Abstract
Introduction:
Post-anaesthesia care unit (PACU) delirium affects 5%–45% of patients after surgery and is associated with postoperative delirium and increased mortality. Up to 40% of PACU delirium is preventable, but it remains under-recognised due to a lack of awareness of its diagnosis. The nursing delirium screening scale (Nu-DESC) has been validated for diagnosing PACU delirium, but is not routinely used locally. This study aimed to use Nu-DESC to establish the incidence and risk factors of PACU delirium in patients undergoing non-cardiac surgery in the surgical population.
Methods:
We conducted an audit of eligible patients undergoing major surgery in three public hospitals in Singapore over 1 week. Patients were assessed for delirium 30–60 min following their arrival in PACU using Nu-DESC, with a total score of ≥2 indicative of delirium.
Results:
A total of 478 patients were assessed. The overall incidence rate of PACU delirium was 18/478 (3.8%), and the incidence was 9/146 (6.2%) in patients aged > 65 years. Post-anaesthesia care unit delirium was more common in females, patients with malignancy and those who underwent longer operations. Logistic regression analysis showed that the use of bispectral index (P < 0.001) and the presence of malignancy (P < 0.001) were significantly associated with a higher incidence of PACU delirium.
Conclusion:
In this first local study, the incidence of PACU delirium was 3.8%, increasing to 6.2% in those aged > 65 years. Understanding these risk factors will form the basis for which protocols can be established to optimise resource management and prevent long-term morbidities and mortality in PACU delirium.
Keywords: Geriatrics, major non-cardiac surgery, postoperative delirium
INTRODUCTION
Post-anaesthesia care unit (PACU) delirium affects 5%–45%[1-3] of patients after surgery. It is associated with postoperative delirium (POD),[2,4] with its attendant poor outcomes of increased hospital length of stay, increased 30-day mortality[5] and long-term progression to dementia.[6] Up to 10% of these patients may develop long-term neurocognitive deficits and have a diminished quality of life, and they pose a tremendous socioeconomic burden on their families and caregivers.[6,7]
With an increasingly ageing population (globally and locally) requiring surgery, the problem of PACU delirium and POD is set to increase. This has led to several guidelines being promulgated to address this issue, including the Brain Health Initiative[8] and the Safe Brain Initiative.[9] Up to 40% of POD is preventable,[10] but POD is often underdiagnosed, partly due to a lack of awareness and an absence of established biomarkers or monitors for detection. The nursing delirium screening scale (Nu-DESC) has been validated as a quick and easy screening tool that can be performed within 2 min [Figure 1]. In postoperative patients, it has a sensitivity and specificity of 98% and 92%, respectively, with a total score of ≥2 indicative of delirium.[2]
Figure 1.
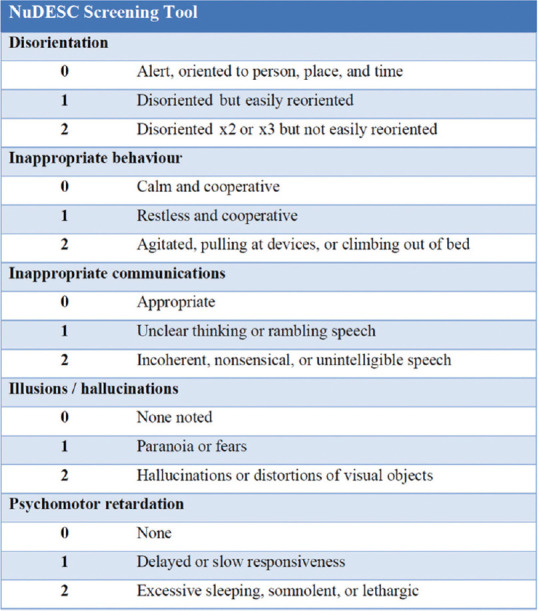
Diagram shows the nursing delirium screening scale (Nu-DESC). [Adapted from Gaudreau et al][7]
We aimed to use Nu-DESC to understand the incidence of PACU delirium after major non-cardiac surgery and its associated risk factors in the local context.
METHODS
The study was conducted in the National University Hospital, Khoo Teck Puat Hospital and Tan Tock Seng Hospital, Singapore, over a period of 1 week. Ethics approval was obtained from the domain specific review board (reference number 2020/00320), which waived written consent requirement.
All patients aged 21 years and above presenting for non-cardiac surgery in major operating theatres were recruited. The exclusion criteria were patients: (a) undergoing neurosurgical procedures of the brain or electroconvulsive therapy; (b) undergoing surgery performed under local anaesthesia and; (c) who were mechanically ventilated in PACU or stayed in PACU for less than 10 min. Other preoperative details such as patient’s existing comorbidities, operative details such as surgical discipline, type of anaesthesia and duration of surgery, and PACU details such as length of stay in PACU and discharge destination were collected. The use of depth of anaesthesia monitoring with bispectral index (BIS) was also recorded.
All eligible patients were assessed for PACU delirium 30–60 min upon arrival in PACU using Nu-DESC. The test was conducted by doctors and nurses participating in the patient’s care. Delirium was evaluated based on observation of the following five features: (a) disorientation, (b) inappropriate behaviour, (c) inappropriate communication, (d) illusions/ hallucinations, and (e) psychomotor retardation. Each item was scored based on its severity of 0–2. A total score of ≥2 was classified as positive for POD [Figure 1].
All data were entered into a statistical software program, with analysis, statistical computing and visualisations carried out in R environment version 1.2.1335 (The R Foundation for Statistical Computing, Vienna, Austria). Continuous variables were presented as median (interquartile range) and the Mann–Whitney U test was used to test the mean differences between the groups. For categorical variables, the chi-test was used to compare the proportions between the groups. Multivariate logistic regression was performed to determine the independent predictors for POD. Factors with P <0.1 from the univariate analysis were included in the multivariate regression models. The effect size was reported as odds ratio (OR) and 95% confidence interval (CI).
RESULTS
A total of 478 patients were assessed for PACU delirium over 1 week in three major public hospitals in Singapore. All the patients who were eligible completed their assessment. The average age was 53.9±17.2 years, with 146 patients aged > 65 years. Four in ten patients were female, and the majority had general anaesthesia. The BIS was used in 55 (11.5%) patients, and the average duration of surgery was 1.68±1.78 h. The overall incidence rate of PACU delirium was 18/478 (3.8%); the incidence rate of PACU delirium in patients aged > 65 years was 9/146 (6.2%) [Table 1].
Table 1.
Patient demographics stratified by PACU delirium.
| Variable | n (%) | P | ||
|---|---|---|---|---|
|
| ||||
| PACU delirium (n=18) | No PACU delirium (n=460) | Total (n=478) | ||
| Gender (female) | 9 (50.0) | 191 (41.6) | 200 (41.8) | 0.480 |
| Agea (yr) | 58.0 [19.1] | 53.5 [17.1] | 53.9 [17.2] | 0.277 |
| >65 | 9 (50.0) | 137 (29.8) | 146 (30.6) | 0.069 |
|
| ||||
| Chronic disease | ||||
| Hypertension | 9 (50.0) | 186 (40.5) | 195 (40.8) | 0.422 |
| Diabetes mellitus | 4 (22.2) | 88 (19.2) | 92 (19.2) | 0.748 |
| Ischaemic heart disease | 3 (16.7) | 42 (9.2) | 45 (9.4) | 0.285 |
| Chronic kidney disease | 1 (5.6) | 25 (5.4) | 26 (5.4) | 0.984 |
| Malignancy | 5 (27.8) | 12 (2.6) | 17 (3.6) | <0.001 |
|
| ||||
| Anaesthetic method | ||||
| General anaesthesia | 18 (100.0) | 396 (85.4) | 411 (86.0) | 0.572 |
| Use of BIS | 10 (55.6) | 45 (9.8) | 55 (11.5) | <0.001 |
| Duration of operationa (min) | 134.22 [72.03] | 99.22 [108.05] | 100.54 [107.06] | 0.174 |
| 0–60 | 2 (11.1) | 178 (38.8) | 180 (37.7) | |
| 60–120 | 6 (33.3) | 154 (33.6) | 160 (33.5) | |
| >120 | 10 (55.6) | 127 (27.7) | 137 (28.7) | |
|
| ||||
| Postoperative | ||||
| Length of stay in PACUa (h) | 2.72 [1.72] | 1.30 [1.09] | 1.36 [1.15] | <0.001 |
| Pain score >5 | 9 (50.0) | 202 (44.0) | 211 (44.1) | 0.606 |
| Discharged to HD/ICU | 5 (27.8) | 35 (7.6) | 40 (8.4) | 0.032 |
| Nu-DESC scorea | 4.8 [1.6] | 0.0 [0.2] | 0.2 [1.0] | <0.001 |
Mann–Whitney U test for continuous variable and chi-square test for discrete variable. aData presented as median [interquartile range]. BIS: bispectral index, HD: high dependency, ICU: intensive care unit, Nu-DESC: nursing delirium screening Scale, PACU: post-anaesthesia care unit
Logistic regression analysis [Table 2] showed that the use of BIS (P < 0.001, OR 7.50 [95% CI 2.46–24.31]) and presence of malignancy (P < 0.001, OR 10.90 [95% CI 2.57–24.31]) were significantly associated with a higher incidence of PACU delirium. Of note, age, gender, type of anaesthesia (general vs. regional), pain score in PACU and duration of surgery were not significantly associated with PACU delirium in univariate regression analysis (P > 0.05). The other prevalent chronic diseases such as hypertension, diabetes mellitus, ischaemic heart disease or chronic kidney disease also did not make a difference in the correlation with PACU delirium. Further analysis of the 55 patients who had BIS monitoring showed a median age of 60.9 (IQR 12.2) years and a higher proportion of females (51.0%) in this population. On average, they also required a longer stay in PACU postoperatively (median 1.83 [IQR 1.12] h), as compared to the general cohort.
Table 2.
Univariate and multivariate logistic/linear regression models for PACU delirium.
| Variable | Univariate | Multivariate | ||
|---|---|---|---|---|
|
|
|
|||
| P | OR (95% Cl) | P | OR (95% Cl) | |
| Gender (female) | 0.481 | 1.40 (0.54–3.65) | ||
|
| ||||
| Age>65 years | 0.0764* | 2.35 (0.90–6.14) | 0.470 | 1.47 (0.50–2.34) |
|
| ||||
| Hypertension | 0.425 | 1.47 (0.56–3.83) | ||
|
| ||||
| Diabetes mellitus | 0.748 | 1.20 (0.33–3.45) | ||
|
| ||||
| Ischaemic heart disease | 0.293 | 1.99 (0.45–6.23) | ||
|
| ||||
| Chronic kidney disease | 0.984 | 1.02 (0.06–5.30) | ||
|
| ||||
| Malignancy | <0.001* | 14.3 (4.09–45.32) | <0.001* | 10.90 (2.57–24.31) |
|
| ||||
| Use of BIS | <0.001* | 11.50 (4.33–31.58) | <0.001* | 7.50 (2.46–24.31) |
|
| ||||
| Duration of surgery (min) | ||||
| 60–120 | 0.131 | 3.46 (0.78–23.9) | 0.395 | 2.12 (0.41– |
| >120 | 0.0129* | 7.00 (1.81–46.1) | 15.73) | |
|
| ||||
| Pain score>5 in PACU | 0.616 | 1.27 (0.49–3.32) | ||
|
| ||||
| Discharge destination (HD/ICU) | 0.006* | 4.52 (1.39–12.74) | 0.440 | 1.35 (0.32–4.69) |
Factors that had a P value of <0.10 from the univariate analysis were included in the multivariate analysis. *Statistically significant. BIS: bispectral index, CI: confidence interval, HD: high dependency, ICU: intensive care unit, Nu-DESC: nursing delirium screening scale, OR: odds ratio, PACU: post-anaesthesia care unit
DISCUSSION
In this cross-sectional, observational study of patients undergoing non-cardiac surgeries in three major public hospitals in Singapore, the incidence of PACU delirium was found to be 3.8%, increasing to 6.2% in those older than 65 years. Our study reported a low incidence of 3.8%, which could reflect the relatively young age of the postoperative population that was assessed within the time frame across different hospital systems. In comparison, in other studies involving elderly orthopaedic trauma patients, up to 50% of patients have been reported to develop PACU delirium.[4,5]
The Nu-DESC is a validated tool for diagnosing delirium postoperatively. We found the implementation of Nu-DESC as a screening tool to be simple, effective and non-disruptive to the workflow in PACU.[2,6,7] A Swiss study that also used Nu-DESC reported an incidence of 4.8%, similar to our experience.[3] However, compared to the Swiss study, the patients in our cohort were younger (58.0 vs 72.9 years) and had an average longer duration of surgery (134.2 vs 85.6 min). With increasing age, the risk of PACU delirium increases. Similar to other studies, we reported a twofold increase in its incidence in postoperative patients aged over 65 years. The type of anaesthesia did not make a difference in our population, and this may be due to the relatively short duration of surgery in this observational study.
An interesting finding was that the use of BIS was associated with a higher incidence of PACU delirium. However, the relationship is unlikely to be causal in nature; BIS was more frequently used in patients aged above 65 years and this reflects the notion that local anaesthesiologists regarded age as a possible indication for using BIS. Bispectral index-guided anaesthesia has been shown to reduce the rates of POD,[10,11] particularly in the elderly. Although it is more common for local anaesthesiologists to utilise BIS for older patients, there was no evidence that this prevented PACU delirium. Also, we did not have data on whether BIS was used to guide the depth of anaesthesia.
Patients with malignancy were at-risk for developing PACU delirium. They were also more likely to utilise more resources and high-dependency unit (HDU) or intensive care unit (ICU) care. This could reflect the patients’ premorbid condition, more extensive surgery and stress response. Increasingly, the role of chemotherapy and the ‘chemo fog’ that is reported may also predispose this vulnerable patient group to PACU delirium.[12] Further data would be required to identify areas of intervention and prevention.
PACU delirium is a harbinger for POD,[13] and early detection and effective triage of these patients is crucial. Patients with PACU delirium and higher Nu-DESC scores were more likely to require more extensive resources and discharge from PACU to HDU or ICU. Implementing Nu-DESC in the PACU unit will lay the foundation for using it as a standard of care and optimising resource management for patients in the postoperative period.
This was the first local observational study of PACU delirium that involved three major public institutions in Singapore. Even though the audit was performed over a relatively short time frame, this study has affirmed the importance of PACU delirium, particularly with an increasingly ageing population presenting for surgery. Specifically, we identified patients with malignancy as a vulnerable group. Future studies will be designed to understand the role of the disease and treatment in PACU delirium. Understanding these risk factors will form the basis for which protocols can be established to optimise resource management and prevent long-term morbidities and mortality of PACU delirium.
This study was not without limitations. All associations are observations, and may indicate, but do not prove, causations. The history of patients with dementia or cognitive impairment, which had been strongly linked with POD, was not collated due to the predominantly young age of the study cohort.
In conclusion, in this 1-week observational study of 478 patients undergoing non-cardiac surgery in Singapore, we found a low incidence of PACU delirium (overall 3.8%, aged >65 years 6.2%). Positive correlation included a history of malignancy and the use of BIS. In addition, PACU delirium was associated with a longer duration of PACU stay.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
About the first author

Dr Ke Yuhe is an anaesthesia resident under the SingHealth Anaesthesiology Residency Programme. She graduated from National University of Singapore in 2017 and was awarded the NUHS Department of Anaesthesia Prize. She has interest in perioperative medicine and big data research in health care.
Acknowledgement
We thank Ms Celest Goh for helping with the data collection at National University Hospital and Dr Felicia Tan for helping with the data collection and entry at Khoo Teck Puat Hospital.
REFERENCES
- 1.Radtke FM, Franck M, MacGuill M, Seeling M, Lütz A, Westhoff S, et al. Duration of fluid fasting and choice of analgesic are modifiable factors for early postoperative delirium. Eur J Anaesthesiol. 2010;27:411–6. doi: 10.1097/EJA.0b013e3283335cee. [DOI] [PubMed] [Google Scholar]
- 2.Radtke FM, Franck M, Schust S, Boehme L, Pascher A, Bail HJ, et al. A comparison of three scores to screen for delirium on the surgical ward. World J Surg. 2010;34:487–94. doi: 10.1007/s00268-009-0376-9. [DOI] [PubMed] [Google Scholar]
- 3.Winter A, Steurer MP, Dullenkopf A. Postoperative delirium assessed by post anesthesia care unit staff utilizing the Nursing Delirium Screening Scale: A prospective observational study of 1000 patients in a single Swiss institution. BMC Anesthesiol. 2015;15:184. doi: 10.1186/s12871-015-0168-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sciard D, Cattano D, Hussain M, Rosenstein A. Perioperative management of proximal hip fractures in the elderly: The surgeon and the anesthesiologist. Minerva Anestesiol. 2011;77:715–22. [PubMed] [Google Scholar]
- 5.Sharma PT, Sieber FE, Zakriya KJ, Pauldine RW, Gerold KB, Hang J, et al. Recovery room delirium predicts postoperative delirium after hip-fracture repair. Anesth Analg. 2005;101:1215–20. doi: 10.1213/01.ane.0000167383.44984.e5. [DOI] [PubMed] [Google Scholar]
- 6.Radtke FM, Franck M, Schneider M, Luetz A, Seeling M, Heinz A, et al. Comparison of three scores to screen for delirium in the recovery room. Br J Anaesth. 2008;101:338–43. doi: 10.1093/bja/aen193. [DOI] [PubMed] [Google Scholar]
- 7.Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA. Fast, systematic, and continuous delirium assessment in hospitalized patients: The nursing delirium screening scale. J Pain Symptom Manage. 2005;29:368–75. doi: 10.1016/j.jpainsymman.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 8.Mahanna-Gabrielli E, Schenning KJ, Eriksson LI, Browndyke JN, Wright CB, Culley DJ, et al. State of the clinical science of perioperative brain health: Report from the American Society of Anesthesiologists Brain Health Initiative Summit 2018. Br J Anaesth. 2019;123:464–78. doi: 10.1016/j.bja.2019.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Aldecoa C, Bettelli G, Bilotta F, Sanders RD, Audisio R, Borozdina A, et al. European Society of Anaesthesiology evidence-based and consensus-based guideline on postoperative delirium. Eur J Anaesthesiol. 2017;34:192–214. doi: 10.1097/EJA.0000000000000594. [DOI] [PubMed] [Google Scholar]
- 10.Janssen TL, Alberts AR, Hooft L, Mattace-Raso F, Mosk CA, van der Laan L, et al. Prevention of postoperative delirium in elderly patients planned for elective surgery: Systematic review and meta-analysis. Clin Interv Aging. 2019;14:1095–117. doi: 10.2147/CIA.S201323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan MTV, Cheng BCP, Lee TMC, Gin T CODA Trial Group. BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol. 2013;25:33–42. doi: 10.1097/ANA.0b013e3182712fba. [DOI] [PubMed] [Google Scholar]
- 12.Mandilaras V, Wan-Chow-Wah D, Monette J, Gaba F, Monette M, Alfonso L, et al. The impact of cancer therapy on cognition in the elderly. Front Pharmacol. 2013;4:48. doi: 10.3389/fphar.2013.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hesse S, Kreuzer M, Hight D, Gaskell A, Devari P, Singh D, et al. Association of electroencephalogram trajectories during emergence from anaesthesia with delirium in the postanaesthesia care unit: An early sign of postoperative complications. Br J Anaesth. 2019;122:622–34. doi: 10.1016/j.bja.2018.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]


