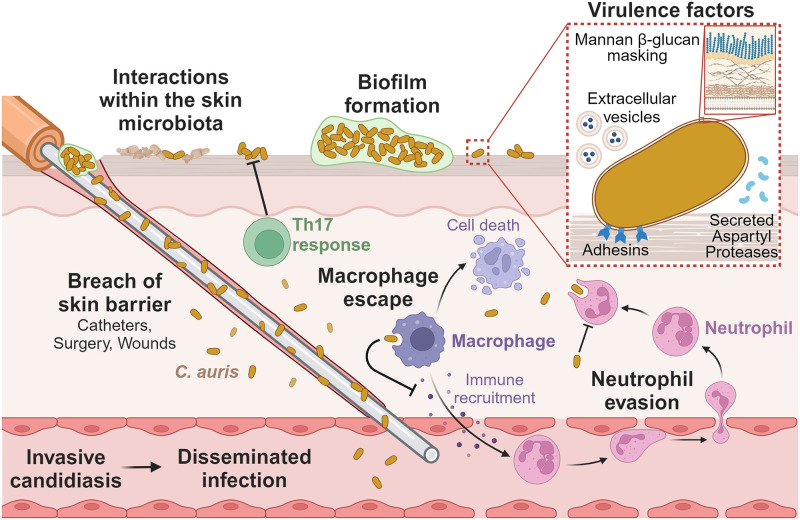
Fig 1. Candida auris mechanisms of pathogenesis.
C. auris colonizes and persists on the skin, and breaches of the skin barrier can lead to invasive candidiasis and hematogenous spread of infection. Interactions with other skin microbiota (e.g., Malassezia spp., Klebsiella pneumoniae, Staphylococcus hominis) influence the growth of C. auris on the skin. Biofilm formation of C. auris increases resistance to antimicrobial treatment on the skin surface. C. auris produces multiple virulence factors to release into the surrounding microenvironment including SAPs and EVs. Adhesins promote attachment to the skin surface, and mannans in the cell wall mask β-glucans from PRRs on immune cells. C. auris evades neutrophil recognition and phagocytosis. C. auris escapes macrophage killing, inhibits macrophage-mediated immune recruitment, and induces macrophage cell death. In contrast, the Th17 T-cell response inhibits C. auris skin colonization. The figure was designed using Biorender. EV, extracellular vesicle; PRR, pathogen recognition receptor; SAP, secreted aspartyl protease.