Abstract
Aim
The first expert consensus documents on management of patients with spontaneous coronary artery dissection (SCAD) were published in 2018. Worldwide quality of care, as measured by adherence to these recommendations, has not been systematically reviewed. We aim to review the proportion of patients with SCAD receiving consensus recommendations globally, regionally and, determine differences in practice before and after 2018.
Methods and results
A systematic review was performed by searching four main databases (Medline, Embase, SCOPUS, CINAHL) from their inception to 16 June 2022. Studies were selected if they included patients with SCAD and reported at least one of the consensus document recommendations. 53 studies, n=8456 patients (mean 50.1 years, 90.6% female) were included. On random effects meta-analysis, 92.1% (95% CI 89.3 to 94.8) received at least one antiplatelet, 78.0% (CI 73.5 to 82.4) received beta-blockers, 58.7% (CI 52.3 to 65.1) received ACE inhibitors or aldosterone receptor blockers (ACEIs/ARBs), 54.4% (CI 45.4 to 63.5) were screened for fibromuscular dysplasia (FMD), and 70.2% (CI 60.8 to 79.5) were referred to cardiac rehabilitation. Except for cardiac rehabilitation referral and use of ACEIs/ARBs, there was significant heterogeneity in all other quality-of-care parameters, across geographical regions. No significant difference was observed in adherence to recommendations in studies published before and after 2018, except for lower cardiac rehabilitation referrals after 2018 (test of heterogeneity, p=0.012).
Conclusion
There are significant variations globally in the management of patients with SCAD, particularly in FMD screening. Raising awareness about consensus recommendations and further prospective evidence about their effect on outcomes may help improve the quality of care for these patients.
Keywords: Acute Coronary Syndrome, Cardiac Rehabilitation, Coronary Artery Disease
WHAT IS ALREADY KNOWN ON THIS TOPIC
Consensus documents recommended five main interventions for patients with spontaneous coronary artery dissection (SCAD): (1) at least one antiplatelet agent, (2) beta-blocker, (3) ACE inhibitor or aldosterone receptor blocker for patient with left ventricular systolic dysfunction, (4) screening for fibromuscular dysplasia (FMD) and (5) cardiac rehabilitation.
WHAT THIS STUDY ADDS
This study provides a systematic review of the current practice in managing patients with SCAD worldwide. It identifies low adherence and likely under-reporting of FMD screening and cardiac rehabilitation.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Raising awareness among clinicians about these recommendations may help improve the quality of care for these patients.
Introduction
Spontaneous coronary artery dissection (SCAD) is an important cause of myocardial infarction (MI), especially in young women.1 2 Once thought to be a rare condition, SCAD has been reported to be the cause of up to 4% of all acute coronary syndrome (ACS)3 and up to 35% of ACS among women less than 50 years of age.4 5 Despite its significance, our understanding about this potentially life-threatening condition remains incomplete. No randomised data have been published to guide treatment for SCAD, and clinicians have largely relied on standard ACS guidelines. This was not ideal as these guidelines are for atherosclerotic ACS.1
In 2018, the American Heart Association and the European Society of Cardiology published the world-first scientific statements on the management of SCAD.1 2 The recommendations of these documents were based on data from mostly observational studies and, where no data were available, expert opinions. Although there are some minor variations with regards to the use of antiplatelets, the consensus recommendations for SCAD treatment are similar and can be summarised as follows: (1) at least one antiplatelet agent, (2) beta-blocker, (3) ACE inhibitor (ACEI) or an angiotensin receptor blocker (ARB) in the presence of left ventricular (LV) systolic dysfunction, (4) referral to cardiac rehabilitation and (5) screening for fibromuscular dysplasia (FMD). So far, there have been no data about the effects of these treatments on major adverse cardiovascular events (MACE). The use of beta-blockers was found to be associated with lower risks of SCAD recurrence in a recent systematic review and meta-analysis.6 As the use of antiplatelets, beta-blockers, ACEI or ARB, and cardiac rehabilitation was also present in guidelines for atherosclerotic ACS, it is worth highlighting the following differences in SCAD consensus recommendations compared with atherosclerotic ACS guidelines: (1) optimal time for antiplatelet therapy was not defined in SCAD and dual-antiplatelets therapy was only recommended if coronary stents were used, (2) ACEIs or ARBs were only recommended in patients with impaired LV systolic function, (3) statins were not recommended in patients with SCAD, and (4) FMD screening was specific for patients with SCAD only and was not recommended in patients with atherosclerotic ACS.
Since the publication of these consensus recommendations, there has been no evaluation of the international implementation of these recommendations. Current optimal quality of care for patients with SCAD around the world is based on the proportion of patients who receive consensus-recommended treatment. The primary aim of this systematic review was to evaluate the quality of care of patients with SCAD, as measured by adherence to global consensus recommendations. Secondary aims included the time from symptom onset to angiography or revascularisation, comparison of adherence to recommendations between geographic regions and before versus after 2018 (the year when the positional papers were published). In addition, for patients presenting with acute MI (AMI), the time from presentation to angiography or revascularisation is an important marker of quality of care, irrespective of the diagnosis of SCAD. As patients with SCAD are often young and without traditional cardiovascular risk factors,7 we hypothesised that this time would be longer compared with patients with atherosclerotic MI.
Method
This systematic review complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statements.8 Ethics approval was not required as only data from published literature was used. This systematic review was registered with the international prospective register of systematic reviews (PROSPERO), ID number CRD42022363414.
Search strategy
A search strategy was developed with a university librarian and performed using the following databases: Medline, Embase, SCOPUS and CINAHL, from their inception up to 16 June 2022. The search was restricted to literature published in English only and using the following search terms: ‘spontaneous coronary artery dissection’ and ‘spontaneous coronary dissection’. The full search strategy can be viewed in online supplemental table 1.
openhrt-2023-002379supp001.pdf (78.9KB, pdf)
Study selection
To be included in the systematic review, studies either had to be an original cohort or original case series on consecutive patients diagnosed with SCAD and, report at least one of the quality-of-care parameters: that is, proportion of patients prescribed with antiplatelets, beta-blockers, ACEIs or ARBs (in the presence of LV systolic dysfunction) during index hospital admission or at the time of discharge, the proportion of patients screened for FMD, the proportion of patients referred to cardiac rehabilitation and, the time from symptom onset to coronary angiography or revascularisation (where appropriate). The sample size had to be more than 10 patients. Case reports, reviews including systematic reviews, editorials and comments, studies not in English and grey literature (eg, conference abstracts) were excluded.
Screening and data extraction
Literature screening using Covidence software (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org) was performed by two pairs of investigators (QD-FO and QD-BS) independently, using the inclusion and exclusion criteria as defined above. An investigator (QD) performed data extraction while another coauthor (FO/BS/SZ/RZ) checked for consistency. For each study included the following parameters were extracted: author name, year of publication, country of study, site of study, city of study, study name, study aim, type of ACS, sample size, parent SCAD cohort or registry, mean or median age, proportion of female, study design, data collection time, baseline comorbidities, quality of care parameters (the proportion of patients receiving antiplatelets, beta-blockers, ACEIs/ARBs, cardiac rehabilitation, FMD screening, time to angiogram/revascularisation), in-hospital and follow-up MACE (cardiovascular death, MI and stroke) and median or mean follow-up time. With regards to FMD screening, current guidelines recommended CT angiography or magnetic resonance angiography from brain to pelvis. We defined the parameter of FMD screening as having either complete or partial screening.
Included studies were evaluated independently by two investigators for bias using the Newcastle-Ottawa Scale (NOS), a scoring system to evaluate the quality of non-randomised studies in meta-analysis. The NOS scores studies in three domains, with higher scores mean higher quality thus lower risk of bias. The three domains of the NOS are: (1) selection, with a maximum of four points, (2) comparability, with a maximum of two points, and (3) exposure, with a maximum of three points. Included studies were classified based on their total NOS score: low risk for total score 7–9, medium risk for total score 4–6 and high risk for total score 0–3.
If there were multiple papers based on the same cohort (or registries) of SCAD patients, to avoid duplication, only the most recent publication and/or with the highest number of patients that reported the quality-of-care parameters was included in the meta-analysis. Although not included in the meta-analysis, multiple papers from the same cohort of patients offered an opportunity to assess how quality-of-care parameters for the same cohort changed with time. These studies were presented and discussed separately. If a study had a quality-of-care criterion as a selection requirement (e.g., a study on patients with SCAD who were screened for FMD), data for that criterion were not collected. At any stage of the screening and data extraction process, disagreements between two investigators were resolved by discussion and consensus, with the involvement of a third investigator (SZ) where required.
Statistical analysis
Descriptive statistics were reported using weighted means and SD. Random effects meta-analysis was used to estimate each quality-of-care parameter, reporting mean percentages and 95% CIs. The differences in these parameters across geographical regions and before and after 2018 were assessed using univariate metaregression. Heterogeneity was analysed using Cochran’s Q test, which tests whether the variability in the observed effect sizes is larger than would be expected based on sampling variability alone. All analysis was conducted in R (R Foundation for Statistical Computing, Vienna, Austria), using the rma function in the metafor package.
Results
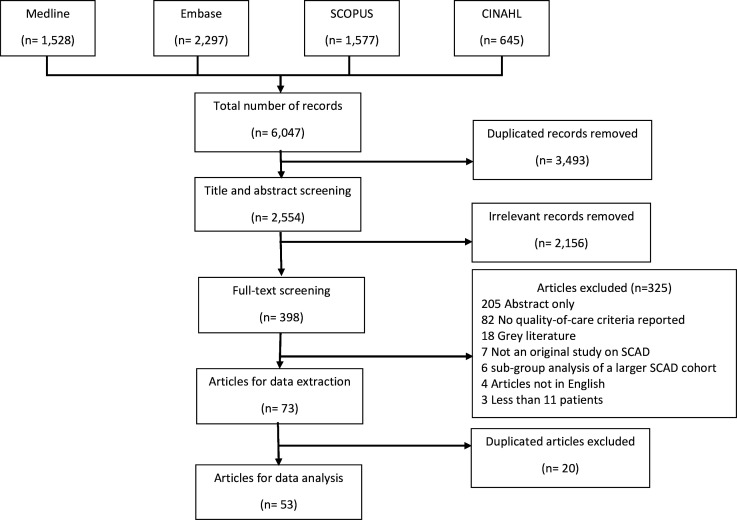
The PRISMA flow chart is presented in figure 1. In total, 2554 articles were screened, and 398 articles were identified for full-text screening. From these, 325 articles were excluded (figure 1). From the remaining 73 articles, 29 were identified to have clear or potential duplicated data from the same cohorts/registries of patients (table 1), with the most appropriate study selected for inclusion. In total, 53 articles, published between 1989 and 2022, were included, with characteristics of the included studies shown in table 2. Overall, n=8456 individuals with SCAD were analysed, mean age 50.1, 90.6% female. Studies were performed in 22 countries which were grouped into 6 geographical regions: Europe, North America, Oceania, East Asia, Middle East and South Asia. Europe had the highest number of studies (20 studies) while North American studies included the highest number of patients (4401). Medical therapy was reported in 39 studies, FMD screening in 24 and cardiac rehabilitation in 3 studies. On assessment of the included studies for risk of bias using NOS, 21 studies were classified as low risk, 28 as medium risk, and 4 as high risk (online supplemental table 2).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow chart. SCAD, spontaneous coronary artery dissection.
Table 1.
Studies excluded due to data duplication
| Potentially duplicated studies | Common cohort | Selected study | Reason of selection |
| Daoulah et al, 202016 Daoulah et al, 202117 Daoulah et al, 202118 Daoulah et al, 202119 Daoulah et al, 202120 |
Gulf SCAD Registry | Daoulah et al, 202120 | Latest study |
| Saw et al, 201421 Saw et al, 201722 Saw et al, 201923 |
Canadian SCAD Registry | Saw et al, 201923 | Latest study with highest number of patients |
| Combaret et al, 202124 Combaret et al, 202225 |
French DISCO Registry | Combaret et al, 202124 | Highest number of patients (2022 study a subgroup of the registry) |
| Alfonso et al, 202226 Diez-Villanueva et al, 202127 Diez-Villanueva et al, 202128 Garcia-Guimaraes et al, 202129 Garcia-Guimaraes et al, 202230 |
Spanish Registry on SCAD | Garcia-Guimaraes et al, 202230 | Latest study with highest number of patients |
| Macaya et al, 201931 Carss et al, 202032 |
UK SCAD Registry | Carss et al, 202032 | Latest study with highest number of patients |
| Rogowski et al, 201733 Seidl et al, 202134 |
Kantonsspital St. Gallen cohort | Seidl et al, 202134 | Latest study with highest number of patients |
| Chen et al, 201935 Chen et al, 202136 |
Kaiser Permanente Northern California cohort | Chen et al, 202136 | Latest study with highest number of patients |
| Kok et al, 201837 Johnson et al, 202238 |
Mayo Clinic Virtual SCAD Registry | Johnson et al, 202238 | Latest study with highest number of patients |
| Eleid et al, 201439 Krittanawong et al, 201640 Tweet et al, 201441 Tweet et al, 201742 Tweet et al, 202043 Turley et al, 202044 |
Mayo Clinic SCAD Registry | Turley et al, 202044 | Latest study with highest number of patients |
DISCO, DIssezioni Spontanee COronariche; SCAD, spontaneous coronary artery dissection.
Table 2.
Characteristics of included studies
| Author | Year | Sample size | Mean or median age | Female percentage | Quality-of-care parameters reported | |||||
| Antiplatelets | Beta-blocker | ACEIs/ARBs | FMD screening | Cardiac rehabilitation | Time to angiogram | |||||
| Daoulah et al20 | 2021 | 83 | 44 | 50.6 | 98.8 | 89.2 | 65.1 | 0 | ND | ND |
| McGrath-Cadell et al45 | 2016 | 40 | 45 | 95 | ND | ND | ND | 47.5 | ND | ND |
| Rashid et al46 | 2016 | 21 | 53.3 | 95.2 | 100 | 76.2 | 80.9 | 52.4 | ND | ND |
| Adams et al47 | 2018 | 22 | 48.7 | 77.3 | 100 | 72.7 | 72.7 | ND | ND | ND |
| Tarr et al48 | 2022 | 91 | 45.4 | 91.2 | ND | ND | ND | 47.3 | ND | ND |
| Chou et al49 | 2016 | 70 | 52.3 | 100 | 95.7 | 85.7 | 48.6 | ND | ND | ND |
| Bouchard et al50 | 2021 | 15 | 47.5 | 86.7 | ND | 100 | ND | ND | ND | ND |
| Inohara et al51 | 2021 | 346 | 53.7 | 90.2 | 93.6 | 86.4 | 63.6 | ND | ND | ND |
| Solomonica et al52 | 2020 | 16 | 52.3 | 93.7 | 25 | 25 | 18.8 | ND | ND | ND |
| Saw et al23 | 2019 | 750 | 51.8 | 88.5 | 93.7 | 84.8 | 57.4 | 73.3 | ND | ND |
| Sun et al53 | 2019 | 85 | 55 | 17.6 | 92.9 | 68.2 | 67.1 | ND | ND | ND |
| Hui et al54 | 2020 | 70 | 50.8 | 74.3 | ND | ND | ND | 74.3 | ND | ND |
| Chang et al10 | 2022 | 30 | 51.8 | 66.7 | 90 | 66.7 | 76.7 | ND | ND | 7 days |
| Mortensen et al55 | 2009 | 22 | 48.7 | 81 | 100 | 100 | ND | ND | ND | ND |
| Combaret et al24 | 2021 | 373 | 51.5 | 90.6 | 88.3 | ND | ND | 74.3 | ND | ND |
| Panneerselvam et al56 | 2017 | 64 | 53.8 | 6.3 | 98.4 | 79.7 | 81.3 | ND | ND | ND |
| Almasi et al57 | 2022 | 15 | 48.2 | 100 | 92.2 | 71.4 | 64.3 | ND | ND | ND |
| Lettieri et al58 | 2015 | 134 | 52 | 81 | 87.3 | ND | ND | ND | ND | ND |
| Antonutti et al59 | 2021 | 70 | 47 | 86 | 100 | 81 | 55 | ND | ND | ND |
| Solinas et al60 | 2022 | 58 | 54 | 86 | 100 | 95 | 78 | 31 | ND | ND |
| Cerrato et al61 | 2021 | 199 | 52.3 | 88.9 | ND | 78.9 | ND | ND | ND | ND |
| Nakashima et al5 | 2016 | 63 | 46 | 94 | ND | ND | ND | 39.7 | ND | ND |
| Nishiguchi et al62 | 2017 | 12 | 63.1 | 58 | 100 | 33 | 75 | ND | ND | ND |
| Inohara et al63 | 2020 | 322 | 52.8 | 100 | 89.1 | 62.1 | 49.4 | ND | ND | ND |
| Inoue et al64 | 2021 | 19 | 48.7 | 100 | 94.7 | ND | ND | ND | ND | ND |
| Kim et al65 | 2021 | 13 | 52.1 | 100 | 53.8 | 69.2 | 76.9 | ND | ND | ND |
| McAlister et al66 | 2021 | 113 | 54 | 88 | 99 | 73 | 42 | ND | ND | ND |
| Romero-Rodriguez et al67 | 2010 | 19 | 47.7 | 79 | 100 | 100 | 100 | ND | ND | ND |
| Alfonso et al9 | 2012 | 17 | 48 | 82 | ND | ND | ND | ND | ND | 1 day |
| Alfonso et al68 | 2012 | 45 | 53 | 58 | 100 | 80 | 53.3 | ND | ND | ND |
| Camacho Freire et al69 | 2019 | 73 | 55 | 77 | 90 | ND | ND | ND | ND | ND |
| Bastante70 | 2020 | 37 | 56 | 97 | 94 | 85 | 64 | 88 | ND | ND |
| Macaya et al71 | 2020 | 78 | 53.2 | 85.9 | 94.8 | 80.5 | ND | 53.8 | ND | ND |
| Mori et al72 | 2020 | 23 | 52.4 | 95.7 | 65.2 | 69.6 | 65.2 | ND | ND | ND |
| Garcia-Guimaraes et al30 | 2022 | 389 | 53 | 88 | 93 | 80 | 51 | 27 | ND | ND |
| Murugiah et al11 | 2022 | 67 | 44.5 | 92.5 | 100 | 83.6 | 52.2 | ND | ND | 142 min |
| Wilander et al73 | 2022 | 147 | 52.9 | 75.5 | 93.1 | 81.9 | 59.2 | ND | ND | ND |
| Seidl et al34 | 2021 | 105 | 53.4 | 93 | 97 | 80 | 42 | 38.1 | ND | ND |
| Smaardijk et al74 | 2020 | 172 | 52 | 100 | ND | ND | ND | 75.6 | ND | ND |
| Carss et al32 | 2020 | 384 | 46.89 | 94.27 | ND | ND | ND | 60.4 | ND | ND |
| Androulakis et al75 | 2022 | 144 | 49 | 87.5 | ND | ND | ND | 52.1 | ND | ND |
| Kotecha et al76 | 2021 | 436 | ND | 93.1 | 95.2 | 83 | 69.7 | ND | ND | ND |
| De Maio Jr et al77 | 1989 | 11 | 43.1 | 54.5 | 36.4 | 27.3 | 10.1 | ND | ND | ND |
| Liang et al15 | 2014 | 158 | 45.2 | 97 | 86 | 62 | 30 | ND | 77 | ND |
| Wagers et al14 | 2018 | 367 | 44.55 | 100 | ND | ND | ND | ND | 72 | ND |
| Clare et al78 | 2019 | 208 | 49 | 88.9 | 70.2 | 83.2 | 57.2 | 43.3 | ND | ND |
| Sharma et al79 | 2019 | 113 | 47 | 87% | ND | ND | ND | 30 | ND | ND |
| McNair et al12 | 2020 | 51 | 46.9 | 100 | ND | ND | ND | 98 | ND | ND |
| Turley et al44 | 2020 | 667 | 46.7 | 100 | ND | ND | ND | 68.1 | ND | ND |
| Chen et al36 | 2021 | 307 | 49.9 | 100 | 94.1 | 84 | 59.3 | 50 | ND | ND |
| Baechler et al13 | 2022 | 115 | 55 | 97 | 88 | 72 | 43 | 41 | 60 | |
| Johnson et al38 | 2022 | 1196 | 54 | 95.6 | ND | ND | ND | 68.8 | ND | ND |
| White Solaru et al80 | 2019 | 11 | 47 | ND | ND | ND | ND | 72.7 | ND | ND |
ND, no data
Study inclusion and MACE outcomes
Table 3 provides the baseline characteristics of the included studies. Before 2018, there were only 15 studies (n=1065), compared with 39 studies (n=7509) after 2018. The majority of included studies were retrospective (28), followed by prospective (12), cross-sectional (10) and mixed-method (4) studies.
Table 3.
Baseline statistics of included studies
| Total number of patients, n | 8456 |
| Mean age | 50.1 |
| Female | 90.6% |
| Geographical location, number of studies (n) | |
| - Europe | 21 (2992) |
| - North America | 16 (4401) |
| - East Asia | 8 (614) |
| - Oceania | 5 (287) |
| - Middle East | 2 (98) |
| - South Asia | 1 (64) |
| Year of publication, number of studies (n) | |
| - Before 2018 | 15 (1065) |
| - After 2018 | 39 (7509) |
| Study design, number of studies (n) | |
| Prospective | 12 (2757) |
| Retrospective | 28 (3216) |
| Cross sectional | 10 (1966) |
| Mixed | 4 (635) |
| Past history, percentage (n) | |
| Smoking | |
| - Active | 13.0% (4385) |
| - Past | 23.0% (2620) |
| - Currency status not provided | 30.1% (2731) |
| Hypertension | 37.3% (7930) |
| Diabetes mellitus | 4.4% (7945) |
| Migraine | 30.8% (3889) |
| Peripheral vascular disease | 1.5% (298) |
| Chronic kidney disease | 1.9% (994) |
| History of previous coronary artery disease | 8.8% (3077) |
| Thyroid disorders | 13.2% (3122) |
| Peripartum | 10.0% (1522) |
| Family history of cardiovascular disease | 34.6% (2143) |
| Depression | 18.5% (2409) |
| Anxiety | 22.0% (1959) |
| In-hospital MACE | 7.3% (2175) |
| Follow-up MACE | 12.4% (4341) |
| Range of mean follow-up | 1 month–49.2 months |
| Range of median follow-up | 12 months–90 months |
MACE, major adverse cardiovascular event; n, total number of patients for whom the data was reported.
Most studies reported MACE as a composite of death, non-fatal MI and revascularisation with stroke, heart failure, and recurrent or de novo SCAD also reported in some studies. MACE occurred in 7.3% of patients in-hospital and 12.4% on follow-up. Total mortality was reported in 20 studies. Follow-up time varied significantly between studies with mean follow-up ranging between 1 month and 49.2 months.
Time to angiography
Only three studies reported time to angiogram or revascularisation and the methods of report were highly heterogenous. Two studies reported the mean time from symptoms onset to angiogram, with one reported 95% CI (24 hours (4–48))9 and the other reported standard deviation (7±5.4 days).10 In another study,11 door-to-balloon time was reported with the difference between patients with SCAD and other causes of AMI being not statistically significant (median 142 min for SCAD vs 99 min for other AMI, p=0.301). Due to heterogeneity, meta-analysis was not performed for this parameter.
Medical management, FMD screening and cardiac rehabilitation referral
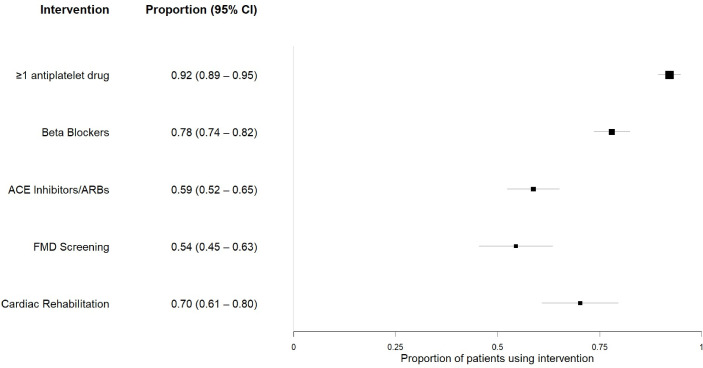
Using random effects meta-analysis, 92.1% of patients (95% CI 89.3% to 94.8%) received at least one antiplatelet, 78.0% (95% CI 73.5% to 82.4%) received beta-blockers, 58.7% (95% CI 52.3% to 65.1%) received ACEIs/ARBs, 54.4% (95% CI 45.4% to 63.5%) were screened for FMD and 70.2% (95% CI 60.8% to 79.5%) were referred to cardiac rehabilitation (figure 2). Left ventricular ejection fraction (LVEF) was not reported in most studies. Among the few studies that reported LVEF, none reported if ACEIs/ARBs were given to patients with impaired LVEF. One study12 reported the proportion of patients (29.6%) who received all consensus-document recommended treatments.
Figure 2.
Meta-analysis of quality-of-care parameters—forest plot depiction for random effect meta-analysis of the proportion of patients received each of the recommended interventions using data from all included studies. Note: ARB, angiotensin receptor blocker; FMD, fibromuscular dysplasia.
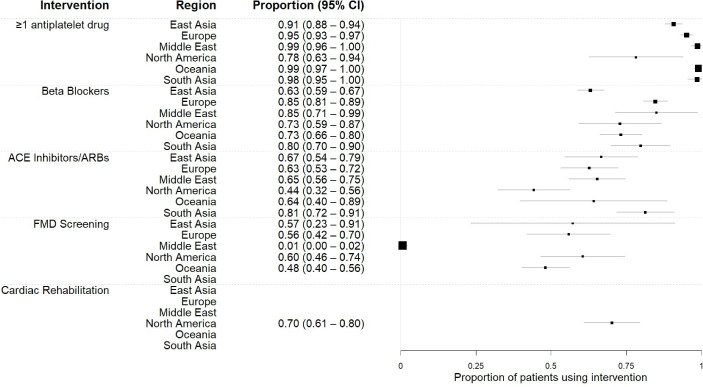
Meta regression analysis of the quality-of-care parameters differed significantly between geographical regions (figure 3) except for the use of ACEIs/ARBs (p=0.088) and cardiac rehabilitation (data for this were only available for North America). Use of at least one antiplatelet was most consistent, with proportions close to 100% in most regions, except for North America (at 78.2%). Use of beta-blockers was also consistently higher than 63% in all regions, while ACEIs/ARBs ranged from 44.2% to 81.3%. Screening for FMD was the most inconsistent parameter, which was lowest in the Middle East (0.6%) and highest in North America (60.5%). North America was also the only region where the rate of cardiac rehabilitation attendance or referral was reported (70.2%, CI 60.9% to 79.5%).
Figure 3.
Meta-analysis of quality-of-care parameters by regions—forest plot depiction of random effect meta-analysis of the proportion of patients received each of the recommended interventions, grouped by regions. Note: ARB, angiotensin receptor blocker; FMD, fibromuscular dysplasia.
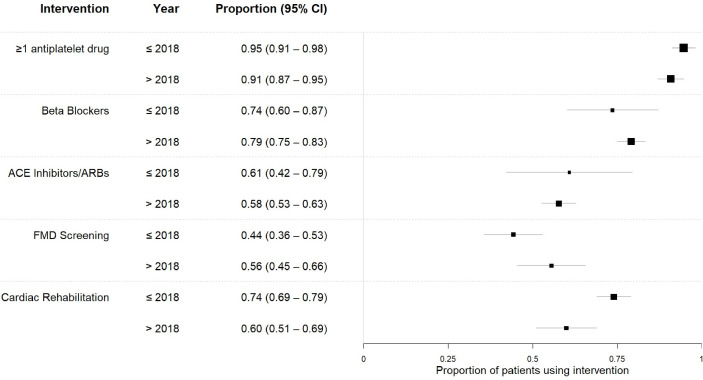
Overall, no significant difference was observed in the proportion of patients receiving each of the recommended treatments between studies published before and after 2018 (figure 4), except for a small deterioration in the proportion of patients undergone cardiac rehabilitation (74.1% vs 60.0%, p=0.012). This parameter, however, was only reported on in North America.
Figure 4.
Meta-analysis of quality-of-care parameters by year of publication—forest plot depiction of random effect meta-analysis of the proportion of patients received each of the recommended interventions, grouped by year of publication. Note: ARB, angiotensin receptor blocker; FMD, fibromuscular dysplasia.
Temporal changes within the same cohorts
The change of quality-of-care parameters within the same cohorts was explored in table 4. Apart from the use of antiplatelets, which consistently increased with time, other parameters fluctuated significantly between the cohorts. The greatest change was observed in the Kantonsspital St. Gallen cohort (drop in FMD screening rate from 62.5% to 38.1%) and Mayo Clinic SCAD Registry (rise in FMD screening rate from 45.5% to 68.1%). There were no data for the change in the rate of referral to cardiac rehabilitation.
Table 4.
Change of quality-of-care parameters on the same cohorts with time
| Cohort | Study | N | Time from | Time to | Antiplatelets | Beta-blocker | ACEIs/ ARBs | FMD screening | Cardiac rehabilitation |
| Canadian SCAD | Saw et al22 2017 | 327 | 04/2012 | 12/2016 | 92 | 83 | 57.6 | 80.7 | ND |
| Saw et al23 2019 | 750 | 06/2014 | 06/2018 | 93.7 | 84.8 | 57.4 | 73.3 | ND | |
| Spanish Registry for SCAD | Garcia-Guimaraes et al29 2021 | 318 | 06/2015 | 04/2019 | 92 | 79 | 51 | 29 | ND |
| Garcia-Guimaraes et al30 2022 | 389 | 06/2015 | 12/2020 | 93 | 80 | 51 | 27 | ND | |
| Kantonsspital St. Gallen cohort | Rogowski et al33 2017 | 64 | 01/1998 | 01/2015 | 97 | 86 | 36 | 63 | ND |
| Seidl et al34 2021 | 105 | 01/1998 | 12/2020 | 97 | 80 | 42 | 38.1 | ND | |
| Kaiser Permanente Northern California cohort | Chen et al35 2019 | 111 | 01/2003 | 12/2012 | 94 | 88 | 63 | 49.5 | ND |
| Chen et al36 2021 | 307 | 09/2002 | 06/2017 | 94.1 | 84 | 59.3 | 50 | ND | |
| Mayo Clinic Virtual SCAD Registry | Kok et al37 2018 | 585 | 01/2010 | 01/2017 | 89 | 59 | ND | 57.3 | ND |
| Johnson et al38 2022 | 1196 | 08/2011 | 03/2020 | ND | ND | ND | 68.8 | ND | |
| Mayo Clinic SCAD Registry | Eleid et al39 2014 | 246 | 01/1979 | 12/2013 | ND | ND | ND | 45.5 | ND |
| Turley et al44 2020 | 667 | 08/2011 | 08/2018 | ND | ND | ND | 68.1 | ND |
ND, No data; SCAD, spontaneous coronary artery dissection.
Discussion
This systematic review is the first to measure adherence to consensus recommendations in patients with SCAD. Overall, adherence to consensus recommendations in SCAD care was highest for antiplatelet therapy and lowest for FMD screening, with significant variations across geographical regions. There was little change in adherence to consensus recommendations before and after the publication of consensus recommendations in 2018.
Medical management and antiplatelet therapy
The proportions of patients with SCAD receiving antiplatelets, beta-blockers, FMD screening and cardiac rehabilitation were 94.5%, 78%, 54.6% and 70.5%, respectively. With regards to antiplatelet therapy, there is no quality evidence guiding the use of single versus dual antiplatelet, or the duration of therapy. In our review, the proportions of patients on single-antiplatelet therapy were provided in almost all studies which reported on this parameter (35 out of 37 studies), while the use of dual therapy was only provided in half (17 out of 37 studies).
Temporal and geographical trends in SCAD care
No significant change in practice was observed for studies published before and after 2018. The proportion of patients who received all of the recommended treatments would have been a good indicator of overall quality of care. Unfortunately, there was only one paper (Baechler et al13) that reported this composite parameter, with the number relatively low at 29.6%. Notably, there was significant heterogeneity across studies and regions in FMD screening, ranging from 0.6% to 60.6%. This is despite the well-known association between SCAD and FMD, with screening recommended in all patients to look for extracardiac vascular manifestations. Most of the studies included in our systematic review were from higher income countries, highlighting a paucity of data from lower income countries. It is possible that adherence would be lower than our current data, particularly for FMD screening and rehab referral, due to limitations in resources in these countries.
SCAD awareness and cardiac rehabilitation referral
SCAD is an increasingly recognised condition and, consistent with this, we found nearly eight times the number of patients studied in the past 4 years, compared with the 30 years prior. Although there was no significant change in most of the quality-of-care parameters in studies published before and after 2018, this was likely a consequence of later studies including patients recruited historically, diluting any change in the quality-of-care with time. The drop in the proportion of patients who underwent cardiac rehabilitation was related to under reporting and differences in type of reporting. Only 3/53 studies provided information on cardiac rehabilitation, with the method of reporting varied. While one provided the rate of referral to cardiac rehabilitation,14 the other two reported on the proportion of patients who attended cardiac rehabilitation.13 15
Limitations
This systematic review is limited by the under reporting of several quality-of-care measures, particularly cardiac rehabilitation and FMD screening. We were also unable to determine use of single vs dual antiplatelet therapy in many studies. The benefit of medical therapy in SCAD, such as antiplatelets and beta blockers remains controversial, with no randomised data to support their use. Most studies reported discharge medical therapy whereby adverse effects related to antiplatelets or beta blockers may have led to early cessation, and we cannot comment on adherence to such therapy. The included studies were heterogenous and were conducted with different aims. In a small number of studies, the percentage of females was low, and it is possible that some atherosclerotic dissections may have been included in these studies. There was an under-reporting of the practice of FMD screening (24 studies) and cardiac rehabilitation (three studies). The risk of reporting bias could not be excluded.
Conclusion
There are significant variations in the management of SCAD globally, particularly with regards to FMD screening and cardiac rehabilitation referral. An improvement in adherence to recommended therapies is thus needed. Raising awareness among clinicians about these recommendations, together with further prospective evidence on their effectiveness in reducing MACE, may help improve quality of care for patients with SCAD.
Acknowledgments
Special thanks to all the co-authors who have contributed to this paper.
Footnotes
Twitter: @quan_m_dang
Presented at: Findings from this study was presented at the 71st Annual Scientific Meeting of the Cardiac Society of Australia and New Zealand and the 2023 European Society of Cardiology Congress.
Contributors: QD: conceptualisation, methodology, investigation, formal analysis, writing - original draft preparation, guarantor. FO, BS, RS: investigation, validation, writing – review and editing. SM: software, formal analysis, data curation, visualisation, writing – review and editing. PP and RKA: writing – review and editing. JC: writing – review and editing. SM: supervision, project administration, conceptualisation, methodology, writing - review and editing.
Funding: QD received a Faculty of Medicine and Health Research Centres Stipend Scholarship from the University of Sydney. SZ was supported by a Heart Foundation Fellowship (ID 102627) and a New South Wales Health Cardiovascular Research Elite Postdoctoral Grant for this work. JJHC was supported by an Investigator grant APP1194139 from National Health & Medical Research Council of Australia. RAL is supported by a British Heart Foundation fellowship (FS/ICRF/22/26051).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available upon reasonable request. The data underlying this article will be shared on reasonable request to the corresponding author.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1.Hayes SN, Kim ESH, Saw J, et al. Spontaneous coronary artery dissection: Current state of the science: A scientific statement from the American heart Association. Circulation 2018;137:e523–57. 10.1161/CIR.0000000000000564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adlam D, Alfonso F, Maas A, et al. European society of cardiology, acute cardiovascular care Association, SCAD study group: a position paper on spontaneous coronary artery dissection. Eur Heart J 2018;39:3353–68. 10.1093/eurheartj/ehy080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zanchin C, Ledwoch S, Bär S, et al. Acute coronary syndromes in young patients: phenotypes, causes and clinical outcomes following percutaneous coronary interventions. International Journal of Cardiology 2022;350:1–8. 10.1016/j.ijcard.2022.01.018 [DOI] [PubMed] [Google Scholar]
- 4.Meng P-N, Xu C, You W, et al. Spontaneous coronary artery dissection as a cause of acute myocardial infarction in young female population: A single-center study. Chinese Medical Journal 2017;130:1534–9. 10.4103/0366-6999.208245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nakashima T, Noguchi T, Haruta S, et al. Prognostic impact of spontaneous coronary artery dissection in young female patients with acute myocardial infarction: A report from the angina Pectoris-myocardial infarction multicenter investigators in Japan. International Journal of Cardiology 2016;207:341–8. 10.1016/j.ijcard.2016.01.188 [DOI] [PubMed] [Google Scholar]
- 6.Chi G, Najafi H, Montazerin SM, et al. Factors associated with recurrent spontaneous coronary artery dissection: a systematic review and meta-analysis. Coron Artery Dis 2022;33:566–73. 10.1097/MCA.0000000000001168 [DOI] [PubMed] [Google Scholar]
- 7.Stevens CJ, Shaffer JA, Edwards KS, et al. Younger age impacts perceptions of care received in the emergency Department among women with spontaneous coronary artery dissection. Journal of Women’s Health 2022;31:1165–72. 10.1089/jwh.2021.0162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. International Journal of Surgery 2021;88:105906. 10.1016/j.ijsu.2021.105906 [DOI] [PubMed] [Google Scholar]
- 9.Alfonso F, Paulo M, Gonzalo N, et al. Diagnosis of spontaneous coronary artery dissection by optical coherence tomography. Journal of the American College of Cardiology 2012;59:1073–9. 10.1016/j.jacc.2011.08.082 [DOI] [PubMed] [Google Scholar]
- 10.Chang S, Dai Y, Song X, et al. Characteristics, management, and prognosis of spontaneous coronary intramural Hematoma. Angiology 2022;73:374–9. 10.1177/00033197211036220 [DOI] [PubMed] [Google Scholar]
- 11.Murugiah K, Chen L, Dreyer RP, et al. Health status outcomes after spontaneous coronary artery dissection and comparison with other acute myocardial infarction: the VIRGO experience. PLoS ONE 2022;17:e0265624. 10.1371/journal.pone.0265624 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNair PW, Parker A, Taylor A, et al. Spontaneous coronary artery dissection and its association with Fibromuscular dysplasia and other vascular abnormalities. The American Journal of Cardiology 2020;125:34–9. 10.1016/j.amjcard.2019.09.043 [DOI] [PubMed] [Google Scholar]
- 13.Baechler CJ, Witt DR, Lohese O, et al. Spontaneous coronary artery dissection and evidence-based medicine. The American Journal of Cardiology 2022;171:65–8. 10.1016/j.amjcard.2022.01.046 [DOI] [PubMed] [Google Scholar]
- 14.Wagers TP, Stevens CJ, Ross KV, et al. Spontaneous coronary artery dissection (SCAD): female survivors' experiences of stress and support. J Cardiopulm Rehabil Prev 2018;38:374–9. 10.1097/HCR.0000000000000330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Liang JJ, Tweet MS, Hayes SE, et al. Prevalence and predictors of depression and anxiety among survivors of myocardial infarction due to spontaneous coronary artery dissection. J Cardiopulm Rehabil Prev 2014;34:138–42. 10.1097/HCR.0000000000000030 [DOI] [PubMed] [Google Scholar]
- 16.Daoulah A, Al-Faifi SM, Alsheikh-Ali AA, et al. Ventricular arrhythmias in patients with spontaneous coronary artery dissection: findings from the Gulf spontaneous coronary artery dissection (Gulf SCAD) Registry. Crit Pathw Cardiol 2020;19:146–52. 10.1097/HPC.0000000000000219 [DOI] [PubMed] [Google Scholar]
- 17.Daoulah A, Al-Faifi SM, Alhamid S, et al. Spontaneous coronary artery dissection in the Gulf: G-SCAD Registry. Angiology 2021;72:32–43. 10.1177/0003319720946974 [DOI] [PubMed] [Google Scholar]
- 18.Daoulah A, Al-Faifi SM, Hurley WT, et al. Spontaneous coronary artery dissection: does being unemployed matter? insights from the GSCAD Registry. CCR 2021;17:328–39. 10.2174/1573403X16999200817173944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Daoulah A, Al-Faifi SM, Hersi AS, et al. Spontaneous coronary artery dissection in relation to physical and emotional stress: A retrospective study in 4 Arab Gulf countries. Current Problems in Cardiology 2021;46:100484. 10.1016/j.cpcardiol.2019.100484 [DOI] [PubMed] [Google Scholar]
- 20.Daoulah A, Al-Faifi SM, Madan M, et al. Clinical presentation and outcome of patients with spontaneous coronary artery dissection versus Atherosclerotic coronary plaque dissection. Crit Pathw Cardiol 2021;20:36–43. 10.1097/HPC.0000000000000233 [DOI] [PubMed] [Google Scholar]
- 21.Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing Arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645–55. 10.1161/CIRCINTERVENTIONS.114.001760 [DOI] [PubMed] [Google Scholar]
- 22.Saw J, Humphries K, Aymong E, et al. Spontaneous coronary artery dissection: clinical outcomes and risk of recurrence. J Am Coll Cardiol 2017;70:1148–58. 10.1016/j.jacc.2017.06.053 [DOI] [PubMed] [Google Scholar]
- 23.Saw J, Starovoytov A, Humphries K, et al. Canadian spontaneous coronary artery dissection cohort study: in-hospital and 30-day outcomes. Eur Heart J 2019;40:1188–97. 10.1093/eurheartj/ehz007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Combaret N, Gerbaud E, Dérimay F, et al. National French Registry of spontaneous coronary artery Dissections: prevalence of Fibromuscular dysplasia and genetic analyses. EuroIntervention 2021;17:508–15. 10.4244/EIJ-D-20-01046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Combaret N, Liabot Q, Deiri M, et al. Characteristics and prognosis of patients with Fibromuscular dysplasia in a population of spontaneous coronary artery Dissections (from the French Registry of spontaneous coronary artery Dissections "DISCO. The American Journal of Cardiology 2022;175:38–43. 10.1016/j.amjcard.2022.04.007 [DOI] [PubMed] [Google Scholar]
- 26.Alfonso F, García-Guimaraes M, Alvarado T, et al. Clinical implications of arterial hypertension in patients with spontaneous coronary artery dissection. Coron Artery Dis 2022;33:75–80. 10.1097/MCA.0000000000001043 [DOI] [PubMed] [Google Scholar]
- 27.Díez-Villanueva P, García-Guimaraes M, Sanz-Ruiz R, et al. Spontaneous coronary artery dissection in old patients: clinical features, angiographic findings, management and outcome. Eur Heart J Acute Cardiovasc Care 2021;10:926–32. 10.1093/ehjacc/zuaa029 [DOI] [PubMed] [Google Scholar]
- 28.Díez-Villanueva P, García-Guimaraes MM, Macaya F, et al. Spontaneous coronary artery dissection and Menopause. The American Journal of Cardiology 2021;148:53–9. 10.1016/j.amjcard.2021.02.007 [DOI] [PubMed] [Google Scholar]
- 29.García-Guimaraes M, Bastante T, Macaya F, et al. Spontaneous coronary artery dissection in Spain: clinical and angiographic characteristics, management, and in-hospital events. Revista Española de Cardiología (English Edition) 2021;74:15–23. 10.1016/j.rec.2020.04.002 [DOI] [PubMed] [Google Scholar]
- 30.Garcia-Guimaraes M, Masotti M, Sanz-Ruiz R, et al. Clinical outcomes in spontaneous coronary artery dissection. Heart 2022;108:1530–8. 10.1136/heartjnl-2022-320830 [DOI] [PubMed] [Google Scholar]
- 31.Macaya F, Salinas P, Gonzalo N, et al. Long-term follow-up of spontaneous coronary artery dissection treated with Bioresorbable scaffolds. EuroIntervention 2019;14:1403–5. 10.4244/EIJ-D-18-00519 [DOI] [PubMed] [Google Scholar]
- 32.Carss KJ, Baranowska AA, Armisen J, et al. Spontaneous coronary artery dissection: insights on rare genetic variation from genome sequencing. Circ Genom Precis Med 2020;13:e003030. 10.1161/CIRCGEN.120.003030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rogowski S, Maeder MT, Weilenmann D, et al. Spontaneous coronary artery dissection: angiographic follow-up and long-term clinical outcome in a predominantly medically treated population. Catheter Cardiovasc Interv 2017;89:59–68. 10.1002/ccd.26383 [DOI] [PubMed] [Google Scholar]
- 34.Seidl S, Rickli H, Rogowski S, et al. Long-term follow-up of medically treated patients with spontaneous coronary artery dissection: a prospective, Swiss single-centre cohort study. Swiss Med Wkly 2021;151:w30067. 10.4414/SMW.2021.w30067 [DOI] [PubMed] [Google Scholar]
- 35.Chen S, Merchant M, Mahrer KN, et al. Spontaneous coronary artery dissection: clinical characteristics, management, and outcomes in a racially and ethnically diverse community-based cohort. TPJ 2019;23:23. 10.7812/TPP/18.278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen S, Merchant M, Mahrer KN, et al. Pregnancy-associated spontaneous coronary artery dissection: clinical characteristics, outcomes, and risk during subsequent pregnancy. J Invasive Cardiol 2021;33:E457–66. [DOI] [PubMed] [Google Scholar]
- 37.Kok SN, Hayes SN, Cutrer FM, et al. Prevalence and clinical factors of migraine in patients with spontaneous coronary artery dissection. JAHA 2018;7:e010140. 10.1161/JAHA.118.010140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Johnson AK, Tweet MS, Rouleau SG, et al. The presentation of spontaneous coronary artery dissection in the emergency Department: signs and symptoms in an unsuspecting population. Academic Emergency Medicine 2022;29:423–8. 10.1111/acem.14426 Available: https://onlinelibrary.wiley.com/toc/15532712/29/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eleid MF, Guddeti RR, Tweet MS, et al. Coronary artery Tortuosity in spontaneous coronary artery dissection: angiographic characteristics and clinical implications. Circ Cardiovasc Interv 2014;7:656–62. 10.1161/CIRCINTERVENTIONS.114.001676 [DOI] [PubMed] [Google Scholar]
- 40.Krittanawong C, Tweet MS, Hayes SE, et al. Usefulness of cardiac rehabilitation after spontaneous coronary artery dissection. The American Journal of Cardiology 2016;117:1604–9. 10.1016/j.amjcard.2016.02.034 [DOI] [PubMed] [Google Scholar]
- 41.Tweet MS, Eleid MF, Best PJM, et al. Spontaneous coronary artery dissection: Revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777–86. 10.1161/CIRCINTERVENTIONS.114.001659 [DOI] [PubMed] [Google Scholar]
- 42.Tweet MS, Hayes SN, Codsi E, et al. Spontaneous coronary artery dissection associated with pregnancy. Journal of the American College of Cardiology 2017;70:426–35. 10.1016/j.jacc.2017.05.055 [DOI] [PubMed] [Google Scholar]
- 43.Tweet MS, Young KA, Best PJM, et al. Association of pregnancy with recurrence of spontaneous coronary artery dissection among women with prior coronary artery dissection. JAMA Netw Open 2020;3:e2018170. 10.1001/jamanetworkopen.2020.18170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Turley TN, O’Byrne MM, Kosel ML, et al. Identification of susceptibility Loci for spontaneous coronary artery dissection. JAMA Cardiol 2020;5:929. 10.1001/jamacardio.2020.0872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McGrath-Cadell L, McKenzie P, Emmanuel S, et al. Outcomes of patients with spontaneous coronary artery dissection. Open Heart 2016;3:e000491. 10.1136/openhrt-2016-000491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rashid HNZ, Wong DTL, Wijesekera H, et al. Incidence and Characterisation of spontaneous coronary artery dissection as a cause of acute coronary syndrome--A single-centre Australian experience. International Journal of Cardiology 2016;202:336–8. 10.1016/j.ijcard.2015.09.072 [DOI] [PubMed] [Google Scholar]
- 47.Adams H, Paratz E, Somaratne J, et al. Different patients, different outcomes: A case-control study of spontaneous coronary artery dissection versus acute coronary syndrome. J Interven Cardiology 2018;31:41–7. 10.1111/joic.12447 Available: https://onlinelibrary.wiley.com/toc/15408183/31/1 [DOI] [PubMed] [Google Scholar]
- 48.Tarr I, Hesselson S, Iismaa SE, et al. Exploring the genetic architecture of spontaneous coronary artery dissection using whole-genome sequencing. Circ Genom Precis Med 2022;15:e003527. 10.1161/CIRCGEN.121.003527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chou AY, Prakash R, Rajala J, et al. The first dedicated cardiac rehabilitation program for patients with spontaneous coronary artery dissection: description and initial results. Canadian Journal of Cardiology 2016;32:554–60. 10.1016/j.cjca.2016.01.009 [DOI] [PubMed] [Google Scholar]
- 50.Bouchard K, Coutinho T, Reed J, et al. Recovering from spontaneous coronary artery dissection: patient-reported challenges and Rehabilitative intervention needs. Health Psychology 2021;40:472–9. 10.1037/hea0001086 [DOI] [PubMed] [Google Scholar]
- 51.Inohara T, Alfadhel M, Choi D, et al. Coronary angiographic manifestations and outcomes in spontaneous coronary artery dissection patients with and without Fibromuscular dysplasia. Canadian Journal of Cardiology 2021;37:1725–32. 10.1016/j.cjca.2021.08.019 [DOI] [PubMed] [Google Scholar]
- 52.Solomonica A, Wagner C, Lavi S. Endothelial dysfunction is not associated with spontaneous coronary artery dissection. Cardiovascular Revascularization Medicine 2020;21:1539–41. 10.1016/j.carrev.2020.05.029 [DOI] [PubMed] [Google Scholar]
- 53.Sun Y, Chen Y, Li Y, et al. Association of Tsr1 variants and spontaneous coronary artery dissection. Journal of the American College of Cardiology 2019;74:167–76. 10.1016/j.jacc.2019.04.062 [DOI] [PubMed] [Google Scholar]
- 54.Hui P, Bai Y, Su X, et al. The value of plasma Fibrillin-1 level in patients with spontaneous coronary artery dissection. International Journal of Cardiology 2020;302:150–6. 10.1016/j.ijcard.2019.12.015 [DOI] [PubMed] [Google Scholar]
- 55.Mortensen KH, Thuesen L, Kristensen IB, et al. Spontaneous coronary artery dissection: a Western Denmark heart Registry study. Cathet Cardio Intervent 2009;74:710–7. 10.1002/ccd.22115 Available: https://onlinelibrary.wiley.com/toc/1522726x/74/5 [DOI] [PubMed] [Google Scholar]
- 56.Basavanna D, Manjunath C, Panneerselvam A, et al. Spontaneous coronary artery dissection: A retrospective analysis of 19,676 coronary angiograms. J Clin Prev Cardiol 2017;6:133. 10.4103/JCPC.JCPC_15_17 [DOI] [Google Scholar]
- 57.Almasi A, Mansouri P, Jameie M, et al. Clinical features and prognoses of middle-aged women with ST-elevation myocardial infarction with a focus on spontaneous coronary artery dissection. Crit Pathw Cardiol 2022;21:18–23. 10.1097/HPC.0000000000000275 [DOI] [PubMed] [Google Scholar]
- 58.Lettieri C, Zavalloni D, Rossini R, et al. Management and long-term prognosis of spontaneous coronary artery dissection. The American Journal of Cardiology 2015;116:66–73. 10.1016/j.amjcard.2015.03.039 [DOI] [PubMed] [Google Scholar]
- 59.Antonutti M, Baldan F, Lanera C, et al. Spontaneous coronary artery dissection: role of Prognostic markers and relationship with genetic analysis. International Journal of Cardiology 2021;326:19–29. 10.1016/j.ijcard.2020.10.040 [DOI] [PubMed] [Google Scholar]
- 60.Solinas E, Alabrese R, Cattabiani MA, et al. Spontaneous coronary artery dissection: an Italian single centre experience. J Cardiovasc Med (Hagerstown) 2022;23:141–8. 10.2459/JCM.0000000000001256 [DOI] [PubMed] [Google Scholar]
- 61.Cerrato E, Giacobbe F, Quadri G, et al. Antiplatelet therapy in patients with conservatively managed spontaneous coronary artery dissection from the Multicentre DISCO Registry. Eur Heart J 2021;42:3161–71. 10.1093/eurheartj/ehab372 [DOI] [PubMed] [Google Scholar]
- 62.Nishiguchi T, Tanaka A, Taruya A, et al. Prognosis of spontaneous coronary artery dissection treated by percutaneous coronary intervention with optical coherence tomography. Journal of Cardiology 2017;70:524–9. 10.1016/j.jjcc.2017.03.009 [DOI] [PubMed] [Google Scholar]
- 63.Inohara T, Saw J, Kohsaka S, et al. Treatment pattern and outcome of spontaneous coronary artery dissection in Japan. International Journal of Cardiology 2020;316:13–8. 10.1016/j.ijcard.2020.04.082 [DOI] [PubMed] [Google Scholar]
- 64.Inoue Y, Tanaka A, Asano H, et al. Clinical characteristics and treatment of spontaneous coronary artery dissection in young women undergoing percutaneous coronary intervention. J Cardiovasc Med (Hagerstown) 2021;22:14–9. 10.2459/JCM.0000000000001067 [DOI] [PubMed] [Google Scholar]
- 65.Kim Y, Han X, Ahn Y, et al. Clinical characteristics of spontaneous coronary artery dissection in young female patients with acute myocardial infarction in Korea. Korean J Intern Med 2021;36:106–13. 10.3904/kjim.2019.118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McAlister CP, Yi M, Adamson PD, et al. Trends in the detection, management and 30-day outcomes of spontaneous coronary artery dissection: A six-year, New Zealand centre experience. Heart, Lung and Circulation 2021;30:78–85. 10.1016/j.hlc.2020.06.020 [DOI] [PubMed] [Google Scholar]
- 67.Romero-Rodríguez N, Fernández-Quero M, Gil-Ortega MV, et al. Spontaneous coronary dissection and its long-term Prognostic implications in a cohort of 19 cases. Revista Española de Cardiología (English Edition) 2010;63:1088–91. 10.1016/S1885-5857(10)70213-9 [DOI] [PubMed] [Google Scholar]
- 68.Alfonso F, Paulo M, Lennie V, et al. “Spontaneous coronary artery dissection: long-term follow-up of a large series of patients prospectively managed with a "conservative" therapeutic strategy”. JACC Cardiovasc Interv 2012;5:1062–70. 10.1016/j.jcin.2012.06.014 [DOI] [PubMed] [Google Scholar]
- 69.Camacho Freire SJ, Díaz Fernández JF, Gheorghe LL, et al. Spontaneous coronary artery dissection and hypothyroidism. Revista Española de Cardiología (English Edition) 2019;72:625–33. 10.1016/j.rec.2018.06.031 [DOI] [PubMed] [Google Scholar]
- 70.Bastante T. Contemporary management of spontaneous coronary dissection. REC Interventional Cardiology 2020;2:247–55. [Google Scholar]
- 71.Macaya F, Vedia Ó, Salazar CH, et al. Clinical outcomes of patients presenting with spontaneous coronary artery dissection versus Takotsubo syndrome: a propensity score analysis. Eur Heart J Acute Cardiovasc Care 2020;9:694–702. 10.1177/2048872619886311 [DOI] [PubMed] [Google Scholar]
- 72.Mori R, Macaya F, Sara JD, et al. Non-invasive assessment of endothelial function in patients with spontaneous coronary artery dissection: A case-control study. International Journal of Cardiology 2020;316:40–2. 10.1016/j.ijcard.2020.04.049 [DOI] [PubMed] [Google Scholar]
- 73.Wilander H, Pagonis C, Venetsanos D, et al. Nationwide observational study of incidence, management and outcome of spontaneous coronary artery dissection: a report from the Swedish coronary angiography and Angioplasty register. BMJ Open 2022;12:e060949. 10.1136/bmjopen-2022-060949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Smaardijk VR, Mommersteeg PMC, Kop WJ, et al. Psychological and clinical characteristics of female patients with spontaneous coronary artery dissection. Neth Heart J 2020;28:485–91. 10.1007/s12471-020-01437-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Androulakis E, Azzu A, Papagkikas P, et al. Spontaneous coronary artery dissection: insights from cardiac magnetic resonance and Extracoronary arterial screening. Circulation 2022;145:555–7. 10.1161/CIRCULATIONAHA.121.058056 [DOI] [PubMed] [Google Scholar]
- 76.Kotecha D, Garcia-Guimaraes M, Premawardhana D, et al. Risks and benefits of percutaneous coronary intervention in spontaneous coronary artery dissection. Heart 2021;107:1398–406. 10.1136/heartjnl-2020-318914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.DeMaio SJ Jr, Kinsella SH, Silverman ME. Clinical course and long-term prognosis of spontaneous coronary artery dissection. The American Journal of Cardiology 1989;64:471–4. 10.1016/0002-9149(89)90423-2 [DOI] [PubMed] [Google Scholar]
- 78.Clare R, Duan L, Phan D, et al. Characteristics and clinical outcomes of patients with spontaneous coronary artery dissection. JAHA 2019;8:e012570. 10.1161/JAHA.119.012570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sharma S, Kaadan MI, Duran JM, et al. Risk factors, imaging findings, and sex differences in spontaneous coronary artery dissection. The American Journal of Cardiology 2019;123:1783–7. 10.1016/j.amjcard.2019.02.040 [DOI] [PubMed] [Google Scholar]
- 80.White Solaru K, Heupler F, Cho L, et al. Prevalence of coronary vasospasm using coronary reactivity testing in patients with spontaneous coronary artery dissection. The American Journal of Cardiology 2019;123:1812–5. 10.1016/j.amjcard.2019.03.001 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
openhrt-2023-002379supp001.pdf (78.9KB, pdf)
Data Availability Statement
Data are available upon reasonable request. The data underlying this article will be shared on reasonable request to the corresponding author.