Abstract
Background
Overnight, physicians in training receive less direct supervision. Decreased direct supervision requires trainees to appropriately assess patients at risk of clinical deterioration and escalate to supervising physicians. Failure of trainees to escalate contributes to adverse patient safety events.
Objective
To standardize the evaluation of patients at risk of deterioration overnight by internal medicine residents, increase communication between residents and supervising physicians, and improve perceptions of patient safety at a tertiary academic medical center.
Methods
A multidisciplinary stakeholder team developed an overnight escalation-of-care protocol for residents. The protocol was implemented with badge buddies and an educational campaign targeted at residents, supervising physicians, and nursing staff. Residents and supervising physicians completed anonymous surveys to assess the use of the protocol; the frequency of overnight communication between residents and supervising physicians; and perceptions of escalation and patient safety before, immediately after (“early postintervention”), and 8 months after (“delayed postintervention”) the intervention.
Results
Seventy-five (100%) residents participated in the intervention, and 57–89% of those invited to complete surveys at the various time points responded. After the intervention, 82% of residents reported using the protocol, though no change was observed in the frequency of communication between residents and supervising physicians. After the implementation, residents perceived that patient care was safer (early postintervention, 47%; delayed postintervention, 72%; P = 0.02), and interns expressed decreased fear of waking and being criticized by supervising physicians.
Conclusion
An escalation-of-care protocol was developed and successfully implemented using a multimodal approach. The implementation and dissemination of the protocol standardized resident escalation overnight and improved resident-perceived patient safety and interns’ comfort with escalation.
Keywords: escalation of care, residency training, communication, clinical deterioration, patient safety
Physicians in training at teaching hospitals provide frontline care under the guidance of supervising physicians (1). Nighttime hours present a unique challenge to supervision, as supervising physicians may be on call but off site. The adequate management of clinically deteriorating patients requires that trainees accurately assess patients’ medical acuity, make timely treatment decisions, and promptly escalate to supervising physicians.
The Agency for Healthcare Research and Quality has identified the failure of timely response to clinically deteriorating patients as a core contributor to failure-to-rescue events (2). Contributing factors to the failure of timely recognition and response include trainee inexperience, overconfidence, and systemic hierarchical barriers, such as hesitancy to escalate care to senior physicians overnight (3). Trainees may also perceive communication with supervising physicians regarding patient care as unnecessary or unwanted, further exacerbating the failure to escalate care (4–6).
To standardize the evaluation of patients at risk of clinical deterioration overnight, increase communication with supervising physicians, and improve perceptions of patient safety among internal medicine residents at Tufts Medical Center, we developed and implemented an escalation-of-care (EoC) protocol. We describe the development and implementation of this protocol, its effect on communication between residents and supervising physicians, and resultant resident perceptions of escalation and patient safety after its implementation.
Methods
Setting
The EoC protocol was developed and implemented at Tufts Medical Center, a 330-bed tertiary academic medical center in Boston, Massachusetts. The internal medicine residency program comprises 75 residents, distributed evenly across three training years. Night float is from 7 p.m. to 7 a.m. Two interns provide clinical cross-coverage of existing patients who are not critically ill, while new patients are admitted by three second- and third-year residents. This group serves as the first point of contact for patient care concerns, with supervising physicians available for consultation by page but not physically present in the hospital. Auxiliary patient care services include 1) a rapid response team consisting of a certified registered nurse, a respiratory therapist, a pharmacist, a security officer, and a second- or third-year medical resident on night float, and 2) one or two intensivists caring for patients in the intensive care units (ICUs), who may be formally consulted for patients requiring a higher degree of care.
Study Population
All internal medicine interns, residents, and supervising physicians on medical wards (non-ICU) between October 2020 and September 2021 (across two academic years) were eligible to participate in this study. As the care escalation criteria for the medical and cardiac ICUs differ from that of non-ICU settings, protocol development and implementation were restricted to general wards.
Study Intervention: Develop an Overnight EoC Protocol
The quality improvement initiative was led by chief residents with support from leadership within the Department of Medicine and the institutional quality and patient safety department. Free-form stakeholder interviews with approximately 10 supervising physicians, 5 residents across all training years, and 1 nurse leader were performed to ascertain common reasons for patient deterioration and communication among the clinical staff. Twenty-five patient charts containing clinical deterioration events, selected from a review of five night-float residents’ pager logs across one month and five patient safety conferences across six months, were reviewed to identify themes among near-miss and failure-to-rescue patient safety events. Using these themes, a preliminary EoC protocol was developed. The preliminary protocol was reviewed with all stakeholders, and with the residency program and department leadership, with minor amendments to develop the final EoC protocol. The resultant overnight EoC protocol consisted of two parts: 1) situations in which interns should conduct bedside evaluations, including situations in which to involve more senior residents during the assessments, and 2) situations in which residents were expected to notify supervising physicians by page. Additional communication (e.g., phone call) between residents and supervising physicians was left to their discretion. A reminder to write a note for every in-person evaluation was included in the protocol. The development of the protocol occurred between March and September 2020.
Implementation, Part 1: Distribute Educational Material (EoC Protocol) to Interns and Supervising Physicians
The protocol was adapted into a badge buddy, a plastic card that can be affixed to an individual’s hospital-issued identification badge, and distributed to all interns. In addition, posters containing the protocol were displayed in nurse and resident work areas, and the protocol was reviewed during resident educational conferences. Supervising physicians were informed of the protocol via e-mail, during orientation, and during monthly inpatient meetings. Initial implementation of the protocol took place between October and November 2020.
Implementation, Part 2: Scale up the EoC Protocol to All Residents and Nurses
The protocol was disseminated to all residents with badge buddies at educational conferences and subsequently incorporated into annual intern and rising second-year resident orientations. Chief residents educated nurses about the protocol by introducing the protocol to nurse leaders, who then disseminated the protocol to nurses, and conducted nursing huddles to review the poster protocol displayed in nurse work areas. Dissemination of the protocol occurred between February and March 2021 and again in July 2021 for new interns and rising second-year residents.
Outcome Measures
The main outcomes of the study were communication between residents and supervising physicians and residents’ perceptions of the EoC protocol and patient safety, assessed using three anonymous surveys administered before (“preintervention,” February 2020), immediately after (“early postintervention,” December 2020), and 8 months after (“delayed postintervention,” August 2021) the intervention. Gift cards were given to all residents for their participation. Survey measure development relied on the existing body of literature pertaining to trainee escalation for clinically deteriorating patients (7, 8). In addition, select stakeholders (chief residents, Department of Medicine leadership, and the quality and patient safety department) reviewed survey measures before implementation.
All residents on night float before and early after the intervention were invited to complete survey 1 (see Figure E1 in the data supplement) after each night-float shift. Survey 1 assessed 1) whether residents contacted supervising physicians overnight and 2) the reason for initiating contact (multiple choice with “other” option). The number of notifications made to supervising physicians was tallied and reported as the number of notifications per 100 patients, standardized for the hospital discharge census during each survey period (one month).
All supervising physicians scheduled for medicine non-ICU service coverage during the pre- and early postintervention periods were invited to complete survey 2 (see Figure E2) after each week of service. Survey 2 assessed 1) whether supervising physicians believed that the communications they received from residents were appropriate overnight and 2) whether supervising physicians retrospectively wished that they had been contacted for patient care overnight. Although last-minute ward coverage changes may have occurred between supervising physicians, this was assumed to be a rare occurrence, so the percentage of responding supervising physicians was calculated from the total number of physicians scheduled to be on ward services during each intervention period.
All residents, irrespective of clinical rotation, were invited to complete survey 3 (see Figure E3) in the early post- and delayed postintervention periods. Survey 3 assessed general perceptions of escalation during nighttime hours and patient safety using Likert scales (9) (a positive response was defined as the percentage who responded “strongly agree” or “agree”) and open-response format.
Process Measures
The main process measures of the study were 1) carrying the badge buddy and 2) use of the EoC protocol. Process measures were assessed early after the intervention as part of survey 3 (see Figure E3), which all residents were invited to complete anonymously. Survey 3 assessed 1) whether interns carried the EoC protocol badge buddy (assessed only among interns because the initial intervention was limited to interns; carrying the badge buddy was defined as the percentage who responded “yes” or “sometimes”) and 2) whether residents used the EoC protocol overnight using a Likert scale (use was defined as the percentage who responded “always,” “most of the time,” or “sometimes”) (see Figure E3).
Statistical Analysis
Comparisons were made between pre-, early post-, and delayed postintervention surveys using the chi-square test. Analyses were performed using R version (R Core Team) (10).
Ethical Considerations
This work did not constitute human research and was exempt from ethics review by the local institutional review board (study number 00003402). The revised Standards for Quality Improvement Reporting Excellence 2.0 were used to write this report (11).
Results
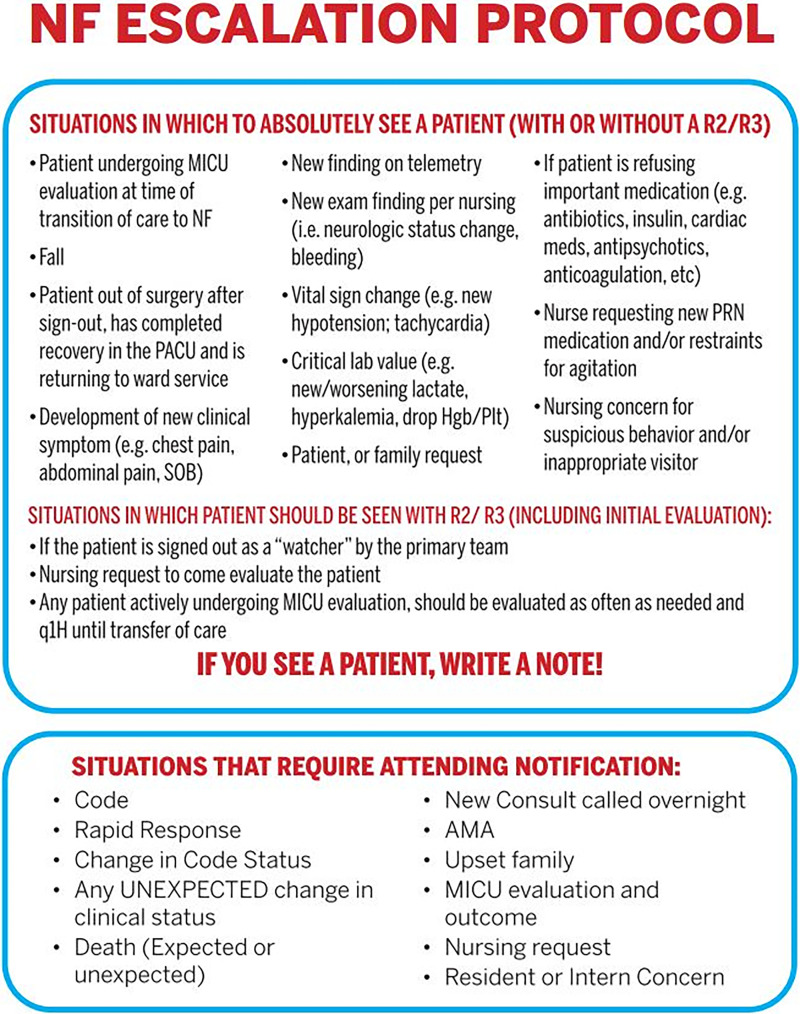
The quality improvement initiative involved 1) development of the EoC protocol, 2) implementation of the protocol (including adaptation into a badge buddy; Figure 1), and 3) dissemination of the protocol across two academic years (Figure 2).
Figure 1.
NF escalation-of-care protocol badge buddy. Notification implies that residents must, at minimum, contact the appropriate supervising physician by page. AMA = against medical advice; Hgb = hemoglobin; MICU = medical intensive care unit; NF = night float; PACU = postanesthesia care unit; Plt = platelets; PRN = pro re nata (as needed); R2 = second-year internal medicine resident; R3 = third-year internal medicine resident; SOB = shortness of breath.
Figure 2.

Framework and timeline of the study. The clinical quality improvement study occurred in three phases: 1) development of the intervention (escalation-of-care [EoC] protocol), 2) implementation of the intervention, and 3) dissemination of the intervention. The EoC protocol was developed over the course of six months. The initial implementation involved distributing educational materials to interns and supervising physicians over the course of one month, three months after which delayed dissemination or scale-up to all residents and nursing staff occurred over the course of one month.
Baseline Data
Seventy-five (100%) residents and 39 supervising physicians participated in the intervention. Before the intervention, 89% of all night-float residents invited to complete survey 1 responded. Residents reported making approximately nine notifications per 100 patients to supervising physicians to escalate patient care, 42% of which were regarding changes in patients’ clinical status. Before the intervention, 56% of supervising physicians invited to complete survey 2 responded and reported that 100% of notifications they received were appropriate, but 22% retrospectively indicated that they wished they had been notified of clinical events that occurred (Table 1).
Table 1.
Process and outcome measures associated with the EoC protocol as assessed by survey responses
| Preintervention (n = 93) (89% Response Rate) |
Early Postintervention (n = 101) (63% Response Rate) |
Delayed Postintervention (n = 43) (57% Response Rate) |
P Value | |
|---|---|---|---|---|
| Process measures | ||||
| Carry badge buddy (PGY 1 only)* | N/A | 69% | 100% | — |
| Use protocol† | ||||
| All trainees | N/A | 82% | — | — |
| PGY 1 | N/A | 69% | — | — |
| PGY 2 | N/A | 86% | — | — |
| PGY 3 | N/A | 89% | — | — |
| Outcome measures: communication | ||||
| Notifications per 100 patients | 9.0 | 9.7 | — | 0.87 |
| Year of trainee made notification | 0.19 | |||
| PGY 1 | 40% | 39% | — | — |
| PGY 2 | 43% | 34% | — | — |
| PGY 3 | 17% | 27% | — | — |
| Reason for notification | 0.76 | |||
| Patient left AMA | 5% | 5% | — | — |
| Patient died | 5% | 2% | — | — |
| Change in patient clinical status | 42% | 51% | — | — |
| Patient transferred to ICU | 31% | 37% | — | — |
| Other | 17% | 20% | — | — |
| Outcome measures: perceptions | ||||
| Notification was appropriate‡ | 100% | 100% | — | 1 |
| Wished they were notified‡ | 22% | 10% | — | 0.09 |
| Fear of criticism by supervising physician | ||||
| All trainees | — | 5% | 5% | 1 |
| PGY 1 | — | 19% | 5% | — |
| PGY 2 | — | 0% | 7% | — |
| PGY 3 | — | 0% | 0% | — |
| Fear of waking supervising physician | ||||
| All trainees | — | 44% | 33% | 0.21 |
| PGY 1 | — | 44% | 21% | — |
| PGY 2 | — | 43% | 40% | — |
| PGY 3 | — | 47% | 44% | — |
| Fear of losing autonomy | ||||
| All trainees | — | 18% | 7% | 0.03 |
| PGY 1 | — | 19% | 0% | — |
| PGY 2 | — | 15% | 13% | — |
| PGY 3 | — | 21% | 11% | — |
| Perceive that patient care is safer | ||||
| All trainees | — | 47% | 72% | 0.02 |
| PGY 1 | — | 63% | 89% | — |
| PGY 2 | — | 43% | 67% | — |
| PGY 3 | — | 32% | 44% | — |
Definition of abbreviations: AMA = against medical advice; EoC = escalation-of-care; ICU = intensive care unit; N/A = not applicable; PGY = postgraduate year.
n = 16 (64%).
n = 55 (73%).
As reported by supervising physicians, n = 18 (56%) before the intervention and n = 21 (66%) early after the intervention.
Process Measures
Early after the intervention, 64% of interns and 73% of all residents (postgraduate year [PGY] 1 through PGY 3) who were invited to complete survey 3 responded. Sixty-nine percent of interns reported carrying the badge buddy, and 82% (PGY 1, 69%; PGY 2, 86%; and PGY 3, 89%) of all residents reported using the protocol.
Outcome Measures
Of all residents in the early postintervention period on night float invited to complete survey 1, 63% responded. Neither a significant change in the number of notifications (preintervention, 9; early postintervention, 9.7; P = 0.87) nor a significant change in the reason for notification was observed (Table 1). Early after the intervention, fewer supervising physicians indicated that they wished they had been called for clinical events (preintervention, 22%; early postintervention, 10%; P = 0.09), and none reported any instance of inappropriate notification overnight with implementation of the protocol (Table 1).
In the delayed postintervention period, 57% of residents who were invited to complete survey 3 responded. Between the early post- and delayed postintervention periods, fear of criticism and fear of waking the supervising physician did not significantly change across all trainee years, but the percentage of interns who reported fear of criticism (early postintervention, 19%; delayed postintervention, 5%) or fear of waking the supervising physician (early postintervention, 44%; delayed postintervention, 21%) decreased. In addition, fear of losing autonomy significantly decreased across all trainee years (early postintervention, 18%; delayed postintervention, 7%; P = 0.03) (Table 1), and residents perceived that patient care was safer as a result of the protocol (early postintervention, 47%; delayed postintervention, 72%; P = 0.02).
Discussion
We describe an EoC protocol with intended use by internal medicine residents on general wards, the product of a multidisciplinary team with stakeholder input. The aim of the protocol was to standardize the evaluation of patients at risk of clinical deterioration, increase communication between residents and supervising physicians overnight, and improve perceptions of patient safety among residents. We hypothesize that the strategic involvement of stakeholders engaged in patient care, especially residents, contributed to the high rate of protocol use by residents after a single change cycle (82% across all trainee years; Table 1).
Although we do not report a significant increase in communication between residents and supervising physicians after implementation of the EoC protocol, the number of notifications to supervising physicians was assessed only during the early postintervention period, merely one month after the implementation of the protocol. Therefore, the overall impact of the protocol on the rate of communication between residents and supervising physicians may not have been captured during the data collection period. In addition, this nonsignificant finding may be greatly confounded by varying degrees of patient acuity and uncertainty regarding the management of patients admitted with symptomatic severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection during the pre- and early postintervention phases, which we were unable to account for in our analyses. However, we did report that fewer supervising physicians wished that they had been contacted after implementation of the protocol, with no increase in reported inappropriate communication overnight as a result of the protocol.
As has previously been identified, systemic hierarchical barriers are a known contributing factor to failure-to-rescue events (3). Here, we demonstrate that the implementation and dissemination of the EoC protocol decreased the fear of waking the supervising physician, with little effect on decreasing the fear of criticism by the supervising physician, although the baseline rate of this perception among our residents was low. Importantly, our results suggest heterogeneity of intervention effect across trainee year. Interns demonstrated the greatest reductions in fear of criticism, fear of waking the supervising physician, and fear of loss of autonomy, with the greatest improvement in perceptions of patient safety. The collective implication of our findings is that the EoC protocol may be an effective tool to address persistent hierarchical barriers between trainees and supervising physicians, especially as perceived by interns during nighttime hours.
Lending to their convenience and inexpensive nature, the use of badge buddies to effect change is appealing. We used the badge buddy as a single component of a multifaceted educational campaign to implement our intervention. The efficacy of badge buddies alone is difficult to elucidate from our project. As in our work, others have used badge buddies as a single component of larger educational campaigns, with mixed efficacy for effecting change in clinical quality improvement (12–15).
Strengths and Limitations
The primary limitations of our study are the self-reported nature of the objective outcomes and the otherwise subjective, semiquantitative nature of perceptions. Measurement and interpretation of such outcomes are susceptible to the Hawthorne effect, in which study participants, knowing that they are being observed, may modify their behavior and responses. All surveys were administered anonymously to reduce the risk of this bias. In addition, given that residents’ fears and perceptions of patient safety were not assessed before the intervention, we are unable to report the absolute change in perceptions before and after the intervention, only a trend in the postintervention period. We cannot exclude the possibility that residents, when prompted by the protocol to communicate with supervising physicians, initially experienced increased fear related to communication during nighttime hours but, once these fears were not realized between the early post- and delayed postintervention periods, reported decreased fear of communication in relation to the early postintervention period but potentially unchanged from preintervention. Last, the generalizability of this institutional protocol is limited given that the structure and auxiliary services for patient care overnight may differ at other institutions.
Conclusions
We demonstrated an overall trend toward decreased systemic hierarchical barriers, especially among interns, with the implementation of an EoC protocol at our institution. To ensure that the intervention is sustained, badge buddies containing the EoC protocol are provided to each incoming resident class, every new supervising physician, and new nurses in non-ICU settings. Next steps include evaluating the impact of the EoC protocol on rapid response, ICU transfer, and code-blue rates in non-ICU settings.
Footnotes
Supported by a Tufts Medical Center Claims Committee Risk Management Grant and National Center for Advancing Translational Sciences, National Institutes of Health, grant TL1TR002546.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Halpern SD, Detsky AS. Graded autonomy in medical education—managing things that go bump in the night. N Engl J Med . 2014;370:1086–1089. doi: 10.1056/NEJMp1315408. [DOI] [PubMed] [Google Scholar]
- 2. Burke JR, Downey C, Almoudaris AM. Failure to rescue deteriorating patients: a systematic review of root causes and improvement strategies. J Patient Saf . 2022;18:e140–e155. doi: 10.1097/PTS.0000000000000720. [DOI] [PubMed] [Google Scholar]
- 3. Johnston MJ, Arora S, King D, Bouras G, Almoudaris AM, Davis R, et al. A systematic review to identify the factors that affect failure to rescue and escalation of care in surgery. Surgery . 2015;157:752–763. doi: 10.1016/j.surg.2014.10.017. [DOI] [PubMed] [Google Scholar]
- 4. Farnan JM, Johnson JK, Meltzer DO, Humphrey HJ, Arora VM. On-call supervision and resident autonomy: from micromanager to absentee attending. Am J Med . 2009;122:784–788. doi: 10.1016/j.amjmed.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 5. Kilminster S, Cottrell D, Grant J, Jolly B. AMEE guide no. 27: effective educational and clinical supervision. Med Teach . 2007;29:2–19. doi: 10.1080/01421590701210907. [DOI] [PubMed] [Google Scholar]
- 6. Loo L, Puri N, Kim DI, Kawayeh A, Baz S, Hegstad D. “Page me if you need me”: the hidden curriculum of attending-resident communication. J Grad Med Educ . 2012;4:340–345. doi: 10.4300/JGME-D-11-00175.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rotella JA, Yu W, Ferguson J, Jones D. Factors influencing escalation of care by junior medical officers. Anaesth Intensive Care . 2014;42:723–729. doi: 10.1177/0310057X1404200607. [DOI] [PubMed] [Google Scholar]
- 8. Senders ZJ, Aeder M, Semrau S, Ammori J. Improving resident-to-attending communication: implementing a tool to facilitate attending notification of critical patient events at a single academic institution. Am Surg . 2019;85:663–670. [PubMed] [Google Scholar]
- 9. Likert R. A technique for the measurement of attitudes. Arch Psychol . 1932;140:5–55. [Google Scholar]
- 10.R Core Team. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2022. https://www.r-project.org [Google Scholar]
- 11. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for Quality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf . 2016;25:986–992. doi: 10.1136/bmjqs-2015-004411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Evans A, Vingelen MB, Yu C, Baird J, Murray P, Bryant P. Nausea in numbers: electronic medical record nausea and vomiting assessment for children with cancer. J Pediatr Oncol Nurs . 2020;37:195–203. doi: 10.1177/1043454219900467. [DOI] [PubMed] [Google Scholar]
- 13. Bates AN, Ercolano E. Development and implementation of a simple wound care guideline for minor skin lesions: a quality improvement project. J Wound Ostomy Continence Nurs . 2021;48:285–291. doi: 10.1097/WON.0000000000000778. [DOI] [PubMed] [Google Scholar]
- 14. Arquiette JM, Moss HA, Truong T, Pieper CF, Havrilesky LJ. Impact of a documentation intervention on health-assessment metrics on an inpatient gynecologic oncology service. Gynecol Oncol . 2019;153:385–390. doi: 10.1016/j.ygyno.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 15. Sadeghi C, Khan HA, Gudleski G, Reynolds JL, Bakhai SY. Multifaceted strategies to improve blood pressure control in a primary care clinic: a quality improvement project. Int J Cardiol Hypertens . 2020;7:100060. doi: 10.1016/j.ijchy.2020.100060. [DOI] [PMC free article] [PubMed] [Google Scholar]