Abstract
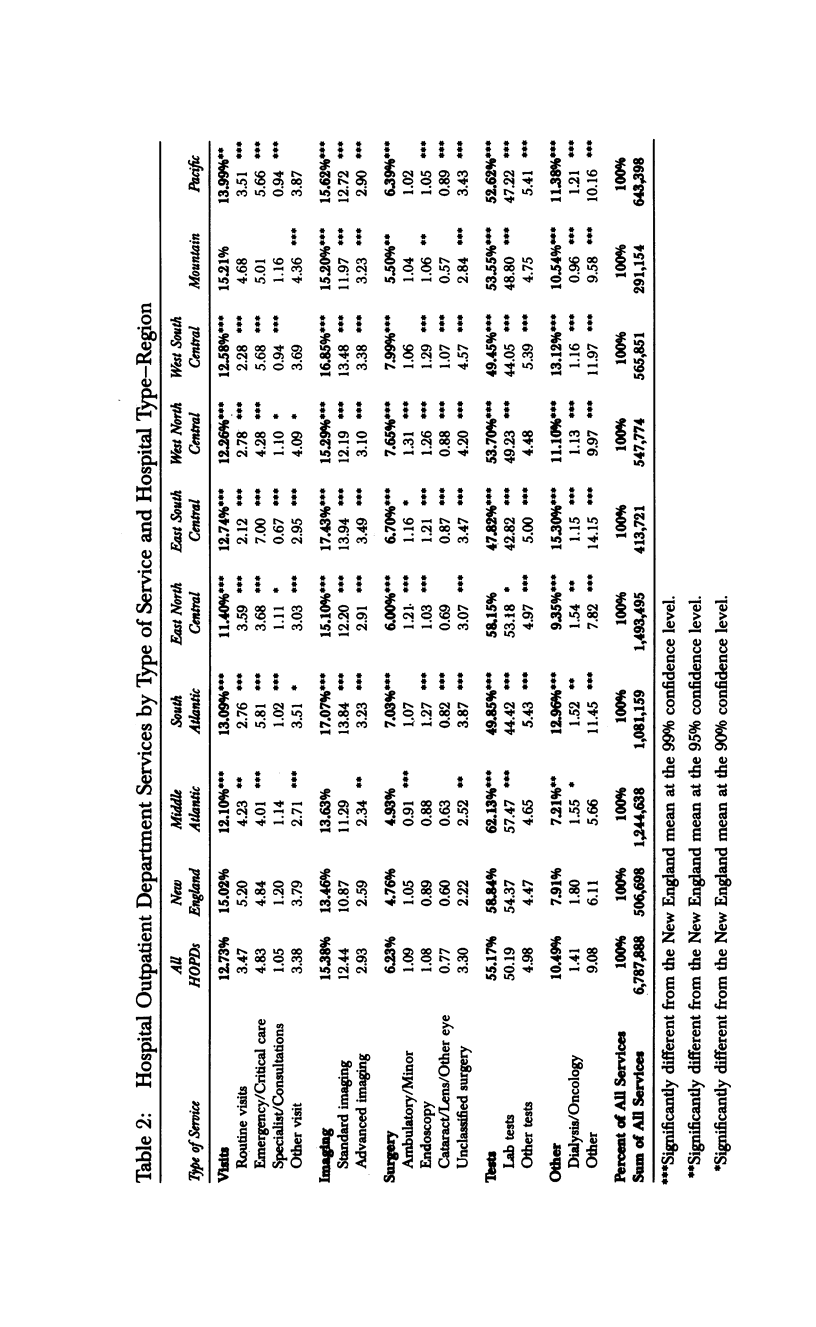
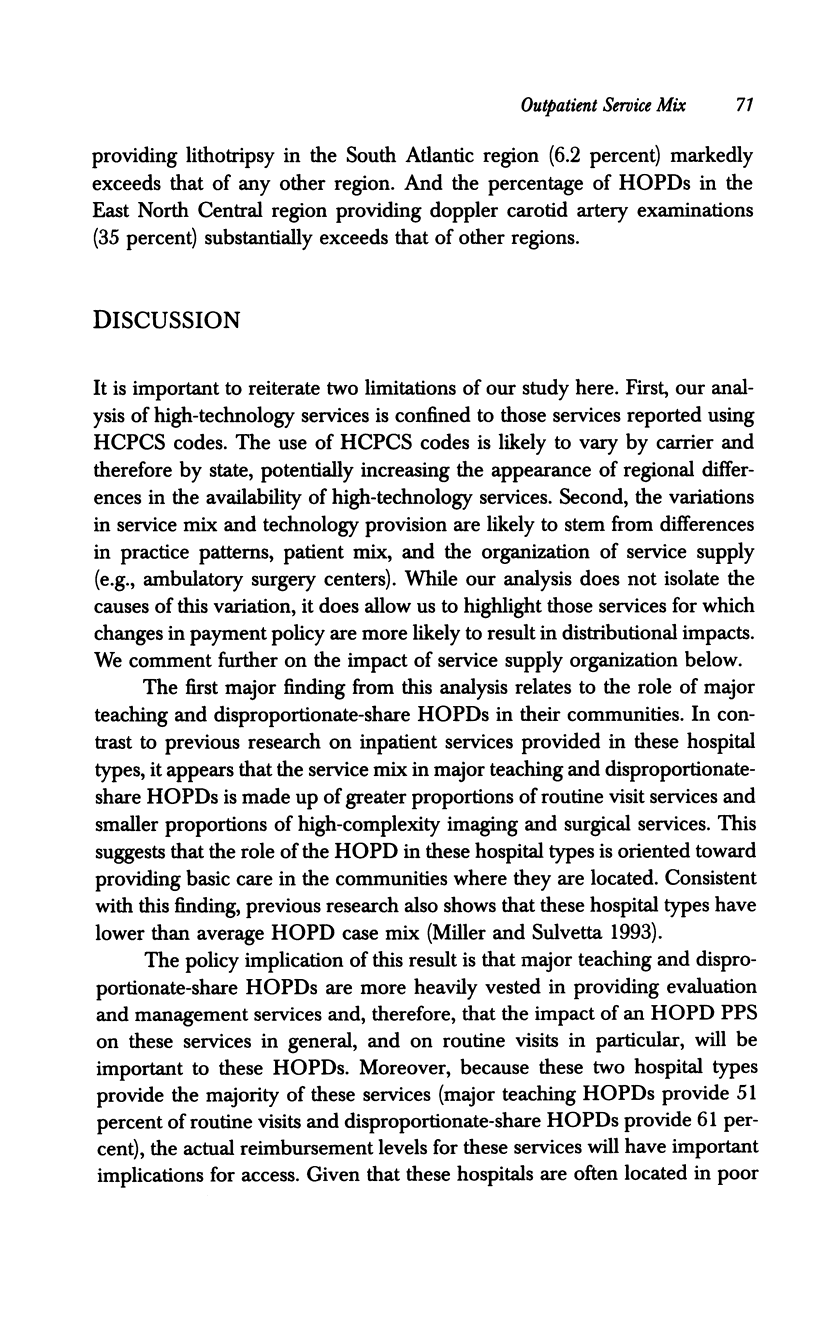
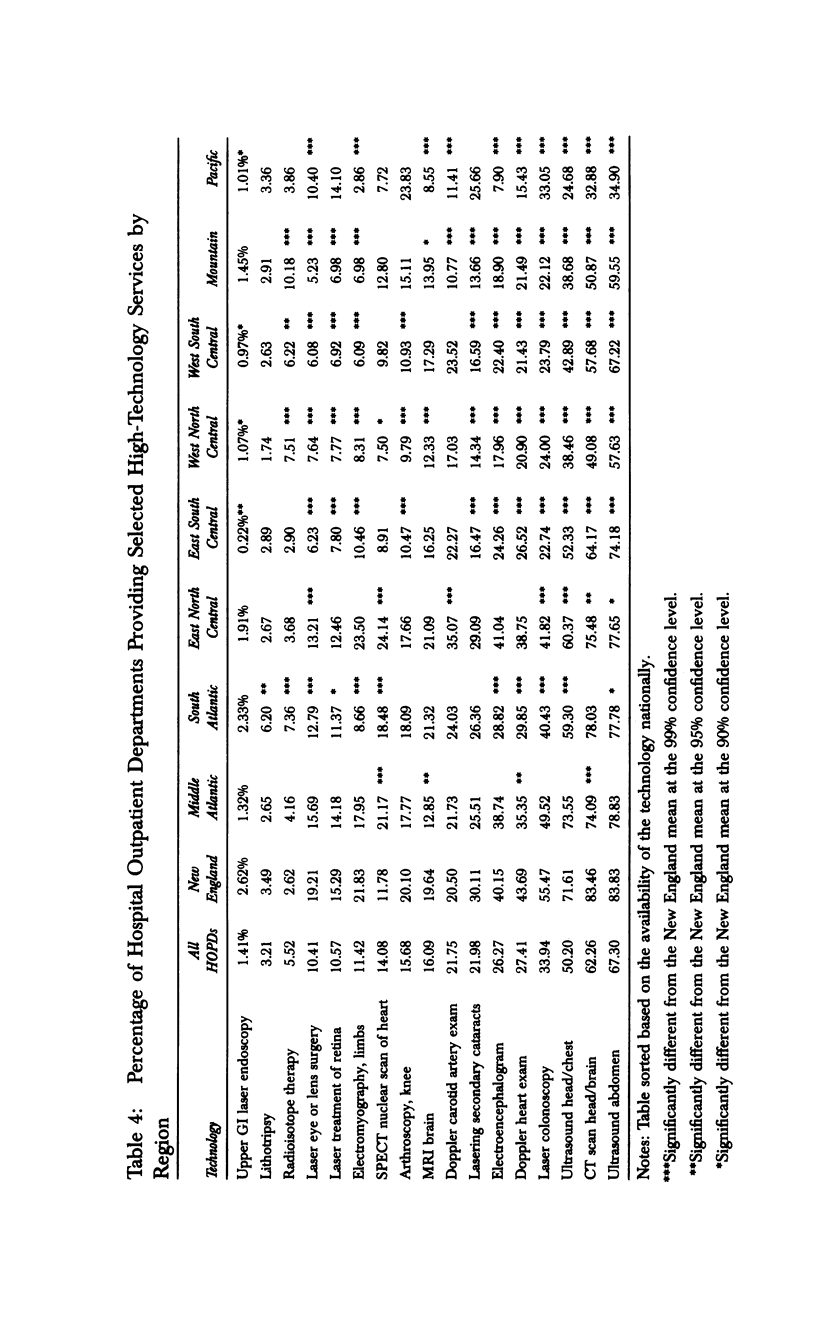
OBJECTIVE. To determine if implementation of a PPS for Medicare hospital outpatient department (HOPD) services will have distributional consequences across hospital types and regions, this analysis assesses variation in service mix and the provision of high-technology services in the HOPD. DATA. HCFA's 1990 claims file for a 5 percent random sample of Medicare beneficiaries using the HOPD was merged, by hospital provider number, with various HCFA hospital characteristic files. STUDY DESIGN. Hospital characteristics examined are urban/rural location, teaching status, disproportionate-share status, and bed size. Two analyses of HOPD services are presented: mix of services provided and the provision of high-technology services. The mix of services is measured by the percentage of services in each of 14 type-of-service categories (e.g., medical visits, advanced imaging services, diagnostic testing services). Technology provision is measured by the percentage of hospitals providing selected high-technology services. FINDINGS/CONCLUSIONS. The findings suggest that the role hospital types play in providing HOPD services warrants consideration in establishing a PPS. HOPDs in major teaching hospitals and hospitals serving a disproportionate share of the poor play an important role in providing routine visits. HOPDs in both major and minor teaching hospitals are important providers of high-technology services. Other findings have implications for the structure of an HOPD PPS as well. First, over half of the services provided in the HOPD are laboratory tests and HOPDs may have limited control over these services since they are often for patients referred from local physician offices. Second, service mix and technology provision vary markedly among regions, suggesting the need for a transition to prospective payment. Third, the organization of service supply in a region may affect service provision in the HOPD suggesting that an HOPD PPS needs to be coordinated with payment policies in competing sites of care (e.g., ambulatory surgical centers).
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berenson R., Holahan J. Sources of the growth in Medicare physician expenditures. JAMA. 1992 Feb 5;267(5):687–691. [PubMed] [Google Scholar]
- Miller M. E., Sulvetta M. B. Medicare hospital outpatient services and costs: implications for prospective payment. Health Care Financ Rev. 1992 Winter;14(2):135–149. [PMC free article] [PubMed] [Google Scholar]
- Sheingold S. H. Alternatives for using multivariate regression to adjust prospective payment rates. Health Care Financ Rev. 1990 Spring;11(3):31–41. [PMC free article] [PubMed] [Google Scholar]
- Sulvetta M. B. Achieving cost control in the hospital outpatient department. Health Care Financ Rev Annu Suppl. 1991:95–106. [PubMed] [Google Scholar]
- Wilensky G. R. Technology as culprit and benefactor. Q Rev Econ Bus. 1990 Winter;30(4):45–53. [PubMed] [Google Scholar]


