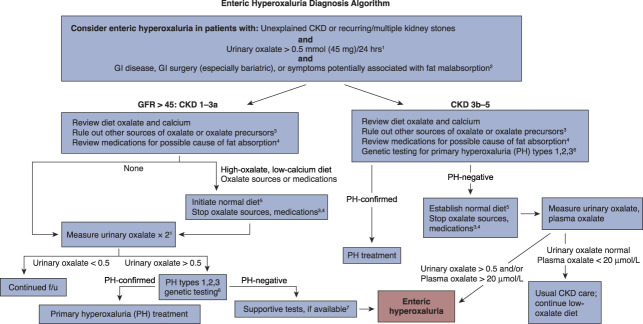
Figure 1.
Enteric hyperoxaluria diagnostic algorithm. Enteric hyperoxaluria is caused by the increased absorption of oxalate from foods in the digestive tract (also called the gut or intestines). This leads to high levels of oxalate in the urine. Enteric hyperoxaluria may occur as a result of certain weight loss surgeries or in inflammatory bowel disease, including Crohn disease, cystic fibrosis, or chronic pancreatitis. Excess oxalate in the urine may lead to recurring kidney stones, CKD, or kidney failure. Symptoms vary but may include kidney stones, loose stools, or weight loss. 124-hour urine collection is important for measurement of oxalate. In children, measurements should be corrected for BSA, with normal values <0.45 mmol/1.73 m2 per 24 hours. In very young children unable to complete a 24-hour urine collection, urine oxalate/urine creatinine ratio may be used to estimate oxalate excretion. Urinary oxalate excretion can be variable in enteric hyperoxaluria, so a normal urinary oxalate does not exclude the possibility of enteric hyperoxaluria. 2Any gastrointestinal (GI) disease that causes fat malabsorption, such as cystic fibrosis or inflammatory bowel disease, may result in enteric hyperoxaluria. Symptoms of malabsorption include diarrhea, fatty stools, or weight loss. Patients can have significant fat malabsorption and enteric hyperoxaluria without GI symptoms. 3Oxalate precursors include vitamin C, which is metabolized to oxalate and may be consumed in high doses by some patients. This is a particular problem in patients with advanced CKD who are less able to excrete resulting oxalate. Low doses of vitamin C, such as those contained in daily multivitamins, are not a concern. 4Medications that can cause fat malabsorption include orlistat, tetracycline, colchicine, acarbose, phenytoin, cholestyramine, laxatives, and ezetimibe. 5Elimination of potential oxalate sources in diet and medications should be maintained for 1–3 months before recheck of urinary oxalate. For purposes of this algorithm, a normal diet is one that avoids intake of high oxalate foods, contains the recommended daily allowance for calcium, and is low fat. If dietary changes are needed, it is recommended that patients be provided with lists of high-oxalate foods to be avoided (www.ohf.org). 6If there is an obvious source of GI hyperabsorption of oxalate, such as new onset after bariatric surgery, PH genetic testing may not be required. 7Elevated fecal fat supports the diagnosis; measurement is recommended but not essential. GI absorption of oxalate can be tested in some referral centers by oral administration and measurement in urine of 13C oxalate but is not widely available. f/u, follow-up; PH, primary hyperoxaluria.