Abstract
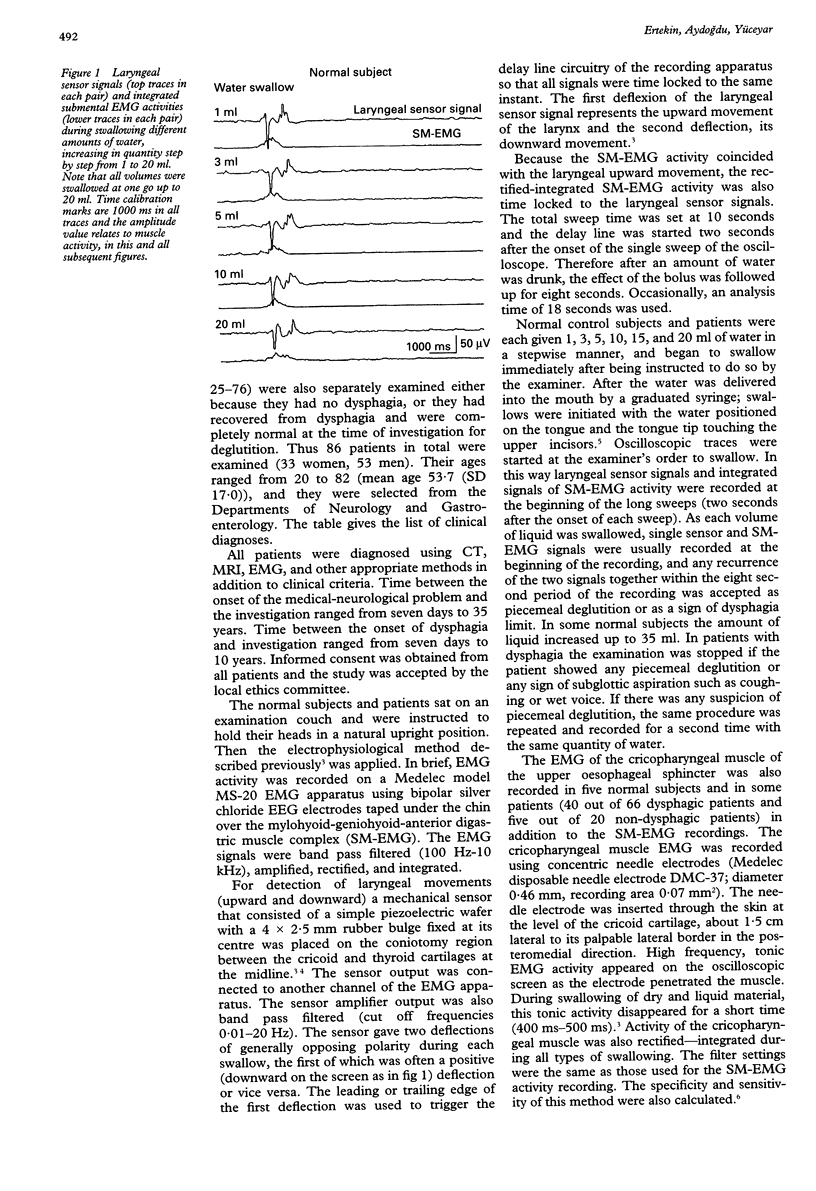
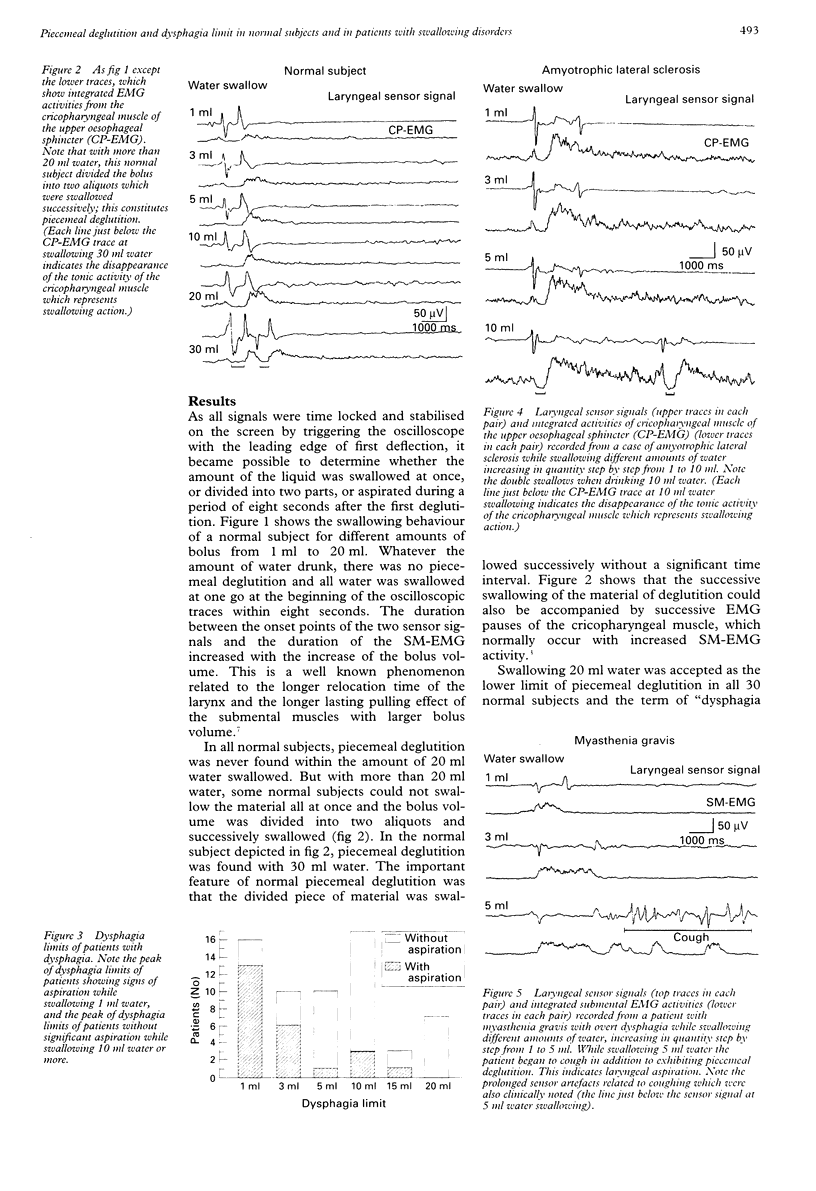
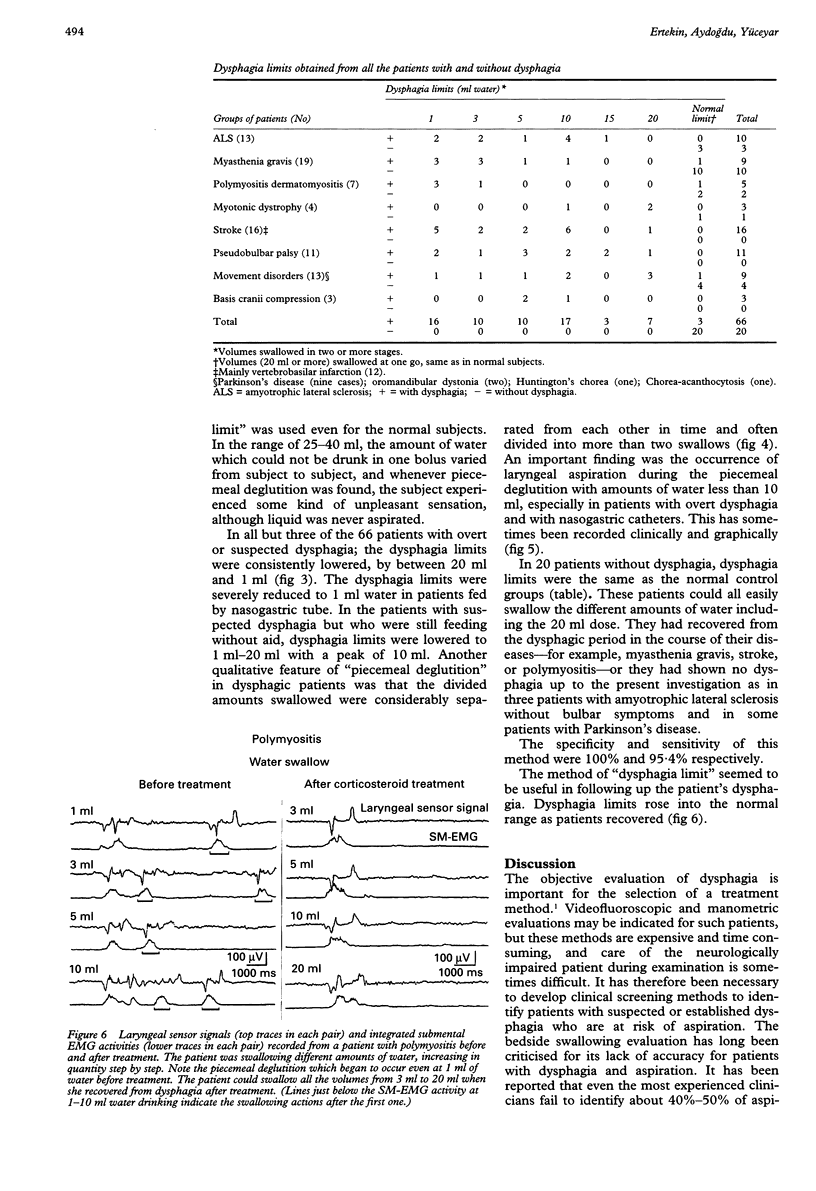
OBJECTIVE: Before the advanced evaluation of deglutition and selection of a treatment method, objective screening methods are necessary for patients with dysphagia. In this study a new electroclinical test was established to evaluate patients with dysphagia. METHODS: This test is based on determining piecemeal deglutition; which is a physiological phenomenon occurring when a bolus of a large volume is divided into two or more parts which are swallowed successively. The combined electrophysiological and mechanical method used to record laryngeal movements detected by a piezoelectric transducer, and activities of the related submental integrated EMG (SM-EMG)-and sometimes the cricopharyngeal muscle of the upper oesophageal sphincter (CP-EMG)-were performed during swallowing. Thirty normal subjects and 66 patients with overt dysphagia of neurogenic origin were investigated after detailed clinical evaluation. Twenty patients with a potential risk of dysphagia, but who were normal clinically at the time of investigation, were also evaluated to determine the specificity of the test. All subjects were instructed to swallow doses of water, gradually increasing in quantity from 1 ml to 20 ml, and any recurrence of the signals related to swallowing within the eight seconds was accepted as a sign of dysphagia limit. RESULTS: In normal subjects as well as in the patients without dysphagia, piecemeal deglutition was never seen with less than 20 ml water. This volume was therefore accepted as the lower limit of piecemeal deglutition. In patients with dysphagia, dysphagia limits were significantly lower than those of normal subjects. CONCLUSION: The method is a highly specific and sensitive test for the objective evaluation of oropharyngeal dysphagia even in patients with suspected dysphagia of neurogenic origin. It can also be safely and simply applied in any EMG laboratory.
Full text
PDF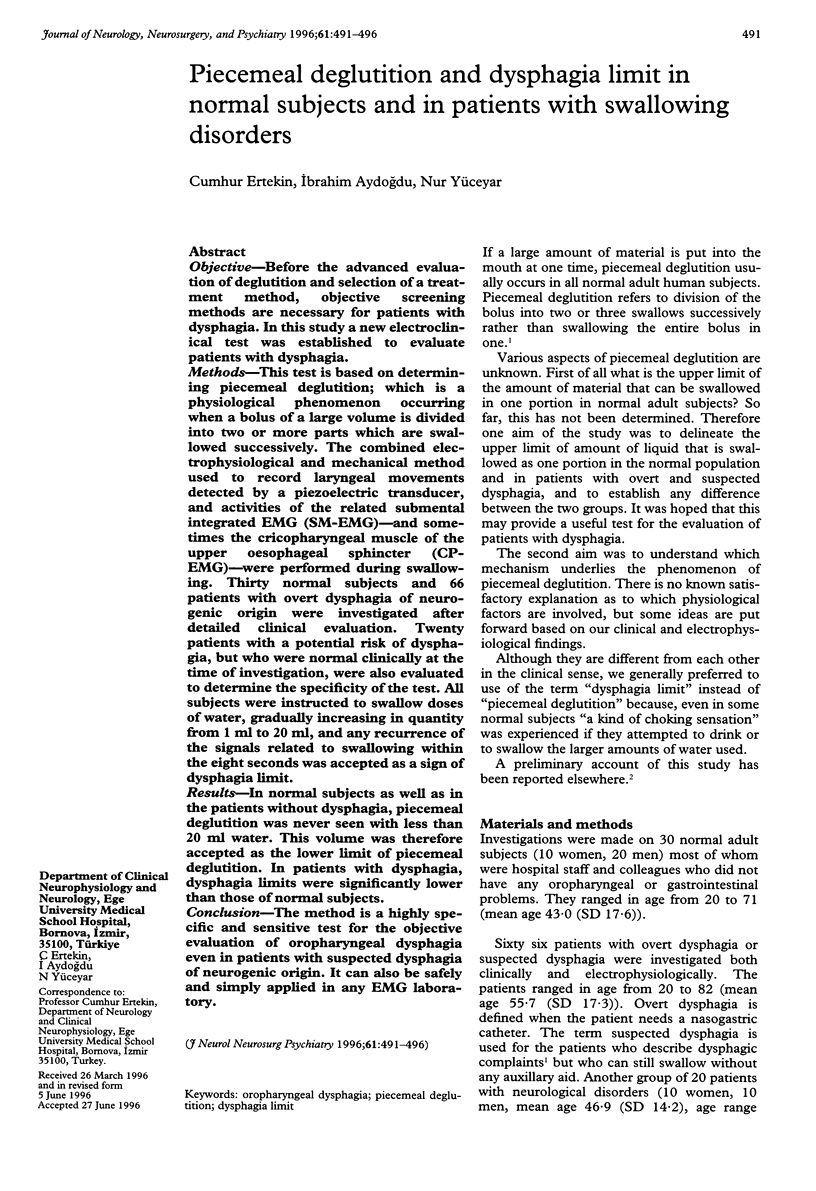
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Buchholz D. W., Bosma J. F., Donner M. W. Adaptation, compensation, and decompensation of the pharyngeal swallow. Gastrointest Radiol. 1985;10(3):235–239. doi: 10.1007/BF01893106. [DOI] [PubMed] [Google Scholar]
- Dantas R. O., Kern M. K., Massey B. T., Dodds W. J., Kahrilas P. J., Brasseur J. G., Cook I. J., Lang I. M. Effect of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol. 1990 May;258(5 Pt 1):G675–G681. doi: 10.1152/ajpgi.1990.258.5.G675. [DOI] [PubMed] [Google Scholar]
- DePippo K. L., Holas M. A., Reding M. J. Validation of the 3-oz water swallow test for aspiration following stroke. Arch Neurol. 1992 Dec;49(12):1259–1261. doi: 10.1001/archneur.1992.00530360057018. [DOI] [PubMed] [Google Scholar]
- Hughes T. A., Wiles C. M. Clinical measurement of swallowing in health and in neurogenic dysphagia. QJM. 1996 Feb;89(2):109–116. doi: 10.1093/qjmed/89.2.109. [DOI] [PubMed] [Google Scholar]
- JONES D. V., WORK C. E. Volume of a swallow. Am J Dis Child. 1961 Sep;102:427–427. doi: 10.1001/archpedi.1961.02080010429023. [DOI] [PubMed] [Google Scholar]
- Jacob P., Kahrilas P. J., Logemann J. A., Shah V., Ha T. Upper esophageal sphincter opening and modulation during swallowing. Gastroenterology. 1989 Dec;97(6):1469–1478. doi: 10.1016/0016-5085(89)90391-0. [DOI] [PubMed] [Google Scholar]
- Jones B., Ravich W. J., Donner M. W., Kramer S. S., Hendrix T. R. Pharyngoesophageal interrelationships: observations and working concepts. Gastrointest Radiol. 1985;10(3):225–233. doi: 10.1007/BF01893105. [DOI] [PubMed] [Google Scholar]
- Kahrilas P. J., Dodds W. J., Dent J., Logemann J. A., Shaker R. Upper esophageal sphincter function during deglutition. Gastroenterology. 1988 Jul;95(1):52–62. doi: 10.1016/0016-5085(88)90290-9. [DOI] [PubMed] [Google Scholar]
- Kahrilas P. J., Lin S., Logemann J. A., Ergun G. A., Facchini F. Deglutitive tongue action: volume accommodation and bolus propulsion. Gastroenterology. 1993 Jan;104(1):152–162. doi: 10.1016/0016-5085(93)90847-6. [DOI] [PubMed] [Google Scholar]
- Kahrilas P. J., Logemann J. A. Volume accommodation during swallowing. Dysphagia. 1993;8(3):259–265. doi: 10.1007/BF01354548. [DOI] [PubMed] [Google Scholar]
- Miller A. J. Deglutition. Physiol Rev. 1982 Jan;62(1):129–184. doi: 10.1152/physrev.1982.62.1.129. [DOI] [PubMed] [Google Scholar]
- Nirkko A. C., Rösler K. M., Hess C. W. Sensitivity and specificity of needle electromyography: a prospective study comparing automated interference pattern analysis with single motor unit potential analysis. Electroencephalogr Clin Neurophysiol. 1995 Feb;97(1):1–10. doi: 10.1016/0924-980x(94)00248-6. [DOI] [PubMed] [Google Scholar]
- Seamen W. B. Pharyngeal and upper esophageal dysphagia. JAMA. 1976 Jun 14;235(24):2643–2646. doi: 10.1001/jama.235.24.2643. [DOI] [PubMed] [Google Scholar]


