Abstract
Introduction and importance
Odontoid fracture (OF) is among the most common and challenging cervical spine fractures in regards to the treatment and surgical approach. Atlanto-axial dislocation (AAD) is considered a significant complication after failed non-surgical treatment of OF. Traditionally, it requires anterior odontoidectomy followed by posterior C1-C2 reduction and fusion. In latest studies, Atlanto-axial joint (AAJ) remodeling in a posterior-only approach has got attention.
Case presentation
We herein present a 30-year-old man with missed type-II OF, presenting with irreducible anterior AAD and progressive neurological deficit. Old non-united OF with dorsal callous formation, compressing spinal cord, was detected. The patient underwent correction of the deformity and reduction of the fracture utilizing the posterior-only approach. AAJ remodeling, callous release and C1-C2 fusion was performed in standard prone position, under fluoroscopic guide and intraoperative electrophysiological monitoring. The patient had uneventful surgery and postoperative course and was neurologically intact with appropriate alignment in 6-month follow-up.
Clinical discussion
The irreducible AAD following type-II OF could be successfully treated with posterior-only approach (C1-C2 fusion).
Conclusion
Type-II OF is considered unstable requiring surgical management. Close follow-up and appropriate patient education is mandatory in non-surgical treatment. Irreducible AAD has been managed with anterior odontoid resection and posterior fusion. Several complications of anterior surgery, makes posterior-only approach a noticeable choice.
Keywords: Odontoid fracture, Atlanto-axial dislocation (AAD), Posterior-only approach, Atlanto-axial joint (AAJ)
Highlights
-
•
Type-II odontoid fracture is considered unstable requiring surgical management.
-
•
Close follow-up and appropriate patient education is mandatory in non-surgical treatment.
-
•
The Atlanto-axial dislocation (AAD) following type-II OF could be successfully treated with posterior-only approach.
-
•
Posterior-only approach is feasible method for correction of AAD in type-II OF associated with less complications.
1. Introduction
Odontoid fracture (OF) accounts for approximately one third of cervical spine fractures [1,2]. In the elderly, it is the most common spinal fracture, even due to low-energy trauma [3,4]. Type-II OF in D'Alonso's classification is the most common type [5] and is classified to different subgroups based on comminution of fragments [6]. OFs rarely causes neurological deficit, due to anatomic location and wider spinal canal at C1-C2 level [7]. External immobilization is widely acceptable for management of type-I and III OFs; but, type-II has many challenges and considerations in treatment [1,5]. Success in non-operative management, depends in many circumstances including age, medical comorbidities and fracture type. In type-II fractures, there is a 30–60 % chance of effective fusion with non-operative management depending on patients' condition and fracture characteristics [1]. Non-union and mal-union of the odontoid are the most common hazards, threatening non-operative managed cases of OFs. Atlanto-axial dislocation (AAD) is also a major complication [[7], [8], [9]] of the missed cases of failed non-surgical treatment of OFs. Commonly, failure in non-operative management, indicates surgical intervention [1,10]. Anterior, posterior or combined approaches for non-united OF has been utilized based on clinical and anatomic characteristics [7]. We herein report a delayed presentation of irreducible traumatic AAD in a missed case of non-united, type-II OF; and its successful management utilizing posterior-only approach.
2. Case presentation
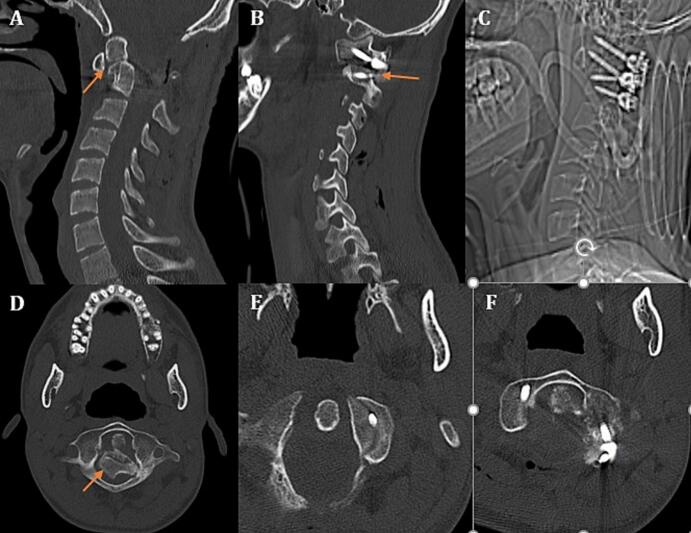
A 30-year-old man was referred to out center with quadriparesis and signs of myelopathy. He was in a car accident 6 months before the presentation, and has been admitted in a hospital due to head, face and neck trauma. He has been diagnosed with stable, type-II OF (Fig. 1A) and was discharged with a Philadelphia collar and instructions for close follow-up. He has undergone facial and mandibular internal fixation 2 weeks after the trauma. He was operated by maxillofacial surgeons during the same admission. In his post-operative course, he developed quadriparesia and distal paresthesia for what he had undergone vascular investigations with conventional and CT-angiogram (Fig. 1B) of carotid and vertebral arteries (Fig. 1C). Displaced OF and dislocated AAJ was missed in imaging investigations (Fig. 1B). The patient was discharged and did not refer for months afterward, till he presented to a neurosurgeon with progressing neurologic deficit. Initial evaluations revealed missed type-II OF with anterior AAD and bilateral locked C1-C2 facet joints (Fig. 1D).
Fig. 1.
A: Initial cervical sagittal CT-scan demonstrating a non-displaced type-II odontoid fracture (OF, arrow); B: displaced OF missed in sagittal brain CT-angiogram; C: normal brain CT-angiogram of the patient being performed after the maxillofacial surgery; D: delayed cervical sagittal CT-scan demonstrating displaced type-II OF with AAD showing posterior fibro-osseous bundle (arrow); E: cervical sagittal CT-scan demonstrating the C1-C2 locked facet (arrow); F: lateral cervical radiography demonstrating proximal, posteriorly displaced segment compressing upper cervical spinal cord segment and lower medulla.
In our spine surgery center, we further evaluated the patient with computed tomography (CT), magnetic resonance imaging (MRI), CT-angiography and dynamic cervical radiogram. Type-II OF with anterior displacement of distal segment associated with AAD and bilateral locked C1-C2 facet was identified (Fig. 1D, E). Posterior fibro-osseous bundle (bone callous) was connecting fracture segments (Fig. 1D). Proximal, posteriorly displaced segment, beside posterior fibro-osseous connecting bundle, was compressing upper cervical spinal cord segment and lower medulla (Fig. 1F).
Due to neurological deficit and anterior spinal cord compression, cervical traction was contraindicated, but we have applied the cervical traction under general anesthesia with neurophysiologic monitoring. Thus, we planned a posterior-only approach for correction of the deformity. Surgery was performed with intraoperative neuromonitoring comprising motor evoked potentials (MEP), sensory evoked potentials (SEP), and electromyography (EMG). After posterior dissection of craniovertebral junction in standard prone position and head fixation, laminectomy of C1-C2, along with small suboccipital craniectomy was performed. Then, C2-ganglion was dissected bilaterally in order to expose C1-C2 facet joint completely. After bilateral wedge drilling of C1 and C2 articular processes, reduction was not achieved. Therefore, under fluoroscopic guidance, facet joints were distracted utilizing an osteotome. This maneuver provided appropriate space for partial resection of posterior fibro-osseous bundle. It was done under close fluoroscopic guide. This procedure, beside intraoperative cervical traction, lead to acceptable C1-C2 and odontoid reduction (Fig. 2A) and released of the C1C2 facet joint (Fig. 2B). Posterior C1-C2 fusion was then performed with bilateral C1 lateral mass screws, C2 pedicular and laminar screws (Fig. 2C). The spinal canal was compromised secondary to AAD and formation of the posterior fibro-osseous bundle (Fig. 2D). The spinal canal was indirectly decompressed after proper reduction (Fig. 2E, F). Surgery was performed with intraoperative neuromonitoring comprising motor evoked potentials (MEP), sensory evoked potentials (SEP), and electromyography (EMG). No change in the electrophysiological parameters was recorded during and after the surgery.
Fig. 2.
A: Postoperative mid-sagittal cervical CT-scan demonstrating reduction of the odontoid fracture (arrow), resection of the callous resection, and decompression of the spinal cord; B: postoperative sagittal cervical CT-scan demonstrating release of the C1-C2 facet (arrow), release of intervertebral foramen and fusion of the C1-C2; C: postoperative lateral cervical radiography demonstrating reduction of the fracture and decompression of the spinal canal and C1-C2 fusion with bilateral C1 lateral mass screws, unilateral C2 pedicular screw and unilateral C2 laminar screw; D: preoperative axial cervical CT-scan demonstrating compromise of the cervical canal with cord compression due to displacement of the C1-C2 and formation of the posterior fibro-osseous bundle (arrow); E, F: postoperative axial cervical CT-scan demonstrating proper reduction of the Atlanto-axial dislocation and complete release of the spinal canal and cord decompression with C1-C2 fusion.
The patient was discharged from the hospital at 3rd postoperative day. The postoperative course was uneventful. After 6 months, complete neurological recovery and acceptable C1-C2 facet joint fusion, was reached. The work has been reported in line with the Updating consensus Surgical CAse REport (SCARE) guidelines [11]. Written informed consent was obtained from the patient's parents/legal guardian for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
3. Discussion
OFs have 3 main types according to D'Alonso's classification. Type-I includes all fractures of tip of the dense process. In type-II, fracture involves base of the odontoid process [5]. It also has a subclassification based on distal segment comminution [6]. Type-III is extension of fracture line into C2-vertebral body [5,6]. Impacts causing extension is always responsible for OFs. While sagittal forces cause type-III fractures, type-II occurs mostly when lateral force is present with angle near 45° from midline [12]. Osteoporosis is a major predisposing factor in elderly patients who had minor trauma, whereas in younger patients, high energy trauma is the cause [13].
The most common symptom in pure OFs is headache, mainly in occipital area. Neurological deficits are uncommon due to wider spinal canal cross sectional area at this level. Dysphagia may also be present. In elderly patients, asymptomatic fractures are common due to neurological age-related comorbidities [14,15]. Type I and type III OF are considered stable and managed with external immobilization with excellent fusion rate [2,3,5]. Type-II, has many variations and considerations. Non-operative management includes Halo-vest (HV) and collar. Although HV showed superior success rate in some studies, its higher morbidity and lower tolerance by the patients makes collar the standard non-operative management [1,12]. Fracture dislocation >5 mm, angulation >10° and failed external immobilization are considered as relative indications for surgical management [1]. In a 2017 review of OFs, considering osteoporotic basis of OFs and higher failure rate in type-II, surgical management got more attention, especially in elderly patients (>65 years) [13]. Rizvi et al. suggested that surgical intervention is of great benefit in patients ≥50 years old with type-II OF [14]. In 2022, additional factors noted for consideration of surgical management in type-II OF. Some of them are: age of 45–55 years or older, posterior displacement and displacement >6 mm, Transverse Atlas Ligament injury, delayed diagnosis or treatment (>4 days), osteoporosis, smoking, fracture comminution, angulation >10° and the inability to achieve adequate reduction (>1 mm fracture gap) or loss of reduction (>2 mm posterior re-displacement). Also HV is mentioned superior to collar for non-operative management of type-II fractures [15]. In the aspect of craniovertebral junction stability, C1-C2 is a highly mobile joint and any major fracture in this region (specially OFs) should be considered unstable until otherwise proven [[16], [17], [18]].
Traumatic AAD has been such a challenging case, for which many studies aimed to reach a standard management in recent decade. It appears that mobility in fracture site is starting point of a cascade leading to AAD [19]. Presenting symptoms are usually altered neck range of motion, neck pain and delayed onset-progressive neurological deficit [20]. Radiologic evaluations must include CT-scan, MRI, dynamic X-ray and vertebral artery (VA) angiogram [19,20]. In these imaging evaluations, callous formation, Atlanto-axial joint (AAJ) relation, reducibility, cord compression and vertebral artery injury should be sought [21]. Irreducible AAD (IAAD) has been traditionally managed with trans-oral/facial decompression and posterior fusion; but, anterior decompression has brought about severe morbidities [7]. Therefore, recent attempts aimed eliminating anterior surgery and managing IAAD with posterior only approaches. This was successfully tried by Goel in 2005 manipulating C1-C2 joints [19]. In posterior approach, AAJ is realigned with drilling with or without joint expander. In selected cases and appropriate occasions, this procedure has been successful in reduction, fusion and morbidity control through elimination of anterior surgery [7,[19], [20], [21], [22]]. Some points help selecting proper cases for this approach:
-
•
Callous formation and progressive/new neurological symptoms, indicate chronic motion at fracture site, thus “feasibility” of posterior reduction [7].
-
•
As this approach needs bilateral AAJ remodeling, any reason blocks access to one joint -such as VA injury or its relation to the joint- makes reduction less feasible [7].
-
•
Pre-operative traction usually failed and caused morbidity in these cases [7].
In our case, reducibility was investigated by cervical dynamic radiogram, showing no reduction. Thus, concerning little chance of reduction in such cases with cervical traction and anterior spinal cord compression by callous bulk, we decided not to try traction prior to surgery. Gardner traction without weight application was fixed after general anesthesia. In effort for reduction, bilateral joint manipulation and osteotomy was done just as it was described by Salunke et al. [7]. Gradual weight application on traction beside joint remodeling could not reduce dislocated joints. Thus, under fluoroscopic guide, we released callous at fracture site. Then reduction was achieved and fusion was performed.
4. Conclusion
Type-II OF is considered unstable due to many reasons and needs early surgical management in most cases. External immobilization with collar is a treatment choice in selected cases, but close follow-up beside excellent patient education and compliance is mandatory. This fracture has great chance of non-union. Irreducible AAD is a consequence of non-union and has been managed with anterior odontoid resection and posterior fusion in past decades. In last years, due to several morbidities of anterior surgery, posterior-only approach has got attentions and many progresses have been achieved.
Consent for publication
The patient and his legal guardians provided their informed written consent for publication of the case.
Availability of data and materials
The medical record, laboratory examinations and all the imaging are available on request in DICOM files.
Ethics approval and consent to participate
Not applicable.
Funding
No funding was received.
Authors' contribution
Conception and Design: SR. Mousavi, MR. Farrokhi
Acquisition of the data: MH. Shahpari, K. Eghbal, A. H. Jangiaghdam
Data Analysis and/or interpretation: H. Jangiaghdam, F. Ghaffarpasand, K. Eghbal
Drafting of manuscript and/or critical revising: All the authors
Approval of final version of manuscript: All the authors
Guarantor
Dr. Seyed Reza Mousavi
Declaration of competing interest
None of the authors have any conflict of interest to declare regarding the manuscript.
Acknowledgements
We would like to acknowledge the editorial assistance of Diba Negar Research Institute for improving the style and English of the manuscript.
Contributor Information
Majid Reza Farrokhi, Email: farokhim@sums.ac.ir.
Hamid Jangiaghdam, Email: jangia@sums.ac.ir.
Fariborz Ghaffarpasand, Email: fariborz.ghaffarpasand@gmail.com.
References
- 1.Carvalho A.D., Figueiredo J., Schroeder G.D., Vaccaro A.R., Rodrigues-Pinto R. Odontoid fractures. Clin. Spine Surg. 2019;32(8):313–323. doi: 10.1097/BSD.0000000000000872. [DOI] [PubMed] [Google Scholar]
- 2.Grasso G., Leone L., Torregrossa F. Management of odontoid cervical fracture. World Neurosurg. 2019;123:246–247. doi: 10.1016/j.wneu.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 3.Waqar M., Van-Popta D., Barone D.G., Sarsam Z. External immobilization of odontoid fractures: a systematic review to compare the halo and hard collar. World Neurosurg. 2017;97:513–517. doi: 10.1016/j.wneu.2016.10.035. [DOI] [PubMed] [Google Scholar]
- 4.Tenny S., Munakomi S., Varacallo M. StatPearls Publishing; Treasure Island (FL): 2023. Odontoid Fractures. StatPearls. Copyright © 2023, StatPearls Publishing LLC. [PubMed] [Google Scholar]
- 5.Anderson L.D., D’Alonzo R.T. Fractures of the odontoid process of the axis. J. Bone Joint Surg. Am. 1974;56(8):1663–1674. [PubMed] [Google Scholar]
- 6.Hadley M.N., Browner C.M., Liu S.S., Sonntag V.K. New subtype of acute odontoid fractures (type IIA) Neurosurgery. 1988;22(1 Pt 1):67–71. doi: 10.1227/00006123-198801010-00010. [DOI] [PubMed] [Google Scholar]
- 7.Salunke P., Sahoo S.K., Savardekar A., Ghuman M., Khandelwal N.K. Factors influencing feasibility of direct posterior reduction in irreducible traumatic atlantoaxial dislocation secondary to isolated odontoid fracture. Br. J. Neurosurg. 2015;29(4):513–519. doi: 10.3109/02688697.2015.1019421. [DOI] [PubMed] [Google Scholar]
- 8.Eghbal K., Abdollahpour H.R., Ghaffarpasand F. Traumatic chance fracture of cervical spine: a rare fracture type and surgical management. Asian J. Neurosurg. 2018;13(3):906–909. doi: 10.4103/ajns.AJNS_80_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eghbal K., Rakhsha A., Saffarrian A., Rahmanian A., Abdollahpour H.R., Ghaffarpasand F. Surgical management of adult traumatic Atlantoaxial rotatory subluxation with unilateral locked facet; case report and literature review. Bull. Emerg. Trauma. 2018;6(4):367–371. doi: 10.29252/beat-060416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsu W.K., Anderson P.A. Odontoid fractures: update on management. J. Am. Acad. Orthop. Surg. 2010;18(7):383–394. doi: 10.5435/00124635-201007000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A. The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 12.Ivancic P.C. Odontoid fracture biomechanics. Spine. 2014;39(24) doi: 10.1097/BRS.0000000000000609. (E1403-E10) [DOI] [PubMed] [Google Scholar]
- 13.Robinson A.L., Möller A., Robinson Y., Olerud C. C2 fracture subtypes, incidence, and treatment allocation change with age: a retrospective cohort study of 233 consecutive cases. Biomed. Res. Int. 2017;2017:8321680. doi: 10.1155/2017/8321680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rizvi S.A.M., Helseth E., Harr M.E., Mirzamohammadi J., Rønning P., Mejlænder-Evjensvold M., et al. Management and long-term outcome of type II acute odontoid fractures: a population-based consecutive series of 282 patients. Spine J. 2021;21(4):627–637. doi: 10.1016/j.spinee.2020.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Nourbakhsh A., Hanson Z.C. Odontoid fractures: a standard review of current concepts and treatment recommendations. J. Am. Acad. Orthop. Surg. 2022;30(6):e561–e572. doi: 10.5435/JAAOS-D-21-00165. [DOI] [PubMed] [Google Scholar]
- 16.Farrokhi M.R., Mousavi S.R., Rafieossadat R. Idiopathic spinal cord herniation at the cervicothoracic junction level presenting with unilateral sensory symptoms. Clin. Neurol. Neurosurg. 2023;224 doi: 10.1016/j.clineuro.2022.107526. [DOI] [PubMed] [Google Scholar]
- 17.Mousavi S.R., Rezvani A., Eghbal K., Motlagh M.A.S., Dehghanian A.R., Taherpour S., et al. Alternative approach to treatment of unusual site giant cell tumor at cervical spine: a case report and review of literature. J. Craniovertebr. Junct. Spine. 2022;13(2):212–220. doi: 10.4103/jcvjs.jcvjs_45_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mousavi S.R., Liaghat A., Shahpari Motlagh M.A., Pishjoo M., Tarokh A., farrokhi M. Launching the DCER (Distraction, Compression, Extension, and Reduction) technique in basilar invagination and Atlantoaxial dislocation: a preliminary report of two cases in iran. Iran. J. Neurosurg. 2023;9(0):2. [Google Scholar]
- 19.Goel A., Kulkarni A.G., Sharma P. Reduction of fixed atlantoaxial dislocation in 24 cases: technical note. J. Neurosurg. Spine. 2005;2(4):505–509. doi: 10.3171/spi.2005.2.4.0505. [DOI] [PubMed] [Google Scholar]
- 20.Goel A., Figueiredo A., Maheshwari S., Shah A. Atlantoaxial manual realignment in a patient with traumatic atlantoaxial joint disruption. J. Clin. Neurosci. 2010;17(5):672–673. doi: 10.1016/j.jocn.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 21.Lenehan B., Guerin S., Street J., Poynton A. Lateral C1-C2 dislocation complicating a type II odontoid fracture. J. Clin. Neurosci. 2010;17(7):947–949. doi: 10.1016/j.jocn.2009.11.025. [DOI] [PubMed] [Google Scholar]
- 22.Kirankumar M.V., Behari S., Salunke P., Banerji D., Chhabra D.K., Jain V.K. Surgical management of remote, isolated type II odontoid fractures with atlantoaxial dislocation causing cervical compressive myelopathy. Neurosurgery. 2005;56(5):1004–1012. (discussion-12) [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The medical record, laboratory examinations and all the imaging are available on request in DICOM files.