanteng K. Critical care at the end of life: a population-level cohort study of cost and outcomes. Crit Care. 2017;21(1):124. doi: 10.1186/s13054-017-1711-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pincus D, Wasserstein D, Nathens AB, Bai YQ, Redelmeier DA, Wodchis WP. Direct medical costs of motorcycle crashes in Ontario. CMAJ. 2017;189(46):E1410-E1415. doi: 10.1503/cmaj.170337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Garbens A, Wallis CJD, Matta R, et al. The cost of treatment and its related complications for men who receive surgery or radiation therapy for prostate cancer. Can Urol Assoc J. 2019;13(8):E236-E248. doi: 10.5489/cuaj.5598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen A, Bushmeneva K, Zagorski B, Colantonio A, Parsons D, Wodchis WP. Direct cost associated with acquired brain injury in Ontario. BMC Neurol. 2012;12:76. doi: 10.1186/1471-2377-12-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Canadian Institute for Health Information . Patient cost estimator methodological notes and glossary. 2013. Accessed March 20, 2023. https://www.cihi.ca/sites/default/files/document/pce-methodology-notes-2020-en-web.pdf
- 21.MacLeod H. Local Health Integration Networks: build on their purpose. Published online September 28, 2015. doi: 10.1177/0840470415600127 [DOI] [PubMed] [Google Scholar]
- 22.Austin PC, van Walraven C, Wodchis WP, Newman A, Anderson GM. Using the Johns Hopkins Aggregated Diagnosis Groups (ADGs) to predict mortality in a general adult population cohort in Ontario, Canada. Med Care. 2011;49(10):932-939. doi: 10.1097/MLR.0b013e318215d5e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228-1234. doi: 10.1080/03610910902859574 [DOI] [Google Scholar]
- 24.Tsugawa Y, Jena AB, Orav EJ, et al. Age and sex of surgeons and mortality of older surgical patients: observational study. BMJ. 2018;361:k1343. doi: 10.1136/bmj.k1343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Okoshi K, Endo H, Nomura S, et al. Comparison of short term surgical outcomes of male and female gastrointestinal surgeons in Japan: retrospective cohort study. BMJ. 2022;378:e070568. doi: 10.1136/bmj-2022-070568 [DOI] [PubMed] [Google Scholar]
- 26.Greenwood BN, Carnahan S, Huang L. Patient-physician gender concordance and increased mortality among female heart attack patients. Proc Natl Acad Sci U S A. 2018;115(34):8569-8574. doi: 10.1073/pnas.1800097115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsugawa Y, Jena AB, Figueroa JF, Orav EJ, Blumenthal DM, Jha AK. Comparison of hospital mortality and readmission rates for Medicare patients treated by male vs female physicians. JAMA Intern Med. 2017;177(2):206-213. doi: 10.1001/jamainternmed.2016.7875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Garbens A, Goldenberg M, Wallis CJD, Tricco A, Grantcharov TP. The cost of intraoperative adverse events in abdominal and pelvic surgery: a systematic review. Am J Surg. 2018;215(1):163-170. doi: 10.1016/j.amjsurg.2017.06.025 [DOI] [PubMed] [Google Scholar]
- 29.Gomez-Rosado JC, Salas-Turrens J, Olry-de-Labry-Lima A. Economic cost analysis related to complications in general and digestive surgery. Cir Esp (Engl Ed). 2018;96(5):292-299. doi: 10.1016/j.ciresp.2018.02.011 [DOI] [PubMed] [Google Scholar]
- 30.Frank E, Dresner Y, Shani M, Vinker S. The association between physicians’ and patients’ preventive health practices. CMAJ. 2013;185(8):649-653. doi: 10.1503/cmaj.121028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women: does the sex of the physician matter? N Engl J Med. 1993;329(7):478-482. doi: 10.1056/NEJM199308123290707 [DOI] [PubMed] [Google Scholar]
- 32.Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33(4):407-416. doi: 10.1097/00005650-199504000-00007 [DOI] [PubMed] [Google Scholar]
- 33.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288(6):756-764. doi: 10.1001/jama.288.6.756 [DOI] [PubMed] [Google Scholar]
- 34.Berthold HK, Gouni-Berthold I, Bestehorn KP, Böhm M, Krone W. Physician gender is associated with the quality of type 2 diabetes care. J Intern Med. 2008;264(4):340-350. doi: 10.1111/j.1365-2796.2008.01967.x [DOI] [PubMed] [Google Scholar]
- 35.Austin PC, Ghali WA, Tu JV. A comparison of several regression models for analysing cost of CABG surgery. Stat Med. 2003;22(17):2799-2815. doi: 10.1002/sim.1442 [DOI] [PubMed] [Google Scholar]
- 36.Kaye DR, Luckenbaugh AN, Oerline M, et al. Understanding the costs associated with surgical care delivery in the Medicare population. Ann Surg. 2020;271(1):23-28. doi: 10.1097/SLA.0000000000003165 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. List of Included Procedures
eTable 2. Baseline Characteristics of Study Cohort, Stratified by Surgeon Sex
eTable 3. Multivariable Adjusted Total Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Dyad
eTable 4. Multivariable Adjusted Relative Total Health Care Costs for Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Dyad
eTable 5. Multivariable Adjusted Health Care Costs For Patients Undergoing Common Elective and Emergent Surgeries, Stratified by Patient-Surgeon Sex Concordance
eTable 6. Crude Costs, Stratified by Surgeon Sex
eTable 7. Crude Costs, Stratified by Patient-Surgeon Sex Concordance
eTable 8. Sensitivity Analysis of Multivariable Adjusted Models Assessing the Association Between Surgeon Sex and Total Health Care Costs, Further Including Operative Duration as a Covariate
eTable 9. Sensitivity Analysis of Multivariable Adjusted Models Assessing the Association Between Patient-Surgeon Sex Concordance and Total Health Care Costs, Further Including Operative Duration as a Covariate
Data Sharing Statement