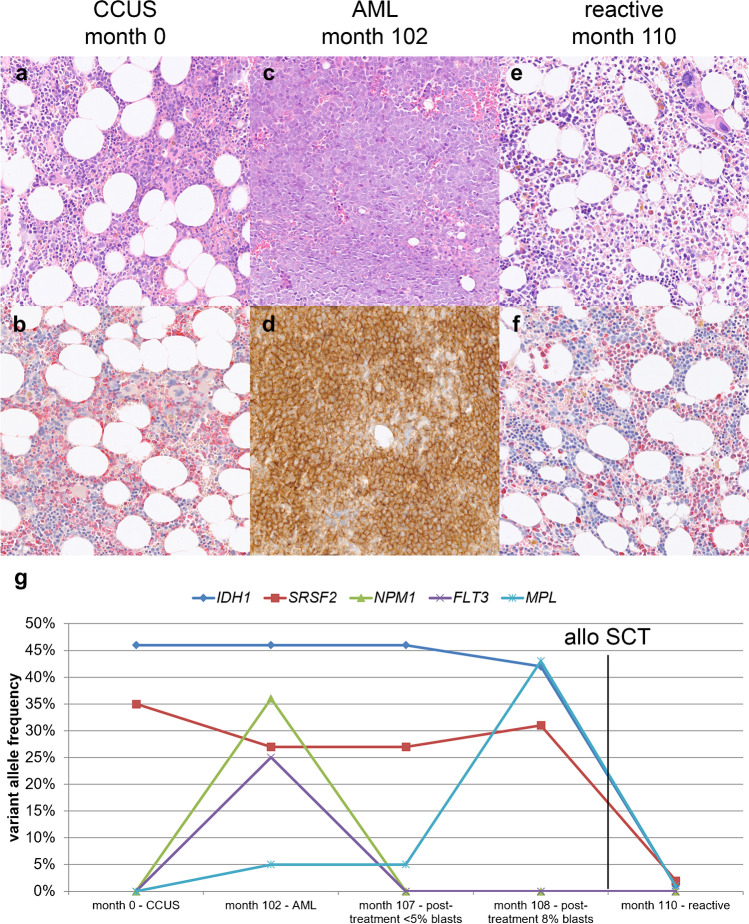
Fig. 4.
Morphology and genetic evolution of case A8. A 54-year-old woman with inconspicuous cytogenetics and reactive bone marrow (BM) at the first biopsy. One hundred and two months later, she was diagnosed with AML and after therapy the BM showed a blast count of <5% and 8%, respectively. After allo-SCT, there were no morphological residues of the AML, compatible with reactive changes. a, b Biopsy month 0; a normocellular BM biopsy with reactive changes, but without apparently dysplastic changes (hematoxylin and eosin (HE), 200× original magnification); b usual distribution of granulopoiesis and erythropoiesis demonstrated by naphthol-AS-D-chloroacetate esterase reaction (200×). c, d Biopsy month 102; c diffuse infiltrates by an acute myeloid leukemia with lots of blasts (HE, 200×) and positivity for CD33 (d CD33 immunoperoxidase, 200×). e, f Biopsy month 110; e normocellular BM biopsy with reactive changes with increased and left shifted erythropoiesis and left shifted granulopoiesis (HE, 200×), also demonstrated by naphthol-AS-D-chloroacetate esterase reaction (f 200×). g Variant allele frequencies (VAF) of mutations in consecutive biopsies. The first biopsy shows an IDH2 (VAF 46%) and a SRSF2 mutation (35%). The AML reveals additional mutations of NPM1 (36%), FLT3 (25%), and MPL (5%). After therapy, IDH2 and SRSF2 mutations do not decrease, but NPM1 and FLT3 cannot be detected anymore, only MPL remains. One month later, the MPL mutation increases to 43%. After allo-SCT, the three mutations in IDH2, SRSF2, and MPL are still detectable with low frequencies (1, 2, and 1%, respectively), demonstrating a small amount of residual mutated cells after transplantation