Dear Editor,
Immunoglobulin A (IgA) vasculitis is an immune complex vasculitis that affects small vessels with dominant IgA deposits.[1] Drugs could be potential triggers of the disease.[2] Thalidomide has been used as an immunomodulator and anti-inflammatory agent for treating multiple conditions. IgA vasculitis is an extremely rare complication of thalidomide therapy.[3,4]
A 61-year-old male with a history of type II diabetes, bipolar affective disorder, hypothyroidism, and hypertension presented with a burning sensation and swelling over both legs. His serum creatinine level was 2.74 mg/dl. His renal biopsy was suggestive of proliferative glomerulonephritis with monoclonal immunoglobulin deposition disease. Bone marrow examination revealed 11% CD138-positive plasma cells. He underwent four cycles of chemotherapy (CyBorD protocol) followed by autologous stem cell transplantation. His creatinine level was stable at around 2.5 mg/dl. The patient was started on thalidomide 100 mg once daily. Six months later, he developed palpable purpuric rashes in both lower limbs. His creatinine level increased to 4.8 mg/dl, and a urine examination revealed new onset hematuria and increased proteinuria.
Skin biopsy showed perivascular inflammatory infiltrates of lymphocytes and eosinophils in the dermis with features of leukocytoclasis and Red blood cell exocytosis along with IgA deposits on immunofluorescence [Figures 1 and 2]. Antinuclear antibodies, antineutrophil cytoplasmic antibodies, complement levels, and anti–double stranded DNA (anti-dsDNA) were within normal range; hepatitis B, hepatitis C, and human immunodeficiency virus serologies were negative. Bone marrow biopsy and flow cytometry ruled out myeloma recurrence. Having a strong suspicion of drug-induced vasculitis, we stopped thalidomide, and the patient was commenced on steroids. On follow-up, his creatinine level declined to 2.5 mg/dl, hematuria and proteinuria subsided, and skin lesions receded. The patient is currently on 10 mg of prednisolone, and thalidomide was changed to bortezomib.
Figure 1.
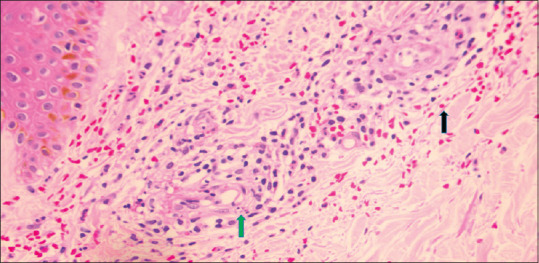
Hematoxylin and eosin (H&E) microphotograph. H&E microphotograph shows skin with unremarkable epidermis (left upper corner) superficial dermal blood vessels with significant neutrophilic, lymphocytic perivascular infiltrate associated with leucocytoclasis (green arrow) and RBC exocytosis (black arrow. Hematoxylin & Eosin stained section (40X).
Figure 2.

Direct immunofluorescence (DIF) with IgA showing small vessel deposition of IgA immune complexes seen as fluorescence (red arrow)
The clinical characteristics of drug-related IgA vasculitis is purpura in nearly 100% of patients, joint involvement in half of them, and gastrointestinal and renal involvement in nearly one-third. The possibility of other small-vessel vasculitis was ruled out as his immunologic and serologic workup were negative. 2-5% cases of vasculitis is related to cancer and majority are related to haematological malignancies.[5] Paraneoplastic Henoch-Schönlein purpura (HSP) should be suspected when IgA nephropathy is associated with necrotic skin lesions without cryoglobulin. There is no unique clinical, pathological, or laboratory marker to differentiate drug-induced vasculitis from another vasculitis. However, considering the clinical circumstances and the patient’s response to drug withdrawal, thalidomide-induced IgA vasculitis was the most definitive diagnosis in this case. To the best of our knowledge, this is the first reported case of IgA vasculitis related to thalidomide. Further epidemiological studies are required to ascertain whether there is a real link between IgA vasculitis and thalidomide.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Audemard-Verger A, Pillebout E, Guillevin L, Thervet E, Terrier B. IgA vasculitis (Henoch-Shönlein purpura) in adults:Diagnostic and therapeutic aspects. Autoimmun Rev. 2015;14:579–85. doi: 10.1016/j.autrev.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 2.Rigante D, Castellazzi L, Bosco A, Esposito S. Is there a crossroad between infections, genetics, and Henoch–Schönlein purpura? Autoimmun Rev. 2013;12:1016–21. doi: 10.1016/j.autrev.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 3.Yildirim ND, Ayer M, Küçükkaya RD, Alpay N, Mete O, Yenerel MN, et al. Leukocytoclastic vasculitis due to thalidomide in multiple myeloma. Jpn J Clin Oncol. 2007;37:704–7. doi: 10.1093/jjco/hym092. [DOI] [PubMed] [Google Scholar]
- 4.Neben K, Moehler T, Benner A, Kraemer A, Egerer G, Ho AD, et al. Dose-dependent effect of thalidomide on overall survival in relapsed multiple myeloma. Clin Cancer Res. 2002;8:3377–82. [PubMed] [Google Scholar]
- 5.Hetland L, Susrud K, Lindahl K, Bygum A. Henoch-Schönlein purpura:A literature review. Acta Derm Venereol. 2017;97:1160–6. doi: 10.2340/00015555-2733. [DOI] [PubMed] [Google Scholar]


