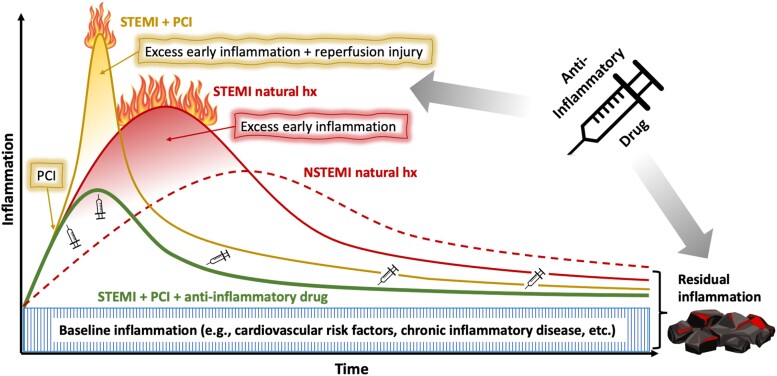
Figure 1.
Putative model for the natural history of ST-segment elevation myocardial infarction vs. non-ST-segment elevation myocardial infarction and the potential effects of percutaneous coronary intervention and anti-inflammatory drugs. Baseline inflammation comprises a chronic level of activity of a patient’s immuno-inflammatory system, determined by traditional cardiovascular risk factors as well as other comorbidities. On top of this chronic inflammation, ST-segment elevation myocardial infarction results in an acute excessive surge of inflammation, both of higher grade and earlier onset compared with non-ST-segment elevation myocardial infarction. Early percutaneous coronary intervention is the gold standard in the treatment of patients with ST-segment elevation myocardial infarction and its beneficial effects on outcome are undisputed. However, percutaneous coronary intervention elicits an additional spike in inflammation caused by local release of inflammatory mediators from balloon and stent expansion, distal microemboli as well as reperfusion injury. Though by far outweighed by the positive aspects of early percutaneous coronary intervention, these effects of reperfusion injury on post-ST-segment elevation myocardial infarction inflammation should not be neglected. Early anti-inflammatory therapy is anticipated to attenuate this early excessive inflammation after ST-segment elevation myocardial infarction. Extending treatment throughout the follow-up period suppresses the residual inflammatory risk (RIR), for which a causal role on patient outcome has been proven. AMI, acute myocardial infarction; hx, history; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction.