Abstract
Treatment of chronic patellar tendon ruptures represents a real challenge for orthopaedic surgeons. The superior patellar migration and the pathological aspect of the tendon are the two conditions that aggravate the situation. Several reconstruction methods have been described in the literature. Hamstring tendon augmentation using horizontal patellar tunnel is widely used in such cases. However, underuse of longitudinal patellar tunnels, although they reproduce the native footprint of the patellar tendon insertion, highlights a missed opportunity in chronic patellar tendon rupture reconstruction. In the current article, we describe a semitendinosus tendon autograft reconstruction technique where the patellar tunnels are drilled longitudinally instead of being drilled transversely from medial to lateral. At 34 months follow-up, our patient claimed full active knee mobility with good quadriceps strength. Reproducing the native footprint of the patellar tendon insertion, through longitudinal patellar tunnels, leads to optimal outcomes after chronic patellar tendon rupture reconstruction with Semitendinosus Autograft.
Keywords: Chronic patellar tendon rupture, Semitendinosus tendon, Autografting, Patellar tendon reconstruction
Introduction
Rupture of the patella tendon may be experienced after severe traumatic injury among the young population, or due to repetitive microtrauma in the elderly population when the tendon is of poor quality. Management of chronic patellar tendon rupture can be achieved either by an allograft of the Achilles tendon, or by autografts such as contralateral bone -patellar tendon -bone graft or semitendinosus and gracilis graft. Hamstring tendon autografts have biomechanical properties close to those of the native extensor apparatus and are widely used to reconstruct the patellar tendon [1]. Commonly, hamstring grafts are passed transversely through the patella. In the present case, we describe a more anatomical technique using the semitendinosus graft, passed longitudinally through the patella, to better fit the anatomy.
Case report
A 42-year-old male, after neglecting a fall on his knee from his motorcycle for 5 months, presented with a deficit of active knee extension. On examination, there was no skin lesion, passive range of motion ranges from 0 to 140° with an active knee extension deficit of 20°, and there was a depression under the patella (Fig. 1).
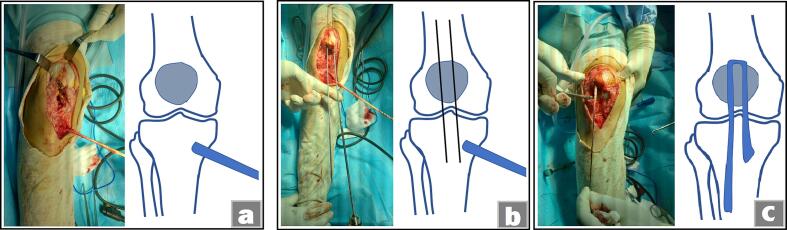
Fig. 1.
Pre-operative presentation with proximal migration of the patella along with an infrapatellar void.
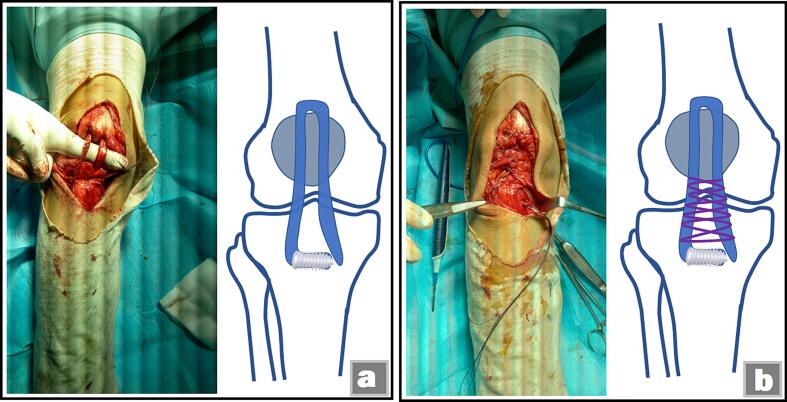
Lateral radiographs of the knee showed a patella Alta with Insall-Salvati ratio of 1.82. There was no fracture. MRI confirmed the total disruption of the patellar tendon. The patient underwent anterior knee surgery using a mid-line incision. Intraoperatively, patellar tendon was lacerated. Surgical technique consisted of an augmentation loop with the ipsilateral semitendinosus tendon. The Semitendinosus tendon was harvested, through the same incision, and left attached to the medial aspect of the tibia. The distal end of the semitendinosus was fixed with tractor wires. Three tunnels were created, guided by wires, using a drill bit with a diameter adapted to the diameter of the graft (4.5-mm). Thus, two parallel longitudinal tunnels were drilled in the patella and one transverse tunnel in the tibia tuberosity (Fig. 2a, b). Once the tunnels are prepared, the graft is passed through the first internal patellar tunnel then turned over and passed through the external patellar tunnel and finally transversely through the tibial tunnel (Fig. 2c). Adjusting the tension on the graft allows the patella to be lowered and to choose the correct fixation position. The fixation of the distal end of the semitendinosus is carried out using an interference screw. Finally, the two semitendinosus strands, used for the reconstruction, were sutured to each other (Fig. 3). Postoperatively, the patient begins an early, gentle and progressive rehabilitation. During the first 2 weeks, the knee was immobilized in a hinged knee brace, limiting motion from 0 to 45°. During this period, only active flexion was allowed, while extension was passive. The arc of range of motion was gradually increased by an additional 15° per week until full range of motion was achieved. Active extension was started at 6 weeks, and the brace was discontinued at 12 weeks when quadriceps strength was adequate. At 34 months follow-up, the patient claimed full active knee mobility with good quadriceps strength.
Fig. 2.
Intra-operative photo and schematic representation showing: (a) the harvesting of the semitendinosus tendon, (b) the realization of the two longitudinal tunnels in the patella and (c) showing the passage of the graft as a loop.
Fig. 3.
Intra-operative photo and schematic representation showing (a) graft fixation with an interference screw and (b) the final aspect of the construction.
Discussion
Patellar tendon rupture may result from a severe acute injury or from chronic degeneration of the patellar tendon due to repetitive stress. Untreated, chronic patellar tendon rupture can lead to knee impairment including chronic pain, stiffness and loss of function.
The reconstruction of a chronic rupture poses many problems: (1) what type of tendon graft to choose for the reconstruction? (2) what are the best positions of the tunnels? (3) how to fix the graft? and (4) how to restore patella height.
Direct tendon-to-tendon repair with suture anchors or trans-osseous sutures can be challenging due to tissue retraction and poor tendon quality [1]. To enhance stability and protect the suture, this direct repair can be reinforced by augmentation with semitendinosus tendon autograft [2]. Nevertheless, direct suturing is rarely used, and tendon injury is commonly repaired by tendon reconstruction.
Several methods of tendon reconstruction have been proposed in the literature. Reconstructions using the Achilles Tendon Allograft technique with calcaneal bone block have the advantage of a solid reconstruction but carry a risk of viral and bacterial infections transmission and are reserved for revision or when the autograft cannot be used [3].
Reconstruction with a contralateral bone-patellar tendon-bone graft has the advantage of automatically reproducing the same patellar height as the contralateral knee and increases the rate of graft consolidation through the graft bone blocks [3].
Semitendinosus autograft reconstruction remains the most popular technique. The grafts are passed through an oblique tunnel in the tibial tuberosity and through transverse tunnel on the patella [4,5]. To reproduce a normal patellar height, the distance between the patella and the tibial tuberosity should be equal to the length of the patella.
In the technique described in our case, the patellar tunnels are drilled longitudinally, and not transversely, as described with acute tendon repair [6] to feat the anatomic footprint of the patellar tendon and optimize the patellar tracking. However, care should be taken that the patellar tunnels are not very close together so that they do not communicate with each other. A one cm distance between the two tunnels is to be respected. Likewise, given the risk of patellar weakening, it is important to pay attention to the osteoporotics patellas of elderly patients and to patellas that have previously undergone surgery.
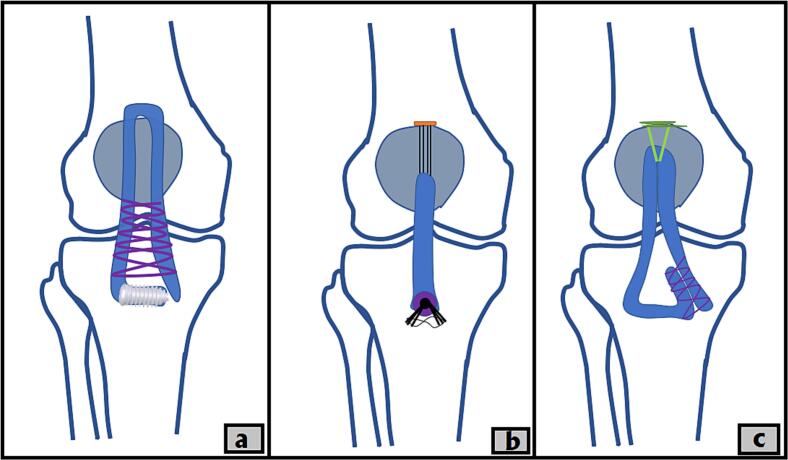
Valianatos et al [7] described a similar technique using the semitendinosus and gracilis as free grafts, folded to create a double construct, passed through a single longitudinal patellar tunnel, and fixed with an endobutton device. The same procedure was used by Ovigue with an endobutton at each end of the graft [8]. In the same spirit, Abdel-Aziz et al [9] proposed a reconstruction thought a blind vertical patellar tunnel using a looped semitendinosus over 2 ETHIBOND sutures.
Our method differs from the previous techniques by the fact that two tunnels were drilled in the patella to pass the graft as a loop, allowing solid anchorage without the need for additional patellar fixation (Fig. 4). Furthermore, the preservation of tendon vascularization is ensured by leaving the graft attached to the tibia, which constitutes the second advantage [10]. Our belief is that reproducing the anatomical footprint of the patellar tendon through longitudinal tunnels allows for more efficient force distribution and reduces stress on the quadriceps muscle.
Fig. 4.
Schematic representation showing (a) our reconstruction method compared to that of Valianatos et al. (b) and to that of Abdel-Aziz et al. (c).
Conclusion
Reconstruction of chronic patellar tendon ruptures using the ipsilateral semitendinosus tendon passed longitudinally through the patella, mimicking the native tendon, appears to be an anatomical method that preserves the kinetics and biomechanics of the patellofemoral joint.
CRediT authorship contribution statement
Aymen Ben Fredj: contributed to writing and editing of the manuscript.
Hedi Rbai: contributed to supervision and validation.
Farouk Chatbouri: contributed to the clinical data collection and writing the case report.
Marouene Berriri: contributed to writing the manuscript.
Abderrahmen Daadoucha: contributed to the design of the case report presentation.
Anouar Boughattas: performed the final revision of the manuscript.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed consent
Informed consent was obtained from the participant included in the study.
Consent to publish
The participant gave their informed consent for the publication of all the figures and data.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics statement
This clinical case report is the authors' own original work, which has not been previously published elsewhere.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgments
None.
Footnotes
A written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Data availability
Not applicable.
References
- 1.Carlson Strother C.R., LaPrade M.D., Keyt L.K., Wilbur R.R., Krych A.J., Stuart M.J. A strategy for repair, augmentation, and reconstruction of knee extensor mechanism disruption: a retrospective review. Orthop. J. Sports Med. 2021;9(10) doi: 10.1177/23259671211046625. (23259671211046625) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dejour H., Denjean S., Neyret P. Traitement des ruptures anciennes ou itératives du ligament patellaire par auto-greffe controlatérale [treatment of old or recurrent ruptures of the patellar ligament by contralateral autograft] Rev. Chir. Orthop. Reparatrice Appar. Mot. 1992;78(1):58–62. (in French) [PubMed] [Google Scholar]
- 3.Nguene-Nyemb A.G., Huten D., Ropars M. Chronic patellar tendon rupture reconstruction with a semitendinosus autograft. Orthop. Traumatol. Surg. Res. 2011;97(4):447–450. doi: 10.1016/j.otsr.2011.01.015. [DOI] [PubMed] [Google Scholar]
- 4.Rocha de Faria J.L., de Barros Carvalho M., Marques A.C., Cavanellas N.T., Branco de Sousa E., Barretto J.M., et al. Surgical treatment for chronic rupture of the patellar tendon performed in 2 stages. Arthrosc. Tech. 2019;9(1):e159–e166. doi: 10.1016/j.eats.2019.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu Q., Tang D., Zhu W., Chen Y. Patellar tendon reconstruction using autologous hamstring tendons for the treatment of extensive patellar tendon ossification. Orthop. Surg. 2022;14(11):3119–3124. doi: 10.1111/os.13435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Imbergamo C., Sequeira S., Bano J., Rate W.R., 4th, Gould H. Failure rates of suture anchor fixation versus transosseous tunnel technique for patellar tendon repair: a systematic review and meta-analysis of biomechanical studies. Orthop. J. Sports Med. 2022;10(8) doi: 10.1177/23259671221120212. (23259671221120212) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valianatos P., Papadakou E., Erginoussakis D., Kampras D., Schizas N., Kouzoupis A. Treatment of chronic patellar tendon rupture with hamstrings tendon autograft. J. Knee Surg. 2020;33(8):792–797. doi: 10.1055/s-0039-1688499. [DOI] [PubMed] [Google Scholar]
- 8.Ovigue J., Graveleau N., Bouguennec N. Patellar tendon reconstruction using hamstring tendon and adjustable suspensory cortical fixation. Arthrosc. Tech. 2019;8(7):e679–e683. doi: 10.1016/j.eats.2019.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abdel-Aziz A., Abdelrazek B.H.M.Z., Waly M.R., Abdel-Aziz M.A., El Din Salah, Sheriff M.M. Technique for fixation of semitendinosus to the Patella in patellar tendon reconstruction. Arthrosc. Tech. 2020;9(12):e1943–e1949. doi: 10.1016/j.eats.2020.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Takazawa Y., Ikeda H., Ishijima M., et al. Reconstruction of a ruptured patellar tendon using ipsilateral semitendinosus and gracilis tendons with preserved distal insertions: two case reports. BMC. Res. Notes. 2013;6:361. doi: 10.1186/1756-0500-6-361. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.