Abstract
Background and Hypothesis
Childhood adversity is associated with a myriad of psychiatric symptoms, including psychotic experiences (PEs), and with multiple psychological processes that may all mediate these associations.
Study Design
Using a network approach, the present study examined the complex interactions between childhood adversity, PEs, other psychiatric symptoms, and multiple psychological mediators (ie, activity-related and social stress, negative affect, loneliness, threat anticipation, maladaptive cognitive emotion regulation, attachment insecurity) in a general population, adolescent sample (n = 865, age 12–20, 67% female).
Study Results
Centrality analyses revealed a pivotal role of depression, anxiety, negative affect, and loneliness within the network and a bridging role of threat anticipation between childhood adversity and maladaptive cognitive emotion regulation. By constructing shortest path networks, we found multiple existing paths between different categories of childhood adversity and PEs, with symptoms of general psychopathology (ie, anxiety, hostility, and somatization) as the main connective component. Sensitivity analyses confirmed the robustness and stability of the networks. Longitudinal analysis in a subsample with Wave 2 data (n = 161) further found that variables with higher centrality (ie, depression, negative affect, and loneliness) better predicted follow-up PEs.
Conclusions
Pathways linking childhood adversity to PEs are complex, with multifaceted psychological and symptom-symptom interactions. They underscore the transdiagnostic, heterotypic nature of mental ill-health in young people experiencing PEs, in agreement with current clinical recommendations.
Keywords: childhood adversity, psychotic experiences, network analysis, adolescents
Introduction
Psychotic experiences (PEs) are common in the general population,1 with highest pooled incidence rate (ie, 5 per 100) and persistence rate (ie, 35.8%) in adolescence.2 Although PEs are transient for most people, about 20% develop persistent PEs and 7% go on to develop a psychotic disorder,3 suggesting a phenomenological and temporal continuity between PEs and psychotic disorders. Particularly, the typical onset of primary psychotic disorders is in the teens to mid-twenties,4 stressing the importance of understanding emerging PEs in adolescence.
Childhood adversity is robustly associated with the development of PEs across this continuum, extending from low-level experiences to a full-blown psychotic disorder.5–10 Extensive literature shows that exposure to adversity in childhood may contribute to an enduring liability to PEs by impacting on affective and cognitive processes, as well as dysfunctional attachment.11–22 Indeed, PEs are associated with enhanced threat anticipation,23,24 maladaptive cognitive emotion regulation,25 dysfunctional attachment,26,27 elevated emotional reactions to daily life stressors23,24,28,29 and comorbid psychopathology,30 characteristics that have also been repeatedly reported in individuals with a history of childhood adversity.17,21,22,31–34 Evidence in fact suggests that negative affect in daily life,31 as well as feelings of loneliness,21 emotional symptoms (eg, anxiety and depression),21,22,35 emotional dysregulation,21,36,37 enhanced threat anticipation,31 and attachment insecurity,21 may all mediate the association between childhood adversity and PEs.
Importantly however, these different psychological mediators do not act independently, but are mutually interrelated.15,18,38 For instance, the effect of stress on PEs is mediated by negative affect in daily life and threat anticipation23; attachment insecurity is associated with altered behavioral and neural patterns of emotion regulation39; and threat anticipation, maladaptive cognitive emotion regulation, and attachment insecurity are all related to general psychopathology.32,40–43 Thus, apparently, pathways linking childhood adversity to PEs are complex, with multifaceted psychological and symptom-symptom interactions. The identification of key mediators, as well as understanding the interplay among these different factors, is crucial to develop the most effective intervention and prevention strategies. To this end, it is necessary to systematically map and test the full complexity of etiological pathways. A network approach may be best suited for this purpose.44–46
The network theory conceptualizes mental disorders as complex systems, in which the causal interactions between symptoms themselves constitute the disorder.44 For instance, Fried et al45 compared 2 hypotheses about the effects of loss (ie, bereavement) on depressive symptoms and found that, instead of being mediated through a latent variable, these effects could be better explained via a network perspective: loss mainly affected the symptom loneliness, which in turn was correlated to other symptoms. Symptoms with such a key role in a network are referred to as central symptoms, as these symptoms may potentially induce other symptoms, whereas decreasing them may help to resolve the whole symptom network. In a longitudinal study with 501 healthy adults, Boschloo et al46 prospectively examined the onset of DSM-IV major depressive disorder after a 2-, 4-, and 6-year follow-up. The authors found that symptoms with the highest centrality (ie, strength centrality) at baseline, such as loss of interest, fatigue, depressed mood, and concentration problems, strongly predicted the onset of major depressive disorder, whereas symptoms with lowest centrality (such as a decrease in weight/appetite, hypersomnia, and suicidal thoughts) were not or only weakly predictive. Thus, early intervention strategies targeting central symptoms in particular hold considerable promise in terms of prevention and treatment success.
In a hallmark study, Isvoranu et al used network analysis to examine the pathways linking childhood adversity and negative and positive psychotic symptoms in a sample of adult patients with a psychotic disorder.35 The authors found that distinct adversity types and psychotic symptoms were connected via general psychopathology, with anxiety as a major connective component. Important gaps in knowledge still remain, however. First, it is unknown how these complex interactions evolve in the early stages of emerging PEs, ie, in adolescence, where they have the highest pooled incidence and persistence rate2 and can be studied free from the biases of treatment, illness progression, or perceived stigma. Second, no study so far has examined the role, centrality and interplay of psychological processes such as stress in daily life, negative affect, feeling of loneliness, threat anticipation, maladaptive cognitive emotion regulation, attachment insecurity, as well as general psychopathology, which are closely associated with PEs and exposure to adversity. The current study therefore aimed to map the complex network linking childhood adversity and PEs by including key psychological mediators in a community sample of adolescents between 12 and 20 years old.
Methods
This study has been post-registered on the Open Science Framework (OSF, https://osf.io/ygchd). Formal analyses deviated from the registered analyses: (1) loneliness was included as a separate variable instead of ascribing it to negative affect as in previous studies, which have demonstrated the mediating role of loneliness between childhood adversity and PEs21,47; (2) we did not include the global severity index score, but the subdimensions of the 53-item Brief Symptom Inventory48 to investigate the mediating role of different categories of psychopathology; (3) we included 4, instead of 9, cognitive emotion regulation strategies, since these 4 have been associated the most with psychopathological symptoms43,49,50; (4) we scored childhood adversity by summing up the items within each module instead of coding each module as binary data (ie, yes or no) to better capture the degree of exposure, consequently, a Gaussian graphical model (GGM) using extended Bayesian information criterion (EBIC), rather than a Mixed Graphical Model using cross validation, was fitted to the data. The R codes used in this manuscript are provided on OSF (https://osf.io/8urg5/).
Participants
The sample used in the current article pertain to the first wave (29/1/2018–3/6/2019) of the SIGMA study.51 1913 adolescents were recruited through 22 mainstream secondary schools (first year = 1048, third year = 424, fifth year = 441) across all 5 provinces in Flanders, Belgium. Our main measure of PEs in this sample is the Prodromal Questionnaire-16 (PQ-16),52,53 since it has good internal consistency in both adolescent help-seeking and general populations.54,55 The PQ-16 was omitted for first-year students following data collection from the first school, as it became clear that the first-year students were unable to complete the full questionnaire battery within the time allowed for the testing session. This resulted in a final sample of 865 adolescents. Written informed consent was obtained from participants and their parents/caregivers prior to the participation. UZ/KU Leuven Medical Ethics Committee has approved this study (number S61395).
Measures
In the present study, we integrated classical questionnaire data with measures derived through Experience Sampling Method, ie, a digital diary method requesting participants to enter responses on their momentary context, feelings and thoughts 10 times a day during 6 consecutive days. Measures of all domains were translated to Dutch and are described in table 1.
Table 1.
Information for All Measures Included in the Analyses
| Domain | Measuresa |
|---|---|
| Childhood adversity | The questionnaire (child self-administered version of the Juvenile Victimization Questionnaire—2nd Revision56,57) covers 5 adversity modules: conventional crime, child maltreatment, peer and sibling victimization, sexual victimization, and witnessing and indirect victimization, with each item with answer options “Yes” or “No.” The conventional crime module was excluded as it was only administered in a limited number of participants due to time constraints. The remaining 4 modules were scored by summing up the relevant items. |
| Stress (ESM) | Based on the vulnerability-stress model, evidence has suggested that elevated emotional reactions to daily life minor stressors mediate the relationship between childhood adversity and PEs.12,19,24,58–60 For social stress,24,28,29 participants were firstly asked to indicate “Who is with me?.” If alone, they then rated the following 2 items “I find being alone pleasant” (reversed) and “I prefer to have company” (from 1 “Not at all” to 7 “Very much”). If they are in company, they rated “I feel comfortable in this company” (reversed) and “I prefer to be alone.” Average score across a 6-day period of either 2 items was used to indicate the social stress level. For activity stress,24,28,29 participants were firstly asked “what are you doing?.” Then they rated current activity with 3 items “I would rather do something else,” “This is difficult for me” and “I can do this well” (reversed). Average score across the 6-day period and 3 items was used to index the activity stress level. |
| Negative affect (ESM) | For emotional reactivity in daily life, negative affect was included quantified by the average score across a 6-day period on 6 ESM items: “I feel irritated,” “I feel anxious,” “I feel insecure,” “I feel sad,” “I feel stressed,” “I feel restless” (from 1 “Not at all” to 7 “Very much”). |
| Loneliness (ESM) | Feeling of loneliness is another pathway suggested to mediate the relationship between childhood adversity and PEs.21 Here, we quantified loneliness with the average score across a 6-day period with the ESM item “I feel lonely” (from 1 “Not at all” to 7 “Very much”). |
| General psychopathology | Nonpsychotic symptoms, especially anxiety and depression, have been demonstrated to mediate the link between childhood adversity and PEs, especially in general population.21,61 Here, we quantified general psychopathology using the 53-item Brief Symptom Inventory,48,62 which asked participants to rate on a 5-point Likert scale (from 0 “Not at all” to 4 “Extremely”) to indicate to which extent they experienced those difficulties in the past 7 days. It covers 9 symptom dimensions, of which paranoid ideation and psychoticism are closely related to psychotic symptoms, thus excluded from the current analyses. The remaining 7 dimensions, including somatization, obsession-compulsion, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, were used to indicate a person’s level of symptomatology by summing up the relevant items. |
| Maladaptive cognitive emotion regulation | Affective dysregulation is another relevant mediator in relation to childhood adversity and PEs. Here we used the 18-item short version of the Cognitive Emotion Regulation Questionnaire50,63 to quantify participants’ cognitive way of handling the emotional arousal situation. Participants were asked to rate on a 5-point Likert scale (from 1 “Almost never” to 5 “Almost always”) to indicate their thought following a negative experience. It covers 9 dimensions: positive refocusing, planning, positive reappraisal, putting into perspective, acceptance, self-blame, other-blame, rumination, and catastrophizing. The latter 4 dimensions are generally suggested as maladaptive and to be associated the most with psychopathological symptoms,43,49,50 thus were included in the current analyses. |
| Attachment insecurity | Based on attachment theory, the link between attachment insecurity and PEs has been well established14,17 and attachment style could mediate the association between childhood adversity and PEs.13,33 Here, we quantified attachment insecurity with the 36-item short version of the Inventory of Parent and Peer Attachment Revised,64,65 which asked participants to rate on a 4-point Likert scale (from 1 “Almost never” to 4 “Almost always”). The questionnaire covers attachment security to father, mother, and peers across 3 subdimensions (Communication, Trust, and Alienation). As the subdimension Alienation was only administered in a limited number of participants, we summed the scores of Communication and Trust reversely to indicate the degree of attachment insecurity to father, mother, and peer, separately. |
| Threat anticipation | Increasing evidence supports the role of threat anticipation in PEs and the association between childhood adversity and PEs.23,24,31,66,67 Here, we quantified threat anticipation with the 10-item short version of the Availability Test,38,68 which asked participants to indicate the possibility that each of 5 negative and 5 positive events described in the items would occur in the coming week on a 7-point Likert scale (from 1 “Very unlikely” to 7 “Very likely”). Negative items were included to indicate threat anticipation by summing up the scores. |
| Psychotic experiences | The Prodromal Questionnaire-1652,53 asked participants to indicate the presence of PEs through their lifetime as “True” or “False,” with True answers then rated the burden for that experience on a 4-point Likert scale (from 0 “Not burdensome” to 3 “Very burdensome”). We combined the endorsement and burdensome level to represent the continuum of PEs (0 = False, 1 = True and Not burdensome, 2 = True and Mild burdensome, 3 = True and Moderate burdensome, 4 = True and Very burdensome).53,69,70 Three subdimensions (perceptual abnormalities, unusual thought content, and negative symptoms) have been suggested as a good fit in a general population70 and were included in the current analyses, with each subdimension calculated by summing up the relevant items. |
Note: ESM, Experience Sampling Method; PEs, psychotic experiences.
aAll questionnaire items included an extra response option (ie, I do not wish to answer) due to the requirements from the participating schools. The proportion of each item with the extra response is reported in file “Supplementary_PQ_ProportionExtraResponse.csv” and data with the extra response were coded as missing data.
Statistical Analysis
Statistical analyses were performed using the R-statistical software, version 4.1.3.71 Missing values of the raw data (ie, at the item level) were handled using a random forest imputation algorithm, implemented using the R-package missForest, version 1.4.72 Descriptive statistics of each item in the raw and imputed data are reported in the file “Supplementary_PQ_Description.xlsx.”
Network estimation was performed on the imputed data. Firstly, scores of the 26 variables were computed using the relevant items and then transformed with nonparanormal transformation73 to relax the normality assumption. Thereafter, an undirected network with all 26 variables was constructed with GGM using the R-package bootnet, version 1.5.74 Within the network, each variable is represented by a node and an edge indicates a partial correlation between 2 variables, while a missing edge indicates an absent correlation, after conditioning on all other variables. To estimate a sparse (more interpretable) network and control for potential spurious connections, we applied an L1-penalty regularization selected by EBIC75–77 with the default regularization parameter lambda (0.5, which was shown to yield accurate network estimations). The network was visualized using the R-package qgraph, version 1.9.278 with the Fruchterman and Reingold layout. To assess the variability of edge-weight accuracy, we performed supplementary analyses of nonparametric bootstrapped 95% confidence intervals and difference tests (see Appendix S2) as suggested by Epskamp et al.79
Node centrality was estimated with strength centrality, quantifying how well a given node is directly connected to other nodes by summing the absolute values of the weights on the edges connected to that node.79 Supplementary analyses of correlation-stability coefficient (CS coefficient), difference tests, and expected influence were conducted to check the estimation (see Appendix S3). As, closeness and betweenness, 2 other centrality indices, have been suggested to be less stable and applicable,44,80 we chose not to interpret these in the current article (see Appendix S3).
Bridge strength indicates the importance of a given node in bridging communities/clusters81 and was estimated during the exploratory analyses, using R-package networktools, version 1.4.0.82 Items in each domain (eg, general psychopathology, attachment insecurity) were defined as a separate cluster, based on which we calculated bridge strength by summing the absolute value of every edge that connected a given node in a certain cluster to nodes in other clusters. Supplementary analyses of CS coefficient, difference tests, and bridge expected influence were conducted to assess the estimation of bridge strength (see Appendix S4). We also performed cluster detection using the “walktrap” algorithm in the R-package EGAnet, version 1.1.0,83 ie, exploring clusters of densely connected nodes within the network structure, while not considering any theoretically determined clusters (see Appendix S5).
Shortest paths 84 were computed using Dijkstra’s algorithm85 to indicate the minimum number of steps needed to go from each category of childhood adversity to the specific PEs. These could give a clear view of potential pathways and mediating variables between different categories of childhood adversity and PEs.35
Supplementary sensitivity analyses were also performed. First, to check the stability of the nonzero edges due to the approach to impute missing data, we used the stability selection technique86 to randomly select half of the cases of the sample size to perform the imputation with random forest and to estimate the network with GGM, over 100 iterations. Then the frequency of each edge present in the 100 iterations was calculated (Appendix S6). Second, we constructed another network quantifying PEs by the 5 items of the Diagnostic Interview Schedule for Children (DISC-C87; Appendix S7), which serves as a further validation of the estimation of the PQ-16 network by increasing the sample size (DISC-C were conducted in all 1913 adolescents). Third, since cross-sectional data do not allow for causal inference, we examined prospective associations with PEs at Wave 2 and the baseline variables used in the network analysis as the predictors using the least absolute shrinkage and selection operator (lasso) regression analysis88 (Appendices S7 and S8).
Results
Demographics
Table 2 displays the demographic information. Of 865 participants, n = 582 participants identified as female, n = 279 as male, and n = 4 as “Other.”
Table 2.
Descriptive Information for All Variables
| Variable | Mean | SD | Observed Range | Theoretical Range | Available Data |
|---|---|---|---|---|---|
| Age | 15.50 | 1.33 | 12–20 | 860 | |
| Stress | |||||
| Social stress | 2.80 | 0.89 | 1–5.62 | 1–7 | 780 |
| Activity stress | 3.09 | 0.78 | 1–7 | 1–7 | 778 |
| Negative affect | 2.28 | 0.94 | 1–7 | 1–7 | 783 |
| Loneliness | 1.89 | 0.91 | 1–7 | 1–7 | 781 |
| Childhood adversity | |||||
| Child maltreatment | 0.82 | 1.00 | 0–4 | 0–4 | 735 |
| Peer and sibling victimization | 1.63 | 1.00 | 0–6 | 0–6 | 730 |
| Sexual victimization | 0.89 | 1.32 | 0–7 | 0–7 | 703 |
| Witnessing and indirect victimization | 1.40 | 1.38 | 0–8 | 0–8 | 697 |
| Threat anticipation | 11.89 | 4.76 | 5–33 | 5–35 | 777 |
| General psychopathology | |||||
| Anxiety | 6.11 | 4.57 | 0–23 | 0–24 | 722 |
| Somatization | 6.00 | 5.03 | 0–26 | 0–28 | 724 |
| Obsession-compulsion | 7.41 | 4.92 | 0–24 | 0–24 | 717 |
| Hostility | 5.25 | 4.07 | 0–20 | 0–20 | 727 |
| Phobic anxiety | 3.49 | 3.64 | 0–20 | 0–20 | 725 |
| Depression | 6.21 | 5.64 | 0–24 | 0–24 | 709 |
| Interpersonal sensitivity | 5.39 | 3.96 | 0–16 | 0–16 | 726 |
| Attachment insecurity | |||||
| Father attachment insecurity | 19.77 | 3.78 | 9–28 | 8–32 | 617 |
| Mother attachment insecurity | 21.92 | 3.55 | 11–29 | 8–32 | 617 |
| Peer attachment insecurity | 22.12 | 4.12 | 8–31 | 8–32 | 623 |
| Maladaptive cognitive emotion regulation | |||||
| Rumination | 6.35 | 2.06 | 2–10 | 2–10 | 697 |
| Self-blame | 5.28 | 2.08 | 2–10 | 2–10 | 676 |
| Catastrophizing | 4.95 | 2.22 | 2–10 | 2–10 | 669 |
| Other-blame | 3.95 | 1.66 | 2–10 | 2–10 | 661 |
| Psychotic experiences | |||||
| Negative symptoms | 1.57 | 1.94 | 0–8 | 0–8 | 639 |
| Unusual thought content | 4.10 | 3.57 | 0–18 | 0–20 | 614 |
| Perceptual abnormalities | 4.50 | 4.79 | 0–28 | 0–36 | 597 |
The available data are reported due to missingness and those for psychotic experiences are highlighed in bold.
Network Estimation
The estimated network is displayed in figure 1a. Of 325 possible edges, 144 (44.31%) nonzero edges emerged, with a mean weight of 0.077. 140 (97.22%) edges were positive and 4 (2.78%) edges were negative. The scores of all the edges and of the plotted edges are reported in file “Supplementary_PQ_pcor.csv” and file “Supplementary_PQ_pcor_plot.csv,” respectively.
Fig. 1.
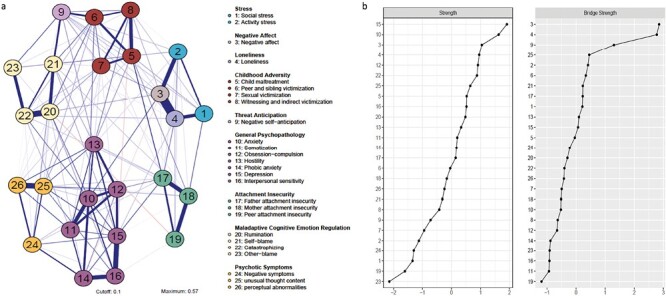
(a) Network model of childhood adversity, psychotic experiences, and potential psychological processes. Each node displays a variable, with variables in the same domain plotted by the same color. Each edge corresponds to a partial correlation between 2 nodes, the thicker the edge, the stronger the connection. Blue edges display positive connections and red edges display negative ones. (b) Centrality indices of the network: strength centrality (left) and bridge strength centrality (right). Variables are shown as standardized z-scores and sorted in decreasing order.
Node and Bridge Centrality
Strength centrality analysis (figure 1b; see raw scores in file “Supplementary_PQ_StrengthScore.csv”) revealed that depression (15), anxiety (10), negative affect (3), and loneliness (4) (in decreasing order) had the highest centrality. The CS coefficient (supplementary figure S3) was 0.75, indicating high stability. Indeed, the difference tests (supplementary figure S4) revealed that depression and anxiety were significantly different from all other nodes, except from each other, and negative affect and loneliness were significantly different from most of the other nodes in the network. Expected influence (supplementary figure S5) was strongly correlated with strength centrality (r = 0.997; P < .001), further confirming the results.
Bridge centrality analysis (figure 1b; see raw scores in file “Supplementary_PQ_BridgeStrengthScore.csv”) revealed nodes with highest bridge centrality were negative affect (3), loneliness (4), and threat anticipation (9). Visual inspection revealed that, for negative affect and loneliness, these were mainly driven by the connections negative affect (3)-loneliness (4), activity stress (2)-negative affect (3), and social stress (1)-loneliness (4), indicating strong interplay among stress, negative affect, and loneliness. Indeed, supplementary cluster detection without considering theory ascribed these 4 nodes into 1 cluster (supplementary figure S9). For threat anticipation, these were mainly driven by the connections between peer and sibling victimization (6)-threat anticipation (9), threat anticipation (9)-self-blame (21), and threat anticipation (9)-other blame (23). The CS coefficient (supplementary figure S6) was 0.75, indicating high stability. The difference tests (supplementary figure S7) revealed that negative affect and loneliness were significantly different from all the other nodes, except from each other, and threat anticipation was significantly different from almost all the other nodes. Bridge expected influence (supplementary figure S8) was strongly correlated with bridge strength centrality (r = 0.998, P < .001).
Shortest Paths in the Network
Four networks presenting the shortest paths between each category of childhood adversity and PEs are shown in figure 2. For childhood maltreatment (5) (figure 2a), the connections to PEs ran via other categories of childhood adversity, ie, connecting to negative symptoms (24) via peer and sibling victimization (6), anxiety (10), and phobic anxiety (14), to unusual thought content (25) via sexual victimization (7), and to perceptual abnormalities (26) via witnessing and indirect victimization (8) and hostility (13). Peer and sibling victimization (6) (figure 2b) either connected to unusual thought content (25) directly, or to negative symptoms (24) via anxiety (10) and phobic anxiety (14) and to perceptual abnormalities (26) via anxiety (10) and somatization (11). Sexual victimization (7) (figure 2c) directly connected to unusual thought content (25), through which it then connected to negative symptoms (24) and perceptual abnormalities (26). Witnessing and indirect victimization (8) (figure 2d) connected to perceptual abnormalities (26) via hostility (13), then connected to negative symptoms (24) and unusual thought content (25).
Fig. 2.
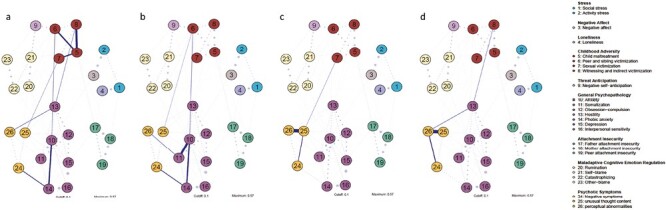
Networks displaying shortest paths between (a) child maltreatment (5), (b) peer and sibling victimization (6), (c) sexual victimization (7), and (d) witnessing and indirect victimization (8) and psychotic experiences. Dashed lines indicate connections existing within the network framework, but are less relevant when investigating shortest paths.
Supplementary sensitivity analysis (supplementary figure S10) showed that nonzero edges with strong weights in the constructed network were present in most of the 100 iterated estimations, indicating high stability.
Sensitivity Analyses Using Psychotic Symptoms Measured by DISC-C
The DISC-C network structure (supplementary figure S11) was well aligned with the PQ-16 network. The estimation of strength centrality (supplementary figure S14) revealed that depression (15) and anxiety (10) were still the first 2 nodes with the highest strength. While negative affect (3) and loneliness (4) were the third and fourth in the strength centrality order in the PQ-16 network, respectively, here they were the fifth and eighth. Thus, though the orders of node strength in the 2 networks were not exactly the same, these nodes were of higher order in both networks, especially anxiety and depression.
The estimation of bridge centrality (supplementary figure S17) revealed that negative affect (3), loneliness (4), and threat anticipation (9) were still the first 3 nodes with highest bridge centrality, confirming the results in the PQ-16 network with larger sample.
The shortest path networks (supplementary figure S20) revealed that the connection to PEs was via hostility (13) from childhood maltreatment (5), via threat anticipation (9) and hostility (13) from peer and sibling victimization (6), via depression (15) and hostility (13) from sexual victimization (7), and via childhood maltreatment (5) and hostility (13) from witnessing and indirect victimization (8). Given PEs were measured in different dimensions in the 2 networks, it is not possible to compare them to each other. However, notably, hostility (13) appeared on the shortest paths estimated within both networks.
Supplementary Longitudinal Analysis
For the lasso regression model including PEs measured by PQ-16, 161 participants (15–21 years; 119 females and 40 males) had complete data at Wave 2. Variables remained after regularization and the coefficients are reported in table 3. In general, the results showed that variables with higher strength centrality in the baseline network, including depression, negative affect, and loneliness, predicted follow-up PEs with larger effect sizes than other variables. The same was true for variables with higher bridge centrality, ie, negative affect, loneliness, and threat anticipation. For the model using PEs measured by DISC-C, 312 participants (13–21 years; 228 females and 80 males) with complete data at Wave 2 were available for analysis. The results (supplementary table S4) showed that loneliness (a variable with high strength and bridge centrality), threat anticipation (a variable with high bridge centrality), and hostility (lying on the shortest paths in the baseline network) remained after regularization.
Table 3.
Results of the Lasso Regression Analysis With PEs Measured by PQ-16.
| Measures at Wave 2 | Predicting Variables at Wave 1 | Coefficient β |
|---|---|---|
| Negative affect | Social stress | 0.113 |
| Negative affect | 0.240 | |
| Loneliness | −0.255 | |
| Peer and sibling victimization | 0.029 | |
| Threat anticipation | −0.067 | |
| Hostility | 0.005 | |
| Phobic anxiety | 0.092 | |
| Depression | 0.385 | |
| Mother attachment insecurity | −0.110 | |
| Catastrophizing | 0.002 | |
| Other-blame | −0.017 | |
| Perceptual abnormalities | −0.015 | |
| Unusual thought content | Activity stress | 0.038 |
| Negative affect | 0.177 | |
| Phobic anxiety | 0.001 | |
| Catastrophizing | 0.035 | |
| Unusual thought content | 0.125 | |
| Perceptual abnormalities | 0.010 | |
| Perceptual abnormalities | Loneliness | 0.109 |
| Child maltreatment | 0.220 | |
| Threat anticipation | 0.106 | |
| Somatization | 0.028 | |
| Hostility | 0.036 | |
| Interpersonal sensitivity | −0.102 | |
| Catastrophizing | 0.007 | |
| Other-blame | 0.026 | |
| Perceptual abnormalities | 0.276 |
Note: PEs, psychotic experiences; PQ-16, Prodromal Questionnaire-16. Predicting variables with higher coefficients are highlighted in bold.
Discussion
Findings
Using a network approach, the current study investigated the associations between childhood adversity and PEs by including multiple psychological mediators in a general population, adolescent sample. Our results revealed that depression, anxiety, negative affect, loneliness, and threat anticipation displayed highest centrality in the formation of the network. We also found evidence for a connective role of anxiety, hostility, and somatization in the shortest paths linking childhood adversity and PEs. These findings move beyond previous studies in 2 crucial aspects: (1) by recruiting multiple previously proposed mediators linking childhood adversity and PEs, we were able to detect those with a central role (ie, high centrality) in these complex associations; (2) by focusing on adolescence, we were able to better grasp the processes linking childhood adversity and emerging PEs in the earliest stages.
Depression, Anxiety, Negative Affect, and Loneliness as Central Elements of the Network
Depression and anxiety were detected as 2 nodes with the highest strength centrality, ie, they had the most and strongest connections with other nodes within the network. Previous studies have demonstrated that depression and anxiety often precede the onset and persistence of PEs.89,90 Negative affect and loneliness were the next 2 nodes with the highest strength centrality and the first 2 nodes with the highest bridge strength centrality. Our supplementary lasso regression analysis further found that variables with higher centrality in the network (ie, depression, negative affect and loneliness) and higher bridge centrality (ie, negative affect, loneliness, and threat anticipation) predicted follow-up PEs with higher effect sizes, further validating these findings. Together, they underscore the transdiagnostic, heterotypic nature of mental ill-health in young people, in agreement with current clinical recommendations.91–93
Bridging Role of Threat Anticipation Between Childhood Adversity and Maladaptive Cognitive Emotion Regulation
Threat anticipation and maladaptive cognitive emotion regulation are 2 psychological processes suggested to mediate the relationship between childhood adversity and PEs.21–23,36 A recent study67 with samples from the same SIGMA study demonstrated that threat anticipation was positively associated with childhood adversity and may mediate the association between childhood adversity, general psychopathology, and PEs in adolescents. Our study extends these findings by demonstrating that threat anticipation may be particularly associated with peer and sibling victimization, which was also the most common category of childhood adversity in our sample. Additionally, our results suggest a strong connection between threat anticipation and maladaptive cognitive emotion regulation strategies, especially self-blame, warranting further investigation.
General Psychopathology as the Main Connective Component in the Shortest Paths
By constructing the shortest path networks, our results supported and extended previous findings,35 indicating that multiple pathways may exist between childhood adversity and PEs, particularly via symptoms of general psychopathology. One of the symptoms playing a main connective role is anxiety (anxiety and phobic anxiety), which has been demonstrated to predict the onset of later PEs.89,94,95 Another main connective component identified is somatization, which lay on the pathway between peer and sibling victimization and perceptual abnormalities. These findings are consistent with those from Isvoranu et al in an adult clinical sample,35 despite notable differences in mean age and sex (75.7% of their sample was male, while 67.3% of our samples were girls), demonstrating a connective role of anxiety and somatic concern between childhood adversity and PEs. These findings point a possible stability of symptom-symptom correlations across the psychosis continuum, suggesting they may be inextricably linked in the context of childhood adversity, in agreement with reports linking childhood adversity to co-occurring psychotic, affective, and anxiety symptoms96 or even a general psychopathology (p-) factor.97 In addition, hostility was identified as another connective component in our study, which is further validated by our supplementary analysis. Pooled evidence has found that around 30% of patients with first-episode psychosis commit at least one act of violence, while one of the factors associated with violence of any severity is hostile affect.98 Furthermore, sensitivity to hostility (eg, angry faces) has been suggested in maltreated children.99 The role of hostility in linking childhood aversity and psychosis, however, has been rarely studied, warranting further research.
Limitations
Our study has some limitations. First, our analyses do not necessarily capture all aspects of the link between childhood adversity and PEs and the choice for certain mediators, but not others, may be arbitrary to a degree. For example, potential mediation by symptoms of post-traumatic stress disorder has been proposed21 but was not included in the current analysis. Nevertheless, our analyses include a wide array of potential mediators suggested in previous research and theoretical frameworks. Second, our samples were not representative in terms of sex, with the majority being girls. There is evidence that the characteristics and influence of childhood adversity on psychopathology is different for boys vs girls.100–102 Future research with sufficient data could estimate the difference of the networks between boys and girls. Third, our analyses were largely based on cross-sectional data, limiting possible causal inference, although the limited longitudinal analyses were generally supportive of our cross-sectional findings. Nevertheless, our results provide a compelling insight into the complex connections between childhood adversity, PEs, and multiple psychological mediators. Future studies with longitudinal design could further explore the causal relationship. Fourth, we used a self-report, retrospective measure of childhood adversity, which may be liable to memory bias and social desirability. Moreover, as the participants were in school while filling out the questionnaires, their data may have been influenced by others observing them, a possible source of bias known as the Hawthorne effect. Lastly, though the network approach is a promising tool helping the understanding of psychiatric disorders, methodological concerns and challenges,103,104 such as the generalizability problem due to the essentially data-driven analysis and the still limited insight into the relationship between the estimated network structure and the “true structure” of causal systems, still remain.
Conclusions
In summary, the present study uncovered the complex associations between childhood adversity and PEs by examining multiple psychological mediators during adolescence. Our results highlight the central role of depression, anxiety, negative affect, and loneliness within this complex system and the bridging role of threat anticipation between childhood adversity and maladaptive cognitive emotion regulation, especially between peer and sibling victimization and self-blame. The shortest path networks demonstrated multiple existing paths between childhood adversity and PEs, with symptoms of general psychopathology (ie, anxiety, hostility, and somatization) as main connective components. Together, these findings emphasize a broad, holistic approach to understanding the complex interactions and core variables/pathways underlying the link between childhood adversity and emerging PEs.
Supplementary Material
Acknowledgments
The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Contributor Information
Zhiling Qiao, Department of Neurosciences, Research Group Psychiatry, Center for Clinical Psychiatry, KU Leuven, Leuven, Belgium.
Ginette Lafit, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium; Department of Psychology, Group on Quantitative Psychology and Individual Differences, KU Leuven, Leuven, Belgium.
Aleksandra Lecei, Department of Neurosciences, Research Group Psychiatry, Center for Clinical Psychiatry, KU Leuven, Leuven, Belgium.
Robin Achterhof, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium.
Olivia J Kirtley, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium.
Anu P Hiekkaranta, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium.
Noëmi Hagemann, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium.
Karlijn S F M Hermans, Strategy and Academic Affairs, Administration and Central Services, Leiden University, Leiden, The Netherlands.
Bart Boets, Department of Neurosciences, Research Group Psychiatry, Center for Developmental Psychiatry, KU Leuven, Leuven, Belgium.
Ulrich Reininghaus, Department of Public Mental Health, Central Institute of Mental Health, Medical Faculty Mannheim, Heidelberg University, Mannheim, Baden-Württemberg, Germany; ESRC Centre for Society and Mental Health and Social Epidemiology Research Group, King’s College London, London, UK.
Inez Myin-Germeys, Department of Neurosciences, Research Group Psychiatry, Center for Contextual Psychiatry, KU Leuven, Leuven, Belgium.
Ruud van Winkel, Department of Neurosciences, Research Group Psychiatry, Center for Clinical Psychiatry, KU Leuven, Leuven, Belgium; University Psychiatric Center (UPC), KU Leuven, Leuven, Belgium.
Funding
This work was supported by a Research Foundation Flanders (FWO) Odysseus grant (G049219N) to I.M.-G., Z.Q., A.L., O.J.K., and U.R. are supported by the China Scholarship Council (202009110102), FWO PhD Fellowship (1104219N), FWO Senior Postdoctoral Fellowship (1257821N), and German Research Foundation Heisenberg professorship (389624707), separately. B.B. is supported by an FWO grant (G0C7816N) and an Excellence of Science grant (EOS G0E8718N/HUMVISCAT). R.W. is supported by an FWO Senior Clinical Fellowship (1803616N) and the Funds Julie Renson, Queen Fabiola and King Baudoin Foundation (Chair for Transition Psychiatry).
References
- 1. Van Os J, Reininghaus U.. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Staines L, Healy C, Murphy F, et al. . Incidence and persistence of psychotic experiences in the general population: systematic review and meta-analysis. Schizophr Bull. 2023;sbad056:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Linscott RJ, Van Os J.. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. [DOI] [PubMed] [Google Scholar]
- 4. Solmi M, Radua J, Olivola M, et al. . Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27(1):281–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bebbington P, Jonas S, Kuipers E, et al. . Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199(1):29–37. [DOI] [PubMed] [Google Scholar]
- 6. Abajobir AA, Kisely S, Scott JG, et al. . Childhood maltreatment and young adulthood hallucinations, delusional experiences, and psychosis: a longitudinal study. Schizophr Bull. 2017;43(5):1045–1055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Varese F, Smeets F, Drukker M, et al. . Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trotta A, Murray RM, Fisher HL.. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. Psychol Med. 2015;45(12):2481–2498. [DOI] [PubMed] [Google Scholar]
- 9. Bechdolf A, Thompson A, Nelson B, et al. . Experience of trauma and conversion to psychosis in an ultra-high-risk (prodromal) group. Acta Psychiatr Scand. 2010;121(5):377–384. [DOI] [PubMed] [Google Scholar]
- 10. Aas M, Andreassen OA, Aminoff SR, et al. . A history of childhood trauma is associated with slower improvement rates: findings from a one-year follow-up study of patients with a first-episode psychosis. BMC Psychiatry. 2016;16:126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE.. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31(2):189–195. [DOI] [PubMed] [Google Scholar]
- 12. Myin-Germeys I, van Os J.. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27(4):409–424. [DOI] [PubMed] [Google Scholar]
- 13. Pearce J, Simpson J, Varese F, Berry K, Bucci S, Moskowitz A.. Attachment and dissociation as mediators of the link between childhood trauma and psychotic experiences. Clin Psychol Psychother. 2017;24(6):1304–1312. [DOI] [PubMed] [Google Scholar]
- 14. Debbané M, Salaminios G, Luyten P, et al. . Attachment, neurobiology, and mentalizing along the psychosis continuum. Front Hum Neurosci. 2016;10:406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Howes OD, Bch BM, Murray RM.. Schizophrenia: an integrated sociodevelopmental-cognitive model. Eur PMC Funders Gr. 2014;383(9929):1677–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Berry K, Barrowclough C, Wearden A.. A review of the role of adult attachment style in psychosis: unexplored issues and questions for further research. Clin Psychol Rev. 2007;27(4):458–475. [DOI] [PubMed] [Google Scholar]
- 17. Ai G, Hef T, Schwannauer M, Macbeth AA.. A systematic review of attachment and psychosis: measurement, construct validity and outcomes. Acta Psychiatr Scand. 2014;129(4):257–274. [DOI] [PubMed] [Google Scholar]
- 18. Bentall RP, Rowse G, Shryane N, et al. . The cognitive and affective structure of paranoid delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry. 2009;66(3):236–247. [DOI] [PubMed] [Google Scholar]
- 19. Nuechterlein KH, Dawson ME.. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr Bull. 1984;10(2):300–312. [DOI] [PubMed] [Google Scholar]
- 20. Freeman D, Garety PA, Kuipers E, Fowler D, Bebbington PE.. A cognitive model of persecutory delusions. Br J Clin Psychol. 2002;41(4):331–347. [DOI] [PubMed] [Google Scholar]
- 21. Alameda L, Rodriguez V, Carr E, et al. . A systematic review on mediators between adversity and psychosis: potential targets for treatment. Psychol Med. 2020;50(12):1966–1976. [DOI] [PubMed] [Google Scholar]
- 22. Bloomfield MAP, Chang T, Woodl MJ, et al. . Psychological processes mediating the association between developmental trauma and specific psychotic symptoms in adults: a systematic review and meta-analysis. World Psychiatry. 2021;20(1):107–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Klippel A, Myin-Germeys I, Chavez-Baldini U, et al. . Modeling the interplay between psychological processes and adverse, stressful contexts and experiences in pathways to psychosis: an experience sampling study. Schizophr Bull. 2017;43(2):302–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Reininghaus U, Kempton MJ, Valmaggia L, et al. . Stress sensitivity, aberrant salience, and threat anticipation in early psychosis: an experience sampling study. Schizophr Bull. 2016;42(3):712–722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ludwig L, Werner D, Lincoln TM.. The relevance of cognitive emotion regulation to psychotic symptoms—a systematic review and meta-analysis. Clin Psychol Rev. 2019;72:101746. [DOI] [PubMed] [Google Scholar]
- 26. Korver-nieberg N, Berry K, Meijer CJ, de Haan L.. Adult attachment and psychotic phenomenology in clinical and non-clinical samples: a systematic review. Psychol Psychother Theory Res Pract. 2014;87(2):127–154. [DOI] [PubMed] [Google Scholar]
- 27. Russo DA, Stochl J, Hodgekins J, et al. . Attachment styles and clinical correlates in people at ultra high risk for psychosis. Br J Psychol. 2018;109(1):45–62. [DOI] [PubMed] [Google Scholar]
- 28. Myin-Germeys I, Van Os J, Schwartz JE, Stone AA, Delespaul PA.. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58(12):1137–1144. [DOI] [PubMed] [Google Scholar]
- 29. Palmier-Claus JE, Dunn G, Lewis SW.. Emotional and symptomatic reactivity to stress in individuals at ultra-high risk of developing psychosis. Psychol Med. 2012;42(5):1003–1012. [DOI] [PubMed] [Google Scholar]
- 30. Varghese D, Scott J, Welham J, et al. . Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr Bull. 2011;37(2):389–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Reininghaus U, Gayer-Anderson C, Valmaggia L, et al. . Psychological processes underlying the association between childhood trauma and psychosis in daily life: an experience sampling study. Psychol Med. 2016;46(13):2799–2813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Weissman DG, Bitran D, Miller AB, Schaefer JD, Sheridan MA, McLaughlin KA.. Difficulties with emotion regulation as a transdiagnostic mechanism linking child maltreatment with the emergence of psychopathology. Dev Psychopathol. 2019;31(3):899–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. van Dam DS, Korver-Nieberg N, Velthorst E, Meijer CJ, de Haan L; For Genetic Risk and Outcome in Psychosis (GROUP). Childhood maltreatment, adult attachment and psychotic symptomatology: a study in patients, siblings and controls. Soc Psychiatry Psychiatr Epidemiol. 2014;49(11):1759–1767. [DOI] [PubMed] [Google Scholar]
- 34. Mclaughlin KA, Green JG, Gruber MJ, Nancy A, Zaslavsky AM, Kessler RC.. Childhood adversities and first onset of psychiatric disorders in a national sample of adolescents. Arch Gen Psychiatry. 2012;69(11):1151–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Isvoranu AM, Van Borkulo CD, Boyette LL, Wigman JTW, Vinkers CH, Borsboom D; Group Investigators. A network approach to psychosis: pathways between childhood trauma and psychotic symptoms. Schizophr Bull. 2017;43(1):187–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lincoln TM, Marin N, Jaya ES.. Childhood trauma and psychotic experiences in a general population sample: a prospective study on the mediating role of emotion regulation. Eur Psychiatry. 2017;42:111–119. [DOI] [PubMed] [Google Scholar]
- 37. Liu J, Lim MSM, Ng BT, Chong SA, Subramaniam M, Mahendran R.. Global emotion dysregulation and maladaptive cognitive emotion regulation strategies mediate the effects of severe trauma on depressive and positive symptoms in early non-affective psychosis. Schizophr Res. 2020;222:251–257. [DOI] [PubMed] [Google Scholar]
- 38. Freeman D, Dunn G, Fowler D, et al. . Current paranoid thinking in patients with delusions: the presence of cognitive-affective biases. Schizophr Bull. 2013;39(6):1281–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Mikulincer M, Shaver PR.. Attachment orientations and emotion regulation. Curr Opin Psychol. 2019;25:6–10. [DOI] [PubMed] [Google Scholar]
- 40. Dagan O, Facompré CR, Bernard K.. Adult attachment representations and depressive symptoms: a meta-analysis. J Affect Disord. 2018;236:274–290. [DOI] [PubMed] [Google Scholar]
- 41. Bakermans-Kranenburg M, van IJzendoorn MH.. The first 10,000 Adult Attachment Interviews: distributions of adult attachment representations in clinical and non-clinical groups. Attach Hum Dev. 2009;11(3):223–263. [DOI] [PubMed] [Google Scholar]
- 42. Dan WG, Nitschke JB.. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat Rev Neurosci. 2013;14(7):488–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Huh HJ, Kim KH, Lee HK, Chae JH.. The relationship between childhood trauma and the severity of adulthood depression and anxiety symptoms in a clinical sample: the mediating role of cognitive emotion regulation strategies. J Affect Disord. 2017;213:44–50. [DOI] [PubMed] [Google Scholar]
- 44. McNally RJ. Can network analysis transform psychopathology? Behav Res Ther. 2016;86:95–104. [DOI] [PubMed] [Google Scholar]
- 45. Fried EI, Bockting C, Arjadi R, et al. . From loss to loneliness: the relationship between bereavement and depressive symptoms. J Abnorm Psychol. 2015;124(2):256–265. [DOI] [PubMed] [Google Scholar]
- 46. Boschloo L, Van Borkulo CD, Borsboom D, Schoevers RA.. A prospective study on how symptoms in a network predict the onset of depression. Psychother Psychosom. 2016;85(3):183–184. [DOI] [PubMed] [Google Scholar]
- 47. Steenkamp L, Weijers J, Gerrmann J, Eurelings-Bontekoe E, Selten J-P.. The relationship between childhood abuse and severity of psychosis is mediated by loneliness: an experience sampling study. Schizophr Res. 2022;241:306–311. [DOI] [PubMed] [Google Scholar]
- 48. Derogatis LR, Melisaratos N.. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- 49. Aldao A, Nolen-Hoeksema S, Schweizer S.. Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin Psychol Rev. 2010;30(2):217–237. [DOI] [PubMed] [Google Scholar]
- 50. Garnefski N, Kraaij V, Spinhoven P.. Negative life events, cognitive emotion regulation and emotional problems. Pers Individ Dif. 2001;30(8):1311–1327. [Google Scholar]
- 51. Kirtley OJ, Achterhof R, Hagemann N, et al. . Initial cohort characteristics and protocol for SIGMA: an accelerated longitudinal study of environmental factors, inter- and intrapersonal processes, and mental health in adolescence. PsyArXiv, 2 Apr. 2021.
- 52. Loewy RL, Bearden CE, Johnson JK, Raine A, Cannon TD.. The prodromal questionnaire (PQ): preliminary validation of a self-report screening measure for prodromal and psychotic syndromes. Schizophr Res. 2005;79(1):117–125. [PubMed] [Google Scholar]
- 53. Ising HK, Veling W, Loewy RL, et al. . The validity of the 16-item version of the prodromal questionnaire (PQ-16) to screen for ultra high risk of developing psychosis in the general help-seeking population. Schizophr Bull. 2012;38(6):1288–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Jong YD, Mulder CL, Boon A, Coenders E, van der Gaag M.. Cross validation of the prodromal questionnaire 16-item version in an adolescent help-seeking population. Schizophr Bull Open. 2020;1(1):sgaa033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chen F, Wang L, Heeramun-Aubeeluck A, et al. . Identification and characterization of college students with attenuated psychosis syndrome in China. Psychiatry Res. 2014;216(3):346–350. [DOI] [PubMed] [Google Scholar]
- 56. Finkelhor D, Hamby SL, Ormrod R, Turner H.. The juvenile victimization questionnaire: reliability, validity, and national norms. Child Abuse Negl. 2005;29(4):383–412. [DOI] [PubMed] [Google Scholar]
- 57. Hamby S, Finkelhor D, Turner H, Kracke K.. The Juvenile Victimization Questionnaire Toolkit . 2011. http://www.unh.edu/ccrc/jvq/index_new.html
- 58. Lardinois M, Lataster T, Mengelers R, Van Os J, Myin-Germeys I.. Childhood trauma and increased stress sensitivity in psychosis. Acta Psychiatr Scand. 2011;123(1):28–35. [DOI] [PubMed] [Google Scholar]
- 59. Rauschenberg C, van Os J, Cremers D, Goedhart M, Schieveld JNM, Reininghaus U.. Stress sensitivity as a putative mechanism linking childhood trauma and psychopathology in youth’s daily life. Acta Psychiatr Scand. 2017;136(4):373–388. [DOI] [PubMed] [Google Scholar]
- 60. Rössler W, Ajdacic-Gross V, Rodgers S, Haker H, Müller M.. Childhood trauma as a risk factor for the onset of subclinical psychotic experiences: exploring the mediating effect of stress sensitivity in a cross-sectional epidemiological community study. Schizophr Res. 2016;172(1–3):46–53. [DOI] [PubMed] [Google Scholar]
- 61. Bebbington P. Unravelling psychosis: psychosocial epidemiology, mechanism, and meaning. Shanghai Arch Psychiatry. 2015;27(2):70–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Derogatis LR. The Brief Symptom Inventory (BSI) Administration, Scoring, and Procedures Manual. 4th ed. Minneapolis, MN: National Computer Systems; 1993. [Google Scholar]
- 63. Garnefski N, Kraaij V.. Cognitive emotion regulation questionnaire—development of a short 18-item version (CERQ-short). Pers Individ Dif. 2006;41(6):1045–1053. [Google Scholar]
- 64. Gullone E, Robinson K.. The Inventory of Parent and Peer Attachment—Revised (IPPA-R) for children: a psychometric investigation. Clin Psychol Psychother. 2005;12(1):67–79. [Google Scholar]
- 65. Armsden GC, Greenberg MT.. The inventory of parent and peer attachment: individual differences and their relationship to psychological well-being in adolescence. J Youth Adolesc. 1987;16:427–454. [DOI] [PubMed] [Google Scholar]
- 66. Kvarta MD, Chiappelli J, West J, et al. . Aberrant anterior cingulate processing of anticipated threat as a mechanism for psychosis. Psychiatry Res Neuroimaging. 2021;313:111300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Paetzold I, Gugel J, Schick A, et al. . The role of threat anticipation in the development of psychopathology in adolescence: findings from the SIGMA Study [published online ahead of print]. Eur Child Adolesc Psychiatry. 2022. doi: 10.1007/s00787-022-02048-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Kaney S, Bowen-Jones K, Dewey ME, Bentall RP.. Two predictions about paranoid ideation: deluded, depressed and normal participants’ subjective frequency and consensus judgments for positive, neutral and negative events. Br J Clin Psychol. 1997;36(3):349–364. [DOI] [PubMed] [Google Scholar]
- 69. Nelson B, Fusar-Poli P, Yung AR.. Can we detect psychotic-like experiences in the general population? Curr Pharm Des. 2012;18(4):376–385. [DOI] [PubMed] [Google Scholar]
- 70. Howie C, Hanna D, Shannon C, Davidson G, Mulholland C.. The structure of the Prodromal Questionnaire-16 (PQ-16): exploratory and confirmatory factor analyses in a general non-help-seeking population sample. Early Interv Psychiatry. 2022;16(3):239–246. [DOI] [PubMed] [Google Scholar]
- 71. R Core Team. R: A Language and Environment for Statistical Computing. Version 4.1.3. 2022. https://www.r-project.org/
- 72. Stekhoven DJ. missForest: Nonparametric Missing Value Imputation using Random Forest. R Package Version 1.4 . 2013. https://CRAN.R-project.org/package=missForest
- 73. Liu H, Lafferty J, Wasserman L.. The nonparanormal: semiparametric estimation of high dimensional undirected graphs. J Mach Learn Res. 2009;10:2295–2328. [PMC free article] [PubMed] [Google Scholar]
- 74. Epskamp S, Fried EI.. Package “bootnet”: Bootstrap Methods for Various Network Estimation Routines. R Package Version 1.5 . 2022. https://CRAN.R-project.org/package=bootnet
- 75. Van Borkulo CD, Borsboom D, Epskamp S, et al. . A new method for constructing networks from binary data. Sci Rep. 2014;4:5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Opsahl T, Agneessens F, Skvoretz J.. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Netw. 2010;32(3):245–251. [Google Scholar]
- 77. Boccaletti S, Latora V, Moreno Y, Chavez M, Hwang DU.. Complex networks: structure and dynamics. Phys Rep. 2006;424(4–5):175–308. [Google Scholar]
- 78. Epskamp S, Cramer AO, Waldorp LJ, Schmittmann VD, Borsboom D.. Network visualizations of relationships in psychometric data. J Stat Softw. 2012;48(4):1–18. [Google Scholar]
- 79. Epskamp S, Borsboom D, Fried EI.. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50(1):195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Bringmann LF, Elmer T, Epskamp S, et al. . What do centrality measures measure in psychological networks? J Abnorm Psychol. 2019;128(8):892–903. [DOI] [PubMed] [Google Scholar]
- 81. Jones PJ, Ma R, McNally RJ.. Bridge centrality: a network approach to understanding comorbidity. Multivariate Behav Res. 2021;56(2):353–367. [DOI] [PubMed] [Google Scholar]
- 82. Jones P. networktools: Tools for Identifying Important Nodes in Networks. R Package Version 1.4.0. 2021. https://cran.r-project.org/package=networktools
- 83. Golino H, Christensen AP.. EGAnet: Exploratory Graph Analysis—A Framework for Estimating the Number of Dimensions in Multivariate Data using Network Psychometrics. R Package Version 1.0.1 . 2022. https://CRAN.R-project.org/package=EGAnet
- 84. Brandes U. On variants of shortest-path betweenness centrality and their generic computation. Soc Netw. 2008;30(2):136–145. [Google Scholar]
- 85. Dijkstra EW. A note on two problems in connexion with graphs. Numer Math. 1959;1:269–271. [Google Scholar]
- 86. Meinshausen N. Stability selection. J R Stat Soc B. 2010;72(4):417–473. [Google Scholar]
- 87. Costello EJ, Edelbrock CS, Costello AJ.. Validity of the NIMH Diagnostic Interview Schedule for Children: a comparison between psychiatric and pediatric referrals. J Abnorm Child Psychol. 1985;13(4):579–595. [DOI] [PubMed] [Google Scholar]
- 88. Society RS. Regression shrinkage and selection via the lasso. J R Stat Soc B. 1996;58(1):267–288. [Google Scholar]
- 89. Freeman D, Stahl D, McManus S, et al. . Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. 2012;47(8):1195–1203. [DOI] [PubMed] [Google Scholar]
- 90. Krabbendam L, Myin-Germeys I, Hanssen M, et al. . Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. Br J Clin Psychol. 2005;44(Pt 1):113–125. [DOI] [PubMed] [Google Scholar]
- 91. Shah JL. Bringing clinical staging to youth mental health from concept to operationalization (and back again). JAMA Psychiatry. 2019;76(11):1121–1123. [DOI] [PubMed] [Google Scholar]
- 92. Shah JL, Scott J, Mcgorry PD, et al. . Transdiagnostic clinical staging in youth mental health: a first international consensus statement. World Psychiatry. 2020;19:233–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Danese A. Bridging between youth psychiatry and child and adolescent psychiatry. World Psychiatry. 2022;21(1):83–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Ben-Zeev D, Ellington K, Swendsen J, Granholm E.. Examining a cognitive model of persecutory ideation in the daily life of people with schizophrenia: a computerized experience sampling study. Schizophr Bull. 2011;37(6):1248–1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Thewissen V, Bentall RP, Oorschot M, et al. . Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50(2):178–195. [DOI] [PubMed] [Google Scholar]
- 96. Van Nierop M, Viechtbauer W, Gunther N, et al. ; Genetic Risk and OUtcome of Psychosis investigators. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychol Med. 2015;45(6):1277–1288. [DOI] [PubMed] [Google Scholar]
- 97. Caspi A, Houts RM, Belsky DW, et al. . The p factor: one general psychopathology factor in the structure of psychiatric disorders? Clin Psychol Sci. 2014;2(2):119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Large MM, Nielssen O.. Violence in first-episode psychosis: a systematic review and meta-analysis. Schizophr Res. 2011;125(2–3):209–220. [DOI] [PubMed] [Google Scholar]
- 99. da Silva Ferreira GC, Crippa JAS, de Lima Osório F.. Facial emotion processing and recognition among maltreated children: a systematic literature review. Front Psychol. 2014;5:1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Tolin DF, Foa EB.. Sex differences in trauma and posttraumatic stress disorder: a quantitative review of 25 years of research. Psychol Bull. 2006;132(6):959–992. [DOI] [PubMed] [Google Scholar]
- 101. Fisher H, Morgan C, Dazzan P, et al. . Gender differences in the association between childhood abuse and psychosis. Br J Psychiatry. 2009;194(4):319–325. [DOI] [PubMed] [Google Scholar]
- 102. Pereda N, Guilera G, Forns M, Gómez-Benito J.. The prevalence of child sexual abuse in community and student samples: a meta-analysis. Clin Psychol Rev. 2009;29(4):328–338. [DOI] [PubMed] [Google Scholar]
- 103. Fried EI, Cramer AOJ.. Moving forward: challenges and directions for psychopathological network theory and methodology. Perspect Psychol Sci. 2017;12(6):999–1020. [DOI] [PubMed] [Google Scholar]
- 104. Guloksuz S, Pries LK, Van Os J.. Application of network methods for understanding mental disorders: pitfalls and promise. Psychol Med. 2017;47(16):2743–2752. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


