Abstract
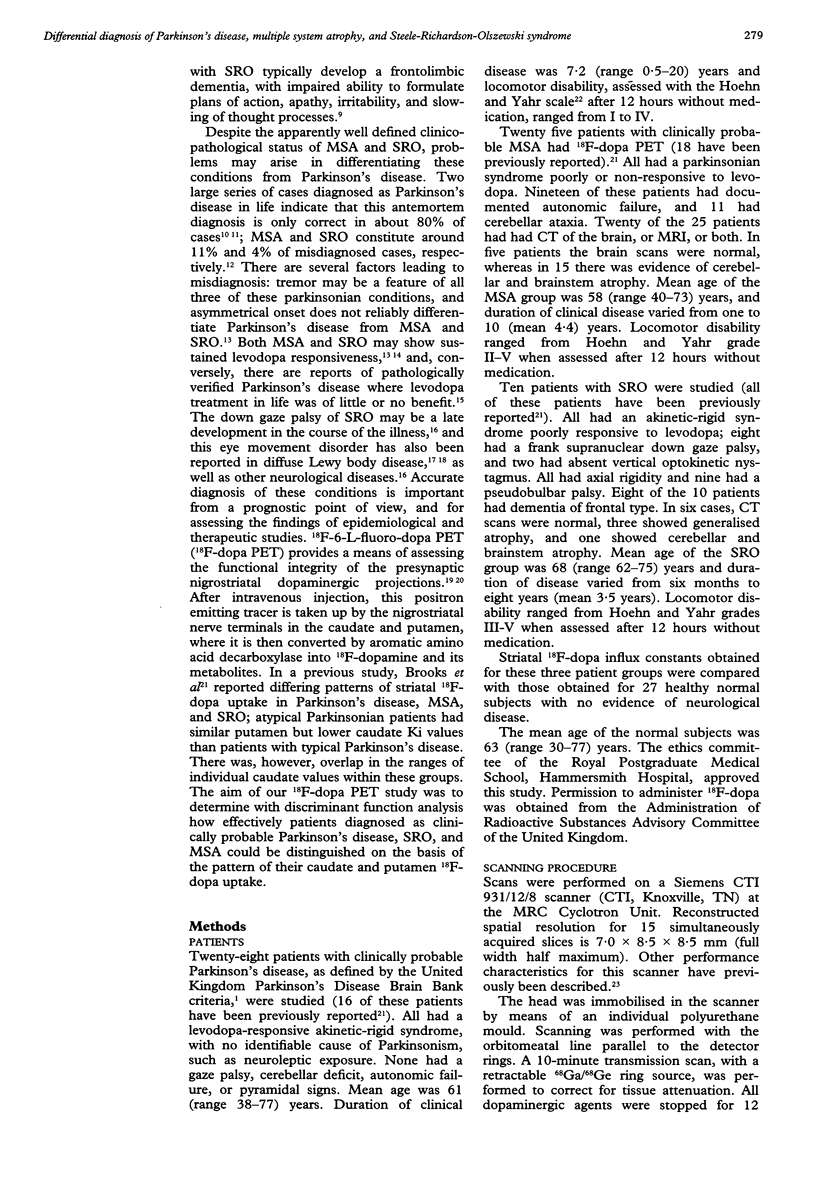
Clinicopathological series indicate that the clinical diagnosis of Parkinson's disease is correct in only 80% of cases. Multiple system atrophy (MSA) and Steele-Richardson-Olszewski syndrome (SRO) comprise most of the misdiagnoses. By means of 18F-dopa PET the pattern of nigrostriatal dopaminergic dysfunction in 28 patients with clinically probable Parkinson's disease, 25 with MSA, and 10 patients with SRO, was assessed and compared with the pattern in 27 normal subjects. Discriminant function analysis was used to assess the ability of 18F-dopa PET to categorize individual parkinsonian patients on the basis of their caudate and putamen tracer uptake. Discriminant function analysis assigned all control subjects a normal category. One Parkinsonian patient out of 63 was classified as "normal" on the basis of PET findings, although this patient had significantly reduced putamen 18F-dopa uptake. Discriminant function analysis was less effective at distinguishing different categories of akinetic-rigid syndrome on the basis of their striatal 18F-dopa uptake, as judged against clinical criteria. Patients clinically labelled as having typical or atypical Parkinsonian syndromes were assigned the same category on PET criteria 64% and 69% of the time, respectively. When all three categories of Parkinson's disease, MSA, and SRO were considered together, clinical and 18F-dopa PET findings correlated in 64% of patients assigned a diagnosis of Parkinson's disease and 70% of those given a diagnosis of SRO; MSA was less readily discriminated, patients with MSA being assigned to MSA, Parkinson's disease, and SRO groups with equal frequency. The correlation between clinical and discriminant function analysis assignment improved when separate comparisons were made between Parkinson's disease and MSA, or Parkinson's disease and SRO groups. In these analyses, clinical and PET categorisation of MSA and Parkinson's disease agreed in 60% of cases, and of SRO and Parkinson's disease in 90% of cases. In summary, (18)F-dopa PET successfully discriminates normal subjects from parkinsonian patients, and patients with Parkinson's disease from patients with SRO, but is less reliable in distinguishing Parkinson's disease from MSA. The concomitant assessment of striatal neuronal function with additional PET tracers may be necessary to reliably differentiate typical and atypical parkinsonian syndromes.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Albert M. L., Feldman R. G., Willis A. L. The 'subcortical dementia' of progressive supranuclear palsy. J Neurol Neurosurg Psychiatry. 1974 Feb;37(2):121–130. doi: 10.1136/jnnp.37.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernheimer H., Birkmayer W., Hornykiewicz O., Jellinger K., Seitelberger F. Brain dopamine and the syndromes of Parkinson and Huntington. Clinical, morphological and neurochemical correlations. J Neurol Sci. 1973 Dec;20(4):415–455. doi: 10.1016/0022-510x(73)90175-5. [DOI] [PubMed] [Google Scholar]
- Brooks D. J., Ibanez V., Sawle G. V., Quinn N., Lees A. J., Mathias C. J., Bannister R., Marsden C. D., Frackowiak R. S. Differing patterns of striatal 18F-dopa uptake in Parkinson's disease, multiple system atrophy, and progressive supranuclear palsy. Ann Neurol. 1990 Oct;28(4):547–555. doi: 10.1002/ana.410280412. [DOI] [PubMed] [Google Scholar]
- Brooks D. J., Salmon E. P., Mathias C. J., Quinn N., Leenders K. L., Bannister R., Marsden C. D., Frackowiak R. S. The relationship between locomotor disability, autonomic dysfunction, and the integrity of the striatal dopaminergic system in patients with multiple system atrophy, pure autonomic failure, and Parkinson's disease, studied with PET. Brain. 1990 Oct;113(Pt 5):1539–1552. doi: 10.1093/brain/113.5.1539. [DOI] [PubMed] [Google Scholar]
- Clark C. M., Ammann W., Martin W. R., Ty P., Hayden M. R. The FDG/PET methodology for early detection of disease onset: a statistical model. J Cereb Blood Flow Metab. 1991 Mar;11(2):A96–102. doi: 10.1038/jcbfm.1991.44. [DOI] [PubMed] [Google Scholar]
- De Volder A. G., Francart J., Laterre C., Dooms G., Bol A., Michel C., Goffinet A. M. Decreased glucose utilization in the striatum and frontal lobe in probable striatonigral degeneration. Ann Neurol. 1989 Aug;26(2):239–247. doi: 10.1002/ana.410260210. [DOI] [PubMed] [Google Scholar]
- Fearnley J. M., Lees A. J. Ageing and Parkinson's disease: substantia nigra regional selectivity. Brain. 1991 Oct;114(Pt 5):2283–2301. doi: 10.1093/brain/114.5.2283. [DOI] [PubMed] [Google Scholar]
- Fearnley J. M., Lees A. J. Striatonigral degeneration. A clinicopathological study. Brain. 1990 Dec;113(Pt 6):1823–1842. doi: 10.1093/brain/113.6.1823. [DOI] [PubMed] [Google Scholar]
- Fearnley J. M., Revesz T., Brooks D. J., Frackowiak R. S., Lees A. J. Diffuse Lewy body disease presenting with a supranuclear gaze palsy. J Neurol Neurosurg Psychiatry. 1991 Feb;54(2):159–161. doi: 10.1136/jnnp.54.2.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett E. S., Firnau G., Nahmias C. Dopamine visualized in the basal ganglia of living man. Nature. 1983 Sep 8;305(5930):137–138. doi: 10.1038/305137a0. [DOI] [PubMed] [Google Scholar]
- Gibb W. R., Lees A. J. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry. 1988 Jun;51(6):745–752. doi: 10.1136/jnnp.51.6.745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham J. G., Oppenheimer D. R. Orthostatic hypotension and nicotine sensitivity in a case of multiple system atrophy. J Neurol Neurosurg Psychiatry. 1969 Feb;32(1):28–34. doi: 10.1136/jnnp.32.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoehn M. M., Yahr M. D. Parkinsonism: onset, progression and mortality. Neurology. 1967 May;17(5):427–442. doi: 10.1212/wnl.17.5.427. [DOI] [PubMed] [Google Scholar]
- Hughes A. J., Colosimo C., Kleedorfer B., Daniel S. E., Lees A. J. The dopaminergic response in multiple system atrophy. J Neurol Neurosurg Psychiatry. 1992 Nov;55(11):1009–1013. doi: 10.1136/jnnp.55.11.1009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes A. J., Daniel S. E., Kilford L., Lees A. J. Accuracy of clinical diagnosis of idiopathic Parkinson's disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry. 1992 Mar;55(3):181–184. doi: 10.1136/jnnp.55.3.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi K., Miyazu K., Katsukawa K., Fukutani Y., Mukai M., Nakamura I., Yamaguchi N., Matsubara R., Isaki K. Cytoskeletal protein abnormalities in patients with olivopontocerebellar atrophy--an immunocytochemical and Gallyas silver impregnation study. Neuropathol Appl Neurobiol. 1992 Jun;18(3):237–249. doi: 10.1111/j.1365-2990.1992.tb00786.x. [DOI] [PubMed] [Google Scholar]
- Maher E. R., Lees A. J. The clinical features and natural history of the Steele-Richardson-Olszewski syndrome (progressive supranuclear palsy). Neurology. 1986 Jul;36(7):1005–1008. doi: 10.1212/wnl.36.7.1005. [DOI] [PubMed] [Google Scholar]
- Mark M. H., Sage J. I., Dickson D. W., Schwarz K. O., Duvoisin R. C. Levodopa-nonresponsive Lewy body parkinsonism: clinicopathologic study of two cases. Neurology. 1992 Jul;42(7):1323–1327. doi: 10.1212/wnl.42.7.1323. [DOI] [PubMed] [Google Scholar]
- Nahmias C., Garnett E. S., Firnau G., Lang A. Striatal dopamine distribution in parkinsonian patients during life. J Neurol Sci. 1985 Jul;69(3):223–230. doi: 10.1016/0022-510x(85)90135-2. [DOI] [PubMed] [Google Scholar]
- Papp M. I., Kahn J. E., Lantos P. L. Glial cytoplasmic inclusions in the CNS of patients with multiple system atrophy (striatonigral degeneration, olivopontocerebellar atrophy and Shy-Drager syndrome). J Neurol Sci. 1989 Dec;94(1-3):79–100. doi: 10.1016/0022-510x(89)90219-0. [DOI] [PubMed] [Google Scholar]
- Patlak C. S., Blasberg R. G. Graphical evaluation of blood-to-brain transfer constants from multiple-time uptake data. Generalizations. J Cereb Blood Flow Metab. 1985 Dec;5(4):584–590. doi: 10.1038/jcbfm.1985.87. [DOI] [PubMed] [Google Scholar]
- Quinn N. Multiple system atrophy--the nature of the beast. J Neurol Neurosurg Psychiatry. 1989 Jun;Suppl:78–89. doi: 10.1136/jnnp.52.suppl.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajput A. H., Rozdilsky B., Rajput A. Accuracy of clinical diagnosis in parkinsonism--a prospective study. Can J Neurol Sci. 1991 Aug;18(3):275–278. doi: 10.1017/s0317167100031814. [DOI] [PubMed] [Google Scholar]
- Ruberg M., Javoy-Agid F., Hirsch E., Scatton B., LHeureux R., Hauw J. J., Duyckaerts C., Gray F., Morel-Maroger A., Rascol A. Dopaminergic and cholinergic lesions in progressive supranuclear palsy. Ann Neurol. 1985 Nov;18(5):523–529. doi: 10.1002/ana.410180503. [DOI] [PubMed] [Google Scholar]
- STEELE J. C., RICHARDSON J. C., OLSZEWSKI J. PROGRESSIVE SUPRANUCLEAR PALSY. A HETEROGENEOUS DEGENERATION INVOLVING THE BRAIN STEM, BASAL GANGLIA AND CEREBELLUM WITH VERTICAL GAZE AND PSEUDOBULBAR PALSY, NUCHAL DYSTONIA AND DEMENTIA. Arch Neurol. 1964 Apr;10:333–359. doi: 10.1001/archneur.1964.00460160003001. [DOI] [PubMed] [Google Scholar]
- Spokes E. G., Bannister R., Oppenheimer D. R. Multiple system atrophy with autonomic failure: clinical, histological and neurochemical observations on four cases. J Neurol Sci. 1979 Sep;43(1):59–82. doi: 10.1016/0022-510x(79)90073-x. [DOI] [PubMed] [Google Scholar]
- de Bruin V. M., Lees A. J., Daniel S. E. Diffuse Lewy body disease presenting with supranuclear gaze palsy, parkinsonism, and dementia: a case report. Mov Disord. 1992 Oct;7(4):355–358. doi: 10.1002/mds.870070410. [DOI] [PubMed] [Google Scholar]


