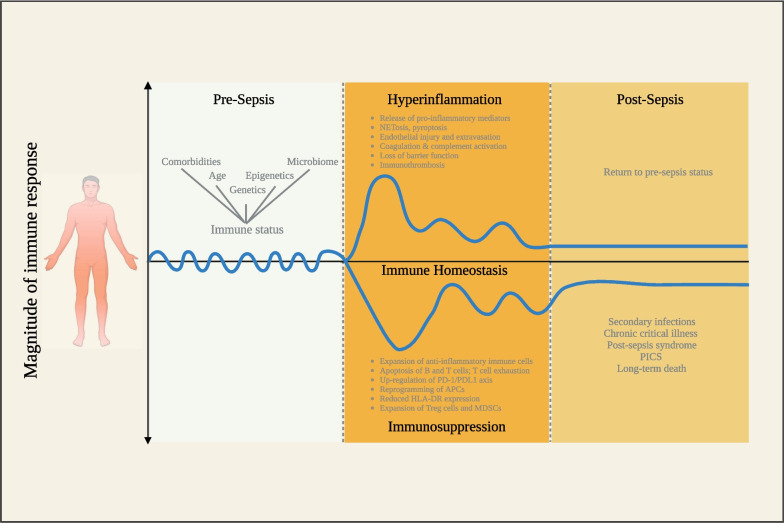
Fig. 1.
Model of sepsis-induced immune responses. This extended model of sepsis-induced immune responses describes the host inflammatory response before, during, and after sepsis. Infection modifies the innate and adaptive immune response for sustained periods of time, even long after clinical recovery. The immune response in sepsis is highly personalized and contingent upon the patient's immune status when infection occurs. This status is influenced by various factors including age, comorbidities, environmental elements, and the microbiome. Moreover, each patient exhibits a highly intricate combination of genetic variations and epigenetic alterations, rendering their immune system a virtually unique selection of genes responsible for cytokines and mediators that regulate immune responses. Excessive inflammation is triggered by the release of pro-inflammatory mediators by various cell types upon detecting pathogen-associated molecular patterns (PAMPs). Simultaneously, the activation of the complement system, the vascular endothelium, and the coagulation system results in microcirculatory disturbances. These processes are exacerbated by the release of damage-associated molecular patterns (DAMPs) as a consequence of tissue damage, the discharge of neutrophil extracellular traps (NETosis), and inflammatory cell death (pyroptosis). Immune suppression can develop at various time points and is characterized by the secretion of anti-inflammatory cytokines, the apoptosis of T cells, B cells, and dendritic cells, T cell exhaustion, and the proliferation of anti-inflammatory immune cells like regulatory T cells (Tregs) and myeloid-derived suppressor cells (MDSCs). Immune suppression is further intensified by decreased expression of human leukocyte antigen–antigen D related (HLA-DR) and heightened expression of programmed cell death 1 (PD-1) and its corresponding ligand (PD-L1). Post sepsis, the immune response can return to pre-sepsis status; however, many sepsis survivors later succumb to secondary infections, chronic critical illness, post-sepsis syndrome, and post-intensive care syndrome (PICS), severely impacting quality of life. A persistent sepsis-induced immune dysfunction can eventually lead to long-term death