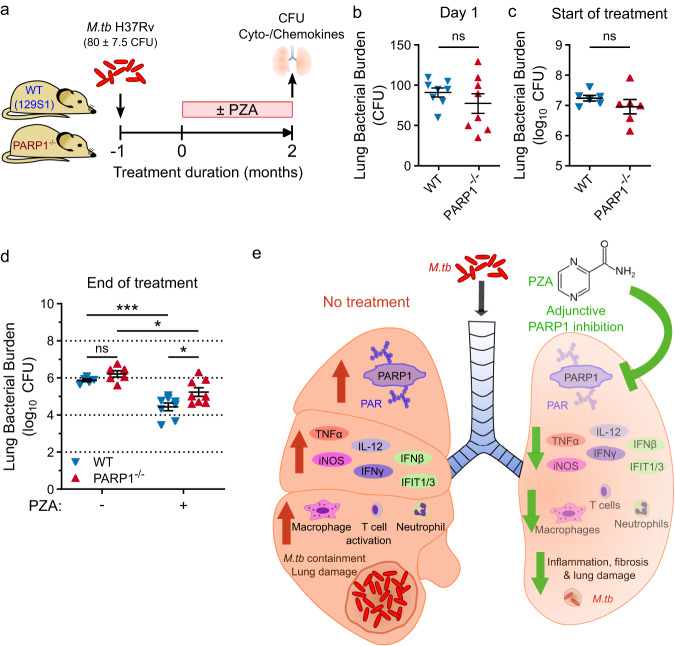
Fig. 6. PZA has reduced efficacy in PARP1−/− mice.
a Study outline to compare the efficacy of PZA in WT and PARP1−/− mice. Male and female PARP1-null (PARP1−/−) or 129S1 (WT) mice were aerosols infected with M.tb H37Rv (implantation: 80 ± 7.5 CFU). Starting one month after infection, half of the mice were administered PZA (150 mg/kg) 5 days/week for 2 months. Lung bacterial burden was assessed at the beginning and end of treatment. b–d Lung bacterial burden on the day after infection (b; n = 8), at the start of treatment (c; n = 6), and in untreated (−) or PZA-treated (+) mice at the end of treatment (d; n = 5 (untreated WT), 6 (untreated PARP1−/−) or 8 (PZA-treated)). Each symbol represents an individual mouse, with mean ± SEM indicated. Statistical differences between groups were determined by two-tailed unpaired t-test (b, c) or two-way ANOVA with Šidák’s multiple comparisons test (d). *p = 0.0135 (PARP1−/− untreated vs. PZA) or 0.0361 (PZA: WT vs. PARP1−/−); ***p = 0.0005; ns not significant. After 2 months of PZA treatment, significantly more bacilli remained in the lungs of PARP1−/− than of WT mice (5.234 vs. 4.437 log10 CFU, respectively). e Proposed model: PARP1 inhibition is a key component of PZA’s mechanism of action in TB therapy. Without treatment (left), M.tb infection activates PARP1 which promotes the production of inflammatory mediators, immune cell activation and M.tb containment at the cost of lung damage. Inhibiting PARP1 during TB therapy (right), by PZA or adjunctive PARP inhibition, can accelerate bacterial clearance and the resolution of lung damage while dampening inflammation. However, PARP1 inhibition without adequate antibiotics may impair bacterial containment. Source data are provided as a Source Data file.