Fig. 4. In situ modulation of immune cell function by changing biomaterial properties and mechanical stimulation.
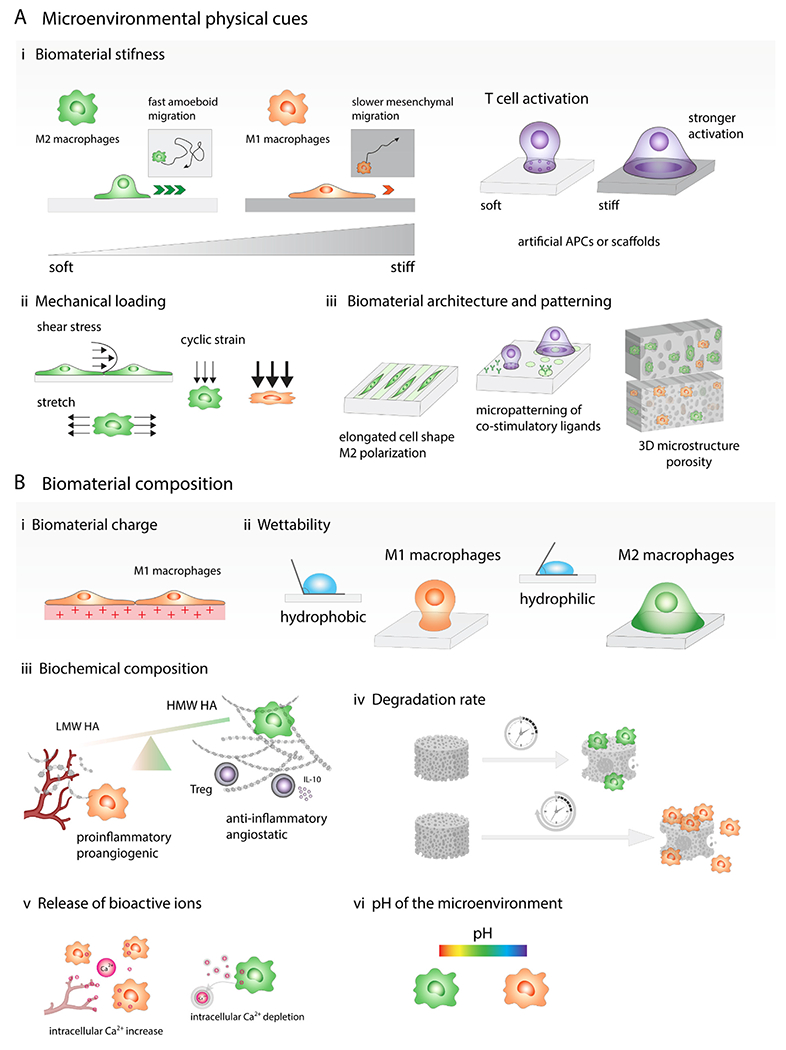
(A) Microenvironmental physical cues. (i) Stiff biomaterials prime macrophages towards M1-like phenotype, while softer ones direct macrophages into anti-inflammatory state. Macrophages cultured on the softer substrates display fast amoeboid migration, while macrophages on stiff gels adopt slower mesenchymal migration. T cell activation by interactions with antigen presenting cell (APC) can be replicated by biomaterials functionalized with ligands that bind to receptors on the T cell surface and biomaterial stiffness is one of the parameters that might significantly affect the level of T cell activation. Generally, stronger T cell activation is observed on stiffer materials. (ii) Immune cell phenotype can be also affected by mechanical loading such as tensile, compressive and shear forces. Moderate cyclic strain can promote M2-like phenotype while higher cyclic strain triggered induction of M1-like macrophages. (iii) Biomaterial architecture and patterning can modulate cell shape and cytoskeletal organization, which impact the immune cell behavior. Macrophage elongated morphology induces M2-like polarization and reduces secretion of proinflammatory cytokines by these cells. Micropatterning can also affect T cell activation, for example, focal presentation of antibodies against CD3 and CD28 increases T cell activation. Microstructure of 3D scaffolds such as pore size and geometry affect immune cell infiltration and polarization. (B) Biomaterial composition. (i) Positively charged materials are more likely to trigger proinflammatory immune cell responses. (ii) Hydrophobic biomaterials tend to induce proinflammatory M1-like macrophage activation while hydrophilic or neutral surfaces create more anti-inflammatory microenvironment. (iii) Low molecular weight hyaluronic acid (LMW HA) fragments promote angiogenesis, high molecular weight HA have angiostatic properties, suppress M1-like polarization and promote Treg formation. (iv) Slowly degrading biomaterials induce prolonged proinflammatory reactions while scaffolds that degrade faster result in constructive tissue remodeling. (v) Release of bioactive ions: calcium signaling plays important role in the proinflammatory activation of macrophages and intracellular Ca2+ oscillations also occur in migrating ECs during capillary sprouting, on the contrary, calcium ion depletion leads to M2-like polarization. (vi) Biomaterials can change the pH of the microenvironment, which can contribute to the immune cell phenotypic changes, alkaline microenvironment can promote M1-like macrophage polarization while acidic pH polarizes macrophages into M2-like phenotype.
