The number of immigrants and refugees from Asia and Africa to developed countries has increased in the past 20 years. Through caring for these patients, western physicians have become increasingly aware of traditional healing practices such as coining, cupping, and herbal therapies.1 Most physicians know little about traditional healing practices involving the mouth. We present 3 cases of dental malformations from care provided by traditional healers in East Africa (figures1,2, and3).
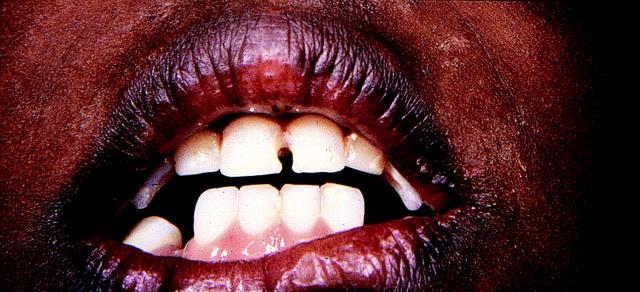
Figure 1.
On a routine physical examination, this 6-year-old Somali boy, a recent immigrant to the United States, was noted to be missing both primary lowercuspids.
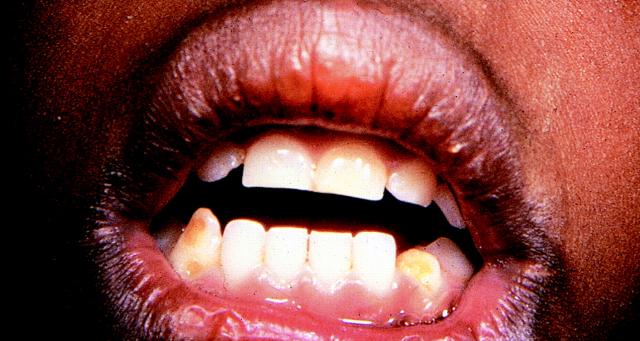
Figure 2.
A 7-year-old Somali boy (brother of boy infigure 1) was also noted on a routine physical examination to have enamel defects located centrally on the buccal surface of both lower cuspids. The right cuspid was broken off above the defect.
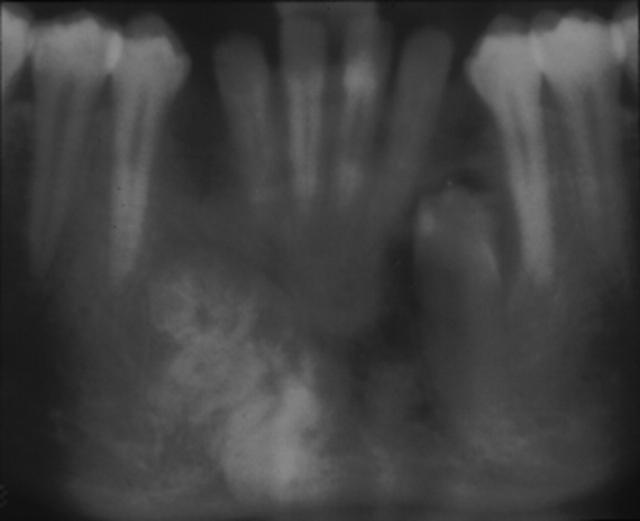
Figure 3.
A 16-year-old Somali boy, who had been in the United States for several years, was noted by his primary care dentist to be missing both permanent lower incisors.
REPORT OF CASES
The history in all 3 of the children indicated that traditional healers inSomalia had treated them when they were infants for the prevention or treatment of diarrhea. Patient 1's gums were cut into and the lower cuspids(the pointed teeth lateral to the 4 incisors) were extracted to prevent diarrhea. Patient 2 had a hot nail pressed into his gums in the area of the lower cuspids as treatment of an episode of gastroenteritis. The mother of both of these children also had absence of her permanent lower cuspids.Patient 3's mother reported that when he was between 4 and 6 months of age, a traditional healer made cuts in the area of the child's lower cuspids and removed gum tissue to prevent diarrhea. A Panorex film revealed absence of the right lower cuspid and the presence of a radiopaque mass, consistent with odontoma in that site. A deformed and impacted left lower cuspid with associated radiopaque structures was identified in the left mandible. An exploration was done and a biopsy specimen taken of these structures. Biopsy findings were consistent with an odontoma (a benign tumor) in the mandible at the expected site of the deformed permanent cuspid tooth bud on the right side. On the left side, an impacted and deformed permanent cuspid developed.Oral surgeons speculated that the odontoma formed as a result of the disruption of the dental tissues resulting from the traditional treatment.Both mothers reported that this was a common procedure in some regions ofSomalia.
EXTENT OF PRACTICE
Reports of traditional healing practices of many African countries in which the cuspids and incisors were removed or mutilated have been numerous: 1% to60% in certain villages inTanzania,2,3 16% in northernUganda,4 22% amongurban children inSudan,5 59% amongEthiopian Jews,6 70%in some populations inEthiopia,7 87% among the Maasai inKenya,8 and 100%among infants younger than 18 months admitted to a hospital in southernSudan.9 We were unable to find any reports of the practice among Somali populations.
All reports indicate that there are strong cultural beliefs that theswelling in the area of the gums associated with the unerupted cuspids is a cause of persistent fever and diarrhea. A traditional healer is consulted to remove or lance this area of the gums. In most instances, the lower cuspids are extracted bilaterally, but the extracting of upper cuspids and lower incisors has also been reported. Lancing of the un erupted cuspids with a hot needle has been reported in the Sudan and has been associated with enamel defects on the buccal surface of the lowercuspids.7Instruments used for these procedures include penknives, metal blades made from spoon handles or bike tire spokes, and sharp fingernails. In some cultures, salt or herbs are applied to the area of the gum that is injured following the procedure.2,5,10
The procedure is carried out by a traditional healer. In some cultures, the healer is a respected older woman.2 In others, it is a person, usually a man, who makes a living from this specific practice.11 The instruments used are often not sterilized, and no topical anesthesia is used.The procedure is performed to prevent or treat gastroenteritis and prolonged fever. One study fromTanzania5 in which parents were interviewed about the health behaviors that had occurred before the traditional treatment showed that parents often consulted a traditional healer after 1 or more visits to a government health facility. They resorted to the traditional treatment because their child's symptoms persisted despiteevaluation and receiving medication from a local hospital. The age at which the extractions and lancing occurred varied from as early as 1 month to 2 to 3years. Peak ages for the procedure in most studies were between 4 and 18months.2,3,4,5,7,8,11
CONSEQUENCE OF CUSPID DISRUPTION
Dental abnormalities are the primary consequence of the practice. In addition to enamel defects and loss of teeth, the mandibular arch size has been documented to be smaller in those who have had the extractions.12Partial extraction of the cuspids often results in hypoplasia of adjacent primary and permanent teeth. The retention of primary lateral incisors with distal eruption of permanent successors has also been noted, along with displacement and impaction of the permanent cuspid.4,9,10 The practice of removing or disrupting the primary cuspid tooth typically occurs before the eruption of the cuspid. The procedure is considered a success if the“tooth worm” is removed along with the primary cuspid. The toothworm is the dental lamina, the permanent cuspid before crown development. If the dental lamina is not removed, it may continue to develop normally, although it is more likely damaged, resulting in a dysplastic or maldeveloped permanent tooth.
Andreasen and Ravin list 10 possible outcomes of trauma to a primary tooth, including “odontoma-likemalformation.”13A true odontoma might result from the extraction of an unerupted cuspid, with concurrent damage to the dental lamina. A case of a small odontoma at the site of a mandibular canine extracted early in childhood by a traditional healer was recently reported in an Ethiopian teenager who now resides inSweden.14 More cases may be seen as these immigrant children receive dental care in developed countries.
The practice has other consequences. Infection at the site of the procedure and death from sepsis have been documented in a number of studies. Of 124infants who had the procedure in Tanzania, 10 died of infectious complications.15 In1 birth cohort in Ethiopia of 594 children who had the procedure and were observed for a year, 1 child died.16 The child had undergone a dual procedure involving uvulectomy and dental extraction, and the maternal history suggested that the child died of infectious complications. Why the mortality rate is so low is unclear, given that the instruments that are used are not routinely sterilized. Physicians working inAfrica report that traditional practitioners will do the procedure on several successive children in a short period of time using the same instrument. This practice is common in areas of Kenya, where nearly a third of the pregnantwomen are documented to be positive for the human immunodeficiency virus, suggesting a possible mechanism for the horizontal spread of the virus(Juliana Otieno, MD, International Fellow, New Nyanza Provincial Hospital,Kenya; oral communication; April 1999).
An Ethiopian study showed decreased growth in children who had dental extractions as long as 4 months after the extractions, and this reduction was observed even when controlling for illness episodes.16 Perhaps the most important consequence of this practice is that the children are not correctly diagnosed or treated for their febrile or gastrointestinal illnesses because parents either do not return to western facilities or seek care directly from a traditional healer.
Public health interventions have been attempted to modify the adverse effects of this practice. In the early 1980s, a health campaign was carried out in Tanzania urging people not to do the procedure, and it was outlawed. A survey in 1992, however, indicated that the procedure was still prevalent in many regions of the country.5 In some areas, the practice has changed from these harmful extractions to rubbing medicinal herbs on the gums. In Kenya, attempts have been made to train traditional practitioners to recognize signs of dehydration and sepsis in children and to provide them with oral rehydration solution (J Otieno, oral communication, April 1999). There have been no reports on the outcome of these public health efforts. Parents we have spoken with from Somalia indicate that the procedure is a source of income for the traditional healers and has become deeply ingrained in the society because of the strong folk belief in its efficacy.
HISTORY OF PROCEDURE
The historical origins of the procedure are not clear. Several authors and our conversations with local East African health outreach workers suggest that this procedure is relatively new in Africa. The first reports of the procedure were from the 1930s and were described in the Nuer tribe in Africa. In Kenya, the procedure was thought to have started among the Maasai in the 1960s and to have spread from neighboring Uganda andTanzania.2 In southern Sudan, the practice is thought to have been brought in by refugees from neighboring countries.7 Our adult dental clinic rarely sees absent cuspids in East African older adults, which suggests that the practice has been prevalent among our refugee population only for the past 30 to 40 years.
Incising the gum over an erupting tooth was promoted in Europe as early as1742 by Joseph Hurlock as a means of decreasing pain associated with eruption.17 The practice was continued into this century in Europe and the United States and may have been used by colonial dentists in East Africa and adopted by traditional healers to treat fever and diarrhea.
Virtually all cultures have specific beliefs associating common childhood illnesses with tooth eruption.18,19,20,21Given the high morbidity and mortality associated with childhood gastroenteritis and febrile conditions in developing countries, it is not surprising that parents associate these illnesses with teething and subject their children to traumatic procedures in the hope of preventing and treating such feared conditions. Educating parents and traditional healers and instituting public health measures to provide clean water supplies and sanitation are needed before these harmful traditional healing practices will cease.
Competing interests: None declared.
References
- 1.Dinulos JG, Graham EA. Influence of culture and pigment on skin conditions in children. Pediatr Rev 1998;19:268-275. [DOI] [PubMed] [Google Scholar]
- 2.Kikwilu EN, Hiza JF. Tooth bud extraction and rubbing of herbs by traditional healers in Tanzania: prevalence, and sociological and environmental factors influencing the practices. Int J PaediatrDent 1997;7:19-24. [DOI] [PubMed] [Google Scholar]
- 3.Hiza JF, Kikwilu EN. Missing primary teeth due to tooth bud extraction in a remote village in Tanzania. Int J PaediatrDent 1992;2:31-34. [DOI] [PubMed] [Google Scholar]
- 4.Pindborg JJ. Dental mutilation and associated abnormalities inUganda. Am J Phys Anthropol 1969;31:383-390. [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen P, Elhassan E, Raadal M. Enamel defects in primarycanines related to traditional treatment of teething problems in Sudan.Int J Paediatr Dent 1992;2:151-155. [DOI] [PubMed] [Google Scholar]
- 6.Holan G, Mamber E. Extraction of primary canine tooth buds: prevalence and associated dental abnormalities in a group of Ethiopian Jewish children. Int J Paediatr Dent 1994;4:25-30. [DOI] [PubMed] [Google Scholar]
- 7.Dagnew MB, Damena M. Traditional child health practices in communities in northwest Ethiopia. Trop Doct 1990;20:40-41. [DOI] [PubMed] [Google Scholar]
- 8.Hassanali J, Amwayi P, Muriithi A. Removal of deciduous canine tooth buds in Kenyan rural Maasai. East Afr Med J 1995;72:207-209. [PubMed] [Google Scholar]
- 9.Baba SP, Kay EJ. The mythology of the killer deciduous canine tooth in southern Sudan. J Pedod 1989;14:48-49. [PubMed] [Google Scholar]
- 10.Welbury RR, Nunn JH, Gordon PH, Green-Abate C. “Killer”canine removal and its sequelae in Addis Ababa. QuintessenceInt 1993;24:323-327. [PubMed] [Google Scholar]
- 11.Halestrap DJ. Indigenous dental practice in Uganda. BrDent J 1971;131:463-466. [DOI] [PubMed] [Google Scholar]
- 12.Hassanali J, Amwayi P. Biometric analysis of the dental casts ofMaasai following traditional extraction of mandibular permanent central incisors and of Kikuyu children. Eur J Orthod 1993;15:513-518. [DOI] [PubMed] [Google Scholar]
- 13.Andreasen JO, Ravin JJ. Enamel changes in permanent teeth after trauma to their primary predecessors. Scand J Dent Res 1973;81:203-209. [DOI] [PubMed] [Google Scholar]
- 14.Erlandsson AL, Backman B. A case of dental mutilation.ASDC J Dent Child 1999;66: 278-279,229. [PubMed] [Google Scholar]
- 15.Mosha H. Dental mutilation and associated abnormalities inTanzania. Odontostomatol Trop 1983;6:215-219. [PubMed] [Google Scholar]
- 16.Asefa M, Hewison J, Drewett R. Traditional nutritional and surgical practices and their effects on the growth of infants in south-west Ethiopia.Paediatr Perinat Epidemiol 1998;12:182-198. [DOI] [PubMed] [Google Scholar]
- 17.Kowitz AA, Loevy HT. Paediatric dentistry: Fauchard and before.Int Dent J 1993;43:239-244. [PubMed] [Google Scholar]
- 18.Zoysa I, Carson D, Feachem R, Kirkwood B, Lindsay-Smith E,Loewenson R. Perceptions of childhood diarrhoea and its treatment in ruralZimbabwe. Soc Sci Med 1984;19:727-734. [DOI] [PubMed] [Google Scholar]
- 19.Adentunji JA. Response of parents to five killer diseases among children in a Yoruba community, Nigeria. Soc Sci Med 1991;32:1379-1387. [DOI] [PubMed] [Google Scholar]
- 20.Gibbons HL, Hebdon CK. Teething as a cause of death: a historical review. West J Med 1991;155:658-659. [PMC free article] [PubMed] [Google Scholar]
- 21.Oyejide CO, Aderinokun GA. Teething myths in Nigerian rural Yoruba communities. Afr Dent J 1991;5:31-34. [PubMed] [Google Scholar]