Abstract
Objective
The study objective was to describe the implementation and results of a postoperative telemedicine program for adult cardiac surgery, including a clinical study and an organic postoperative telemedicine program aimed at reducing readmission rates and barriers to care.
Methods
Patients undergoing coronary artery bypass grafting consented to enrollment in our Perfect Care study funded by The Duke Endowment including advanced practice provider–led postdischarge telemedicine services with data collection. There were 2 telemedicine visits at days 3 and 10 postdischarge using a live face-to-face video platform. Patients were provided with home wearables for heart rate monitoring, blood pressure cuffs, and scales. The success of the Perfect Care study led to the formation of our organic program, the Tele Heart Care, which was adapted to include a larger patient population while remaining structurally similar.
Results
Fifty patients were enrolled prospectively between January and October 2021 in Perfect Care. The 30-day readmission rates for those enrolled was 4% compared with a 16% readmission rate for nonenrolled patients during this period. Furthermore, 36% of enrolled patients received medication modifications to optimize blood pressure, heart rate and rhythm, and fluid-volume status, or to treat infectious symptoms. Tele Heart Care enrolled 203 patients and was associated with a decrease in 30-day readmission rates in all cardiac surgery patients at our institution from 24% to 4% over a 6-month period.
Conclusions
An advanced practice provider–led postdischarge telemedicine program after cardiac surgery can reduce hospital readmission and barriers to care, and improve patient satisfaction. With involvement of multiple stakeholders, a successful program can be launched despite the present state of national health system finances with limited human capital and constrained access to monitoring equipment.
Key Words: barriers to care, CABG, cardiac surgery, readmission, Telehealth, telemedicine
Graphical Abstract
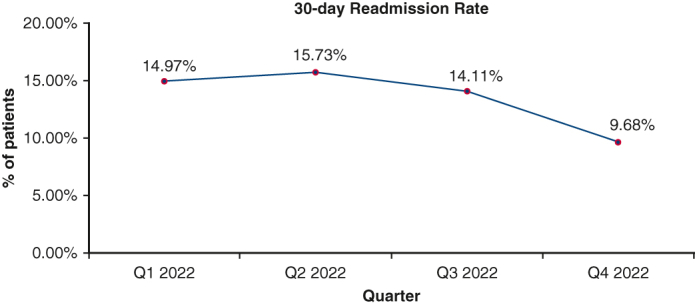
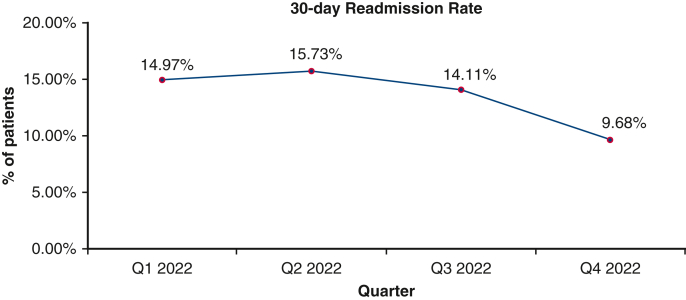
The 30-day readmission rates in our cardiac surgery department shown by quarter showing a decrease from 15.73% in Q2 right before Tele Heart Care implementation to 9.68% in Q4 after Tele Heart Care implementation.
Central Message.
A postoperative telemedicine program after cardiac surgery can reduce hospital readmission and barriers to care, and improve patient satisfaction.
Perspective.
Telemedicine has been shown to provide benefits to both patients and healthcare systems while remaining clinically effective, and has become a significant modality for patient care. A postoperative telemedicine program after cardiac surgery can reduce hospital readmission and barriers to care, and improve patient satisfaction.
See Discussion on page 507.
Telemedicine has become a significant modality for patient care outside of the hospital environment, and its implementation in surgical care has increased in recent years.1 Postoperative telemedicine is shown in selected settings to provide benefits to both patients and healthcare systems while remaining safe and effective.2 Postoperative follow-up after cardiac surgery is critical, and strategies for early detection and management of complications are needed.3 Diagnosis and treatment of postsurgical complications have been shown possible through telemedicine alone without compromising the patient's perceptions of his/her quality of care.1,4
Telehealth is a viable method for follow-up after discharge to expedite recovery.5 Hospital 30-day readmission rates after cardiac surgery range between 8% and 29% and may be higher in some places.3 Factors predictive of readmission are increasing age, female gender, renal failure, prior heart failure or myocardial infarction, and diabetes.3 Patient follow-up within 1 week after discharge for those at high risk of readmission has been shown to reduce the rate of readmission after open surgery.6 Additional benefits of postoperative telemedicine include saving time and expense for both patients and providers along with increasing access to care. Eliminating barriers to telemedicine can increase its use and therefore afford better access to care and more timely interventions for complications.7
Although recent medical literature supports the use of postoperative telemedicine to assess time-sensitive conditions so they may be addressed in a timely manner to prevent hospital readmission, cardiac surgery is a field often omitted when assessing telemedicine feasibility.2,8, 9, 10 The majority of postoperative telemedicine programs make use of telephone calls and automated surveys, which carry limited utility for assessment. As such, we sought out a strategy to improve timely access to postoperative care of cardiac surgery patients. We describe the trial implementation and results of a postoperative telemedicine program aimed at reducing readmission rates and barriers to care for the adult cardiac surgery population. We hypothesize that the implementation of a postoperative telemedicine program will reduce readmission rates and barriers to care for the adult cardiac surgery population at our institution.
Material and Methods
Our institution conducted a Perfect Care study supported by funding from the Duke Endowment.11 Patients undergoing coronary artery bypass grafting (CABG) who had a discharge disposition of home without home health were considered for enrollment. Further inclusion criteria included access to a smartphone, connection to Wi-Fi, device Bluetooth connectivity, and ability to navigate their smartphone device. This study was determined to be quality improvement by the Institutional Review Board (February 11, 2019); individual consent was not required.
All patients were provided with home wearables for heart rate monitoring, blood pressure (BP) cuffs, and scales. These home wearables were configured for patients before they left the hospital to ensure proper initial setup. The wearables connected directly to a smartphone application that consistently monitored vital signs throughout the day. This application communicated vital signs with abnormal parameters directly to a clinician, and a clinician checked all parameters from the application at least once daily. If abnormal parameters were measured, they were sent directly to the advanced practice provider (APP) who monitored them during business hours. Other parameters not automatically monitored through provided home wearables but available for input into the app were temperatures, blood glucose, and oxygen saturations.
Patients agreed to telemedicine visits at approximately days 3 and 10 after hospital discharge that were scheduled before the patient left the hospital. The platform for visits used the existing hospital electronic medical record (EMR) framework (Epic) via live face-to-face video. Before the visit, patients received a survey through the monitoring app asking targeted questions for infection, fluid overload, arrhythmias, pain, and malaise. The option to upload pictures of surgical incisions was also included. Visits were conducted as regular follow-up checks along with review of medications for adherence and any needs for adjustments based on vital signs and survey results. After the visit, patients received surveys through the app to rate their satisfaction with their experience.
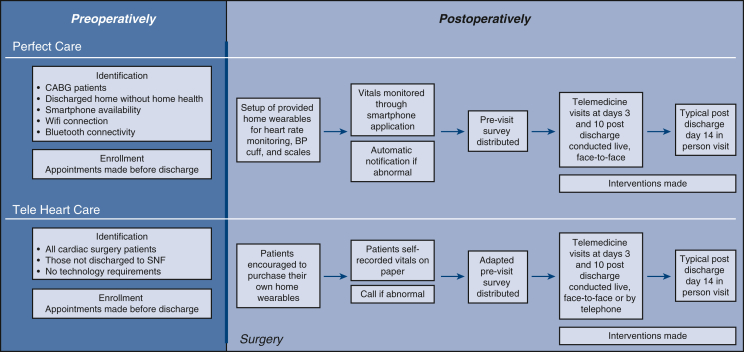
After presentation of these study results to our health system administration, funding was granted for a full-time APP position to lead a postdischarge telemedicine program, termed “Tele Heart Care” (Figure 1). With human resource funding in place, the following interdisciplinary stakeholders engaged in program development from trial phase to practice: social work, case management, outpatient clinical staff, physical therapy, quality analytics, nurse educators, patients, and physician champions.
Figure 1.

The Tele Heart Care logo used at WakeMed Health and Hospitals.
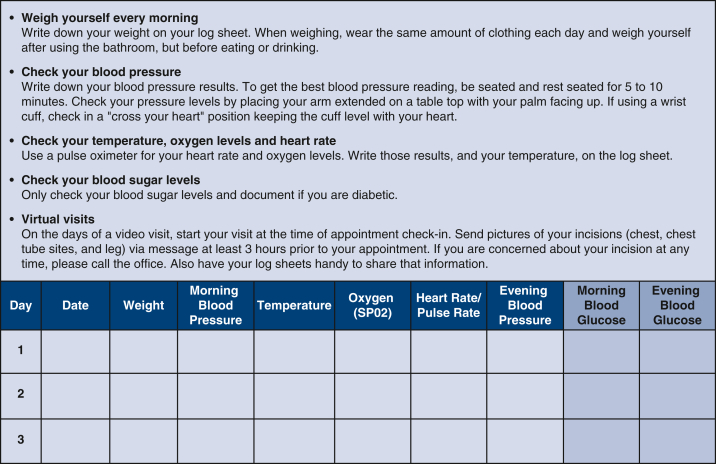
Our cardiac surgery department implemented Tele Heart Care for all cardiac surgery patients, not just those who were thought to be sufficiently technologically savvy. Those without access to a smart device or internet were offered the opportunity to participate in a telephone visit. The only exclusion criterion was patients who were discharged to a skilled nursing facility. Remote monitoring was possible for all patients despite cost constraints after being afforded grant funding (WakeMed Foundation, wakemedfoundation.org) with wearables made available to patients who could not afford to buy them on their own. Patient educational materials were created to include a flyer encouraging patients to obtain their own devices as well as a daily log whereby data points and vital sign measurements were to be recorded and subsequently reviewed at telemedicine visits (Figure 2). Collaboration with our institutional IT department allowed us to create a specific EMR visit type with a patient questionnaire tailored to a pertinent review of systems, adapted from the Perfect Care study previsit survey. Patients were encouraged to upload pictures of their incisions to the EMR software portal (Figure 3).
Figure 2.
An excerpt from the Tele Heart Care flyer aimed at encouraging patients to check their vital signs and record them on a log. A 3-day example of the log is also shown, which will be reviewed during the telemedicine visit.
Figure 3.
Methods and process for both Perfect Care and Tele Heart Care from patient identification and enrollment preoperatively to completion of telemedicine visits postoperatively with included typical postoperative in-person follow-up. CABG, Coronary artery bypass grafting; BP, blood pressure; SNF, skilled nursing facility.
Data are reported as percentages with the purpose of presenting clinical results and methods for incorporation into practice. No statistical analyses were conducted for these data, and no statistical significance was determined.
Results
Perfect Care
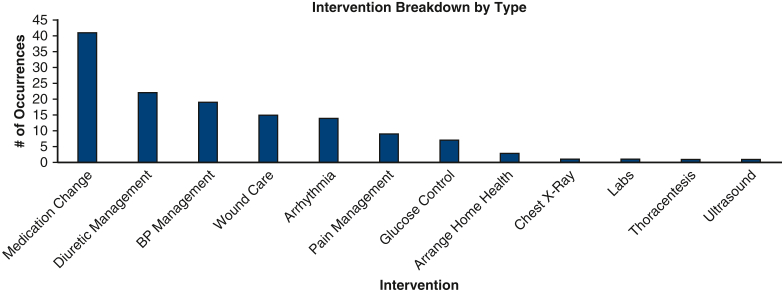
The Perfect Care study enrolled 50 patients from January to October 2021 (Table 1). Forty participants were male and 10 were female, with a mean age of 61 years (SD = 11). A total of 74% of those enrolled were White, 14% were African American, 4% were Asian, and 8% were other. The mean Society of Thoracic Surgeons (STS) predicted risk of mortality was calculated for those in the Perfect Care cohort undergoing isolated CABG (n = 39) and was calculated as 0.8%. The mean STS predicted risk of mortality for those not enrolled in Perfect Care during this time, but still eligible due to a home discharge status, and who underwent isolated CABG (n = 110) was 1.8%. Interventions done as a result of the telemedicine visits in decreasing order of prevalence include medication adjustment, diuretic management, BP management, wound care, arrhythmia management, pain management, glucose control, arranging home services, chest x-ray, lab work, thoracentesis, and ultrasound (Figure 4). Many patients required more than 1 intervention. Some 36% of patients had medication modifications to optimize BP, heart rate, or rhythm or to combat fluid-volume overload or treat minor infectious symptoms. The 30-day readmission rates postoperatively for those enrolled was 4% (1 due to an non–ST-elevation myocardial infarction and 1 due to a pulmonary embolism) compared with a 16% readmission rate at our institution for nonenrolled patients with home discharge during this period. The Perfect Care study cohort mortality rate was 0%. With regard to patient satisfaction, 36 patients completed the postvisit survey. Some 97% of respondents reported having a good, a very good, or an excellent overall healthcare experience with 3% indicating a fair or poor experience. Some 89% of respondents indicated their experience with the remote monitoring devices as good or excellent, and 11% rated it as fair or poor.
Table 1.
Participants demographics comparison between the Perfect Care study and Tele Heart Care
| Intervention | Category | Value |
|---|---|---|
| Perfect Care | Total participants | 50 |
| Male | 40 | |
| Female | 10 | |
| Mean age | 61 y (SD = 11) | |
| White | 74% | |
| African American | 14% | |
| Asian | 4% | |
| Other | 8% | |
| Tele Heart Care | Total participants | 203 |
| Male | 144 | |
| Female | 59 | |
| Mean age | 65 y (SD = 10) | |
| White | 76% | |
| African American | 17% | |
| Asian | 3% | |
| Other | 4% |
Figure 4.
Interventions made as a result of telemedicine visits during the Perfect Care study categorized by type in decreasing order of prevalence by number of occurrences. BP, Blood pressure.
Tele Heart Care
Tele Heart Care went live June 2022 with 203 patients enrolled (Table 1). Of the 83 patients who underwent cardiac surgery who were not enrolled, reasons for this included discharge to a skilled nursing facility, not answering their phone to confirm or complete the visit, or the patient opted not to participate. Of the 203 patients, 144 were male and 59 were female with a mean age of 65 years (SD = 10); 76% were White, 17% were African American, 3% were Asian, and 4% were other. Over the 6-month period between June 2022 and December 2022, readmission rates of all cardiac surgery patients at our institution regardless of discharge disposition decreased from 24% in June to 4% in December and from 15.73% in Q2 to 9.68% in Q4 (Figure 5). With regard to postdischarge return to the emergency department, 12% of patients not enrolled returned, whereas only 7% of those enrolled returned.
Figure 5.
The 30-day readmission rates in our cardiac surgery department shown by quarter showing a decrease from 15.73% in Q2 right before Tele Heart Care implementation to 9.68% in Q4 after Tele Heart Care implementation.
Discussion
The Perfect Care study implemented telemedicine visits at days 3 and 10 postcardiac surgery discharge and was associated with a reduction in 30-day readmission rates for those enrolled, which encouraged the development of our Tele Heart Care program that supported this reduction in 30-day readmission rates. We found that a telemedicine program for early postoperative care of the cardiac surgery patient carries important utility for better patient care, including improved outcomes and improved patient satisfaction scores, in contrast to prior suggestions that the role of telemedicine is best placed in long-term follow-up settings (Figure 6).
Figure 6.
Graphical abstract providing an overview of the telemedicine process and important findings. APP, Advanced practice provider.
On the contrary, Telehealth in this study was used to augment care in the early period between discharge and a patient's usual in-person follow-up with their surgeon at approximately postoperative week 4. The creation of a comprehensive postdischarge telemedicine program inclusive of those who underwent adult cardiac surgical intervention necessitated the inclusion of multiple stakeholders, a critical component of program success. Multidisciplinary care and patient involvement in the management of their health are both augmented by telemedicine and previously shown to sustain reduction in readmissions.12 By the continuous collection of vital signs as opposed to only reviewing data points at postoperative visits, providers are able to detect any alarming trends and intervene quicker. Images in medicine proved helpful for not only patients but also the large number of team members involved in the care of patients undergoing cardiac surgery (Figure 1, Figure 2, Figure 3).
Developing an organic postdischarge telemedicine program without trial resources posed a number of obstacles that were ultimately overcome. It proved difficult to secure funding to outright provide monitoring devices universally to the population. Third-party payer reimbursement was investigated but was not widely available on most plans to include Medicare. As such, a process was created encouraging patients preoperatively to purchase or secure access to their own personal scale, BP cuff, and pulse oximeter. Recognizing the vulnerability of those without the resources to secure such devices, nonprofit grant funding was secured to provide a limited supply of scales, BP cuffs, and pulse oximeters to those patients unable to purchase for themselves. We found that the majority of patients were able and willing to secure their own medical monitoring devices. Affordability, without compromising clinical outcomes, is essential for a telemedicine care model to be a viable option for healthcare delivery.
The Perfect Care study patient population was largely male and White and as such may not be generalizable to the larger public, but the real-world results from our organic Tele Heart Care program with a diverse population indicate broad benefits. In addition, this study was limited to cardiac surgery, but it is suggested that this same model would be effective for other specialties. However, barriers to telemedicine implementation and adoption still exist. A systematic review found that the highest frequency patient barrier is age, followed by level of education and computer literacy.13 In efforts to combat this, we offered the opportunity for patients to conduct visits via telephone for those who are not able to access Wi-Fi or work-smart technology. The same review found that the highest frequency organizational barrier is cost, followed by reimbursement, legal liability, and privacy confidentiality.13 Patients participating in Tele Heart Care who went home by themselves or with home care experienced a difference in average direct variable cost of $7000 or lower for the period between June 2022 and March 2023. By using the EMR for patient interactions and visits, we remained Health Insurance Portability and Accountability Act compliant and protected patient health information. By allowing patients to conduct visits within their own home, patients may personalize their attendees to allow more participation from their support group, such as family members or caretakers.14 A decrease in the number of scheduled clinic visits can make a significant impact on improving access to surgical services.2
Other surgical specialties have conducted research on optimal positioning for mobile evaluation of surgical sites.15 Both patient and provider education are necessary for successful adoption. Patient satisfaction is essential for telemedicine to be a viable mode of healthcare delivery and should remain a focus for telemedicine programs in the future. Travel cost, absence from everyday activity, and dependence on others are all barriers to access to healthcare, and the Tele Heart Care program we describe may improve access for underserved cohorts.8 The need remains for definition of and action toward provider reimbursement, insurance coverage, data management guidelines, and guidance on care across state lines.
Study Limitations
A limitation in the interpretation of the data and processes presented includes a potential concomitant benefit to patients from a robust infection prevention initiative as well in an existing enhanced recovery after surgery cardiac pathway.16,17 No a priori statistical assumptions were made for either study, and as such statistical significance was not calculated. Additionally, the Perfect Care study participants were required to be smart technology proficient and therefore may have inherently higher socioeconomic status, introducing bias. This bias was attempted to be mitigated by removing the requirement for smart technology proficiency for participation in Tele Heart Care. The calculated STS predicted risk of mortality was lower for those enrolled in Perfect Care than those not enrolled; however, this may be skewed because it was only for isolated CABG, and scores were not calculated for the 22% of the enrolled population undergoing additional procedures. This study was conducted at a large community-based health system, and each institution's organization structure varies, which could play a significant role in the implementation of a telemedicine program. Ultimately, telemedicine may be implemented in whichever way fits an institution best. Finally, technical literacy is often associated with age and socioeconomic status, and we acknowledge the importance of research in overcoming this obstacle for patients.
Conclusions
An APP-led postdischarge telemedicine program after cardiac surgery can reduce hospital readmission and barriers to care, and improve patient satisfaction. With involvement of multiple stakeholders, a successful program can be launched despite the present state of national health system finances with limited human capital and constrained access to monitoring equipment. Increased follow-up intervals are made possible by telemedicine.
Conflict of Interest Statement
The authors reported no conflicts of interest.
The Journal policy requires editors and reviewers to disclose conflicts of interest and to decline handling or reviewing manuscripts for which they may have a conflict of interest. The editors and reviewers of this article have no conflicts of interest.
Footnotes
Funding: Perfect Care Collaborative and WakeMed Clinical Research Institute.
References
- 1.Sallam A., Shang M., Vallabhajosyula I., Mori M., Chinian R., Assi R., et al. Telemedicine in the era of coronavirus 19: implications for postoperative care in cardiac surgery. J Card Surg. 2021;36:3731–3737. doi: 10.1111/jocs.15875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gunter R.L., Fernandes-Taylor S., Rahman S., Awoyinka L., Bennett K.M., Weber S.M., et al. Feasibility of an image-based mobile health protocol for postoperative wound monitoring. J Am Coll Surg. 2018;226:277–286. doi: 10.1016/j.jamcollsurg.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Trooboff S.W., Magnus P.C., Ross C.S., Chaisson K., Kramer R.S., Helm R.E., et al. A multi-center analysis of readmission after cardiac surgery: experience of The Northern New England Cardiovascular Disease Study Group. J Card Surg. 2019;34:655–662. doi: 10.1111/jocs.14086. [DOI] [PubMed] [Google Scholar]
- 4.Hwa K., Wren S.M. Telehealth follow-up in lieu of postoperative clinic visit for ambulatory surgery: results of a pilot program. JAMA Surg. 2013;148:823–827. doi: 10.1001/jamasurg.2013.2672. [DOI] [PubMed] [Google Scholar]
- 5.George I., Salna M., Kobsa S., Deroo S., Kriegel J., Blitzer D., et al. The rapid transformation of cardiac surgery practice in the coronavirus disease 2019 (COVID-19) pandemic: insights and clinical strategies from a centre at the epicentre. Eur J Cardio Thorac Surg. 2020;58:667–675. doi: 10.1093/ejcts/ezaa228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borregaard B., Dahl J.S., Riber L.P.S., Ekholm O., Sibilitz K.L., Weiss M., et al. Effect of early, individualized and intensified follow-up after open heart valve surgery on unplanned cardiac hospital readmissions and all-cause mortality. Int J Cardiol. 2019;289:30–36. doi: 10.1016/j.ijcard.2019.02.056. [DOI] [PubMed] [Google Scholar]
- 7.Atilgan K., Onuk B.E., Köksal Coşkun P., Yeşi̇l F.G., Aslan C., Çolak A., et al. Remote patient monitoring after cardiac surgery: the utility of a novel telemedicine system. J Card Surg. 2021;36:4226–4234. doi: 10.1111/jocs.15962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orlando J.F., Beard M., Kumar S. Systematic review of patient and caregivers’ satisfaction with telehealth videoconferencing as a mode of service delivery in managing patients’ health. PLoS One. 2019;14 doi: 10.1371/journal.pone.0221848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Russo J.E., McCool R.R., Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E Health. 2016;22:209–215. doi: 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
- 10.Smith S.M., Jacobsen J.H.W., Atlas A.P., Khoja A., Kovoor J.G., Tivey D.R., et al. Telehealth in surgery: an umbrella review. ANZ J Surg. 2021;91:2360–2375. doi: 10.1111/ans.17217. [DOI] [PubMed] [Google Scholar]
- 11.Perfect care. Accessed April 28, 2023. https://perfectcare.org/
- 12.Bates O.L., O'Connor N., Dunn D., Hasenau S.M. Applying STAAR interventions in incremental bundles: improving post-CABG surgical patient care. Worldviews Evid Based Nurs. 2014;11:89–97. doi: 10.1111/wvn.12028. [DOI] [PubMed] [Google Scholar]
- 13.Kruse C., Heinemann K. Facilitators and barriers to the adoption of telemedicine during the first year of COVID-19: systematic review. J Med Internet Res. 2022;24 doi: 10.2196/31752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lattouf O.M. Telemedicine in the era of coronavirus 19: implications for postoperative care in cardiac surgery. J Card Surg. 2021;36:3738–3739. doi: 10.1111/jocs.15873. [DOI] [PubMed] [Google Scholar]
- 15.Zhu C., Williamson J., Lin A., Bush K., Hakim A., Upadhyaya K., et al. Implications for telemedicine for surgery patients after COVID-19: survey of patient and provider experiences. Am Surg. 2020;86:907–915. doi: 10.1177/0003134820945196. [DOI] [PubMed] [Google Scholar]
- 16.Downing M., Modrow M., Thompson-Brazill K.A., Ledford J.E., Harr C.D., Williams J.B. Eliminating sternal wound infections: why every cardiac surgery program needs an “I Hate Infections Team” (IHIT) JTCVS Tech. 2023;19:93–103. doi: 10.1016/j.xjtc.2023.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Williams J.B., McConnell G., Woltz P., Allender J., Smith P.K., Engelman D.T., et al. Early results from the first US-based enhance recovery after cardiac surgery program. J Thorac Cardiovasc Surg. 2019;157:1881–1888. doi: 10.1016/j.jtcvs.2018.10.164. [DOI] [PubMed] [Google Scholar]