Abstract
Background
The annual volume of patients requiring revision total hip arthroplasty prior to age 60 is projected to increase considerably. Despite this, outcome data for revision THA in these younger patients remain limited. The purpose of this study was to define implant survivorship, identify risk factors for re-revision, and determine clinical outcomes of revision THA in patients aged ≤60 years.
Methods
We identified 191 revision THAs performed in patients aged ≤60 years. Minimum 4-year follow-up was obtained in 141 (73.8%) hips (mean 10.3 years [range, 4–20]). Mean age was 48 years (range, 20–60). Forty-five hips (32%) had previously been revised. Indications for index revision included aseptic loosening (28%), polyethylene wear (26%), dislocation (20%), and infection (14%). Outcome measures were Kaplan-Meier survival free from re-revision and patient-reported outcome scores (mHHS, UCLA).
Results
Survivorship free from re-revision for any cause was 78% [95% CI=70–85] at five years and 71% [62–78] at ten years. The most common indication for re-revision at both five and ten years was dislocation (12% [8–19], 16% [10–23]), followed by infection (6% [3–12], 10% [5–18]) and aseptic loosening (2% [1–7], 4% [1–11]). Mean scores were improved from baseline at six (mHHS +21.4, UCLA +0.9) and twelve years (mHHS +13.4, UCLA +0.5).
Conclusion
Revision THA in patients less than 60 years of age was associated with considerably lower rates of early loosening-related failure than historically reported. Recurrent dislocation and infection appear to remain challenges in this population. Despite improvements in survivorship from earlier studies, patient-reported functional improvements remained relatively unchanged.
Level of Evidence: IV
Keywords: revision, hip, arthroplasty, THA, young, younger
Introduction
Younger age at the time of primary total hip arthroplasty (THA) has historically been associated with increased risk for revision surgery.1-3 With contemporary implants and surgical technique, revision-free survivorship of primary THA in younger patients has approached that of older patients,4 and THA continues to be utilized increasingly in younger patients.5
With more than half of all primary THAs projected to be performed in patients <65 by the end of the decade, and with the greatest increase expected among patients aged 45–55, the volume of patients that can be anticipated to require revision surgery prior to age 60 is considerable.5-8 Understanding the indications and prognoses of revision surgery in this population is critical to providing realistic expectations to these patients and to mitigating risk for re-revision surgery.
Despite this importance, outcome data for revision THA in young patients have remained extremely limited. Ten-year failure rates have ranged from 37–52%, with high observed rates of early aseptic loosening.9-11 However, the majority of series published to date include more historical fixation (cemented, early cementless) and bearing surfaces (conventional polyethylene, early ceramics). Thus, the purpose of this study was to provide a more contemporary overview of implant survivorship, risk factors for re-revision, and clinical outcomes of revision THA in patients 60 years of age or younger.
Methods
Following institutional review board approval, a retrospective review of our institutional total joint arthroplasty registry was performed to identify patients who underwent revision THA at 60 years of age or younger between 2000 and 2016. Revision THA was defined as reoperation with exchange of one or more components of a prior THA. Patients with prior hemi- or resurfacing arthroplasty were excluded. Oncologic cases were also excluded. We initially identified 191 revision THAs. Of these, 141 (73.8%) had minimum 4-year follow-up (mean 10 years [range, 4–20 years]) or were re-revised and were the focus of this report.
Mean age at the time of index revision THA was 48 years (range, 20–60), mean body mass index (BMI) was 29 (range, 19–53 kg/m2), and 65% were female. Prior ipsilateral revision THA was noted in 45 (32%) hips (mean 1.7 previous revisions [range, 1–6]). The most common indications for index revision surgery were aseptic loosening (28%), polyethylene wear (26%), dislocation (20%), and periprosthetic joint infection (PJI) (14%). Aseptic loosening was of the acetabular component in 26 (67%) hips, femoral component in 3 (8%) hips, and of both components in 10 (26%) hips. Comorbidities included rheumatoid arthritis (13%), systemic lupus erythematous (12%), sickle cell anemia (1%), and HIV/AIDS (1%).
Among the 141 included revision surgeries, acetabular revisions were most common (43%, n=61), followed by femoral and acetabular revision (25%, n=35), isolated head and liner exchange (24%, n=34), and femoral revision (8%, n=11), Table 1. Both head and liner were exchanged in all cases. Heads were predominantly cobalt chromium (93%, n=121), with ceramic used in the remainder (7%, n=20). Median head size was 32mm (range, 22–40) and 86% of polyethylene liners were highly cross-linked. Constrained liners were used in 39% (n=11/28) of hips undergoing index revision for dislocation. A posterolateral approach was used in all cases. Postoperatively, all patients were instructed to follow posterior hip precautions for three months, and abduction bracing used selectively.
Table 1.
Components Used in the 141 Included Revision THAs
| Components | % used |
|---|---|
| Acetabular | |
| Zimmer Trabecular Metal ModularTM | 68% |
| Zimmer Trilogy® | 30% |
| Howmedica Osteonics | 2% |
| Femoral | |
| Zimmer VerSys® Beaded Fullcoat | 72% |
| DePuy Solution System® | 14% |
| Zimmer VerSys® Heritage® | 7% |
| Howmedica Osteonics | 2% |
| Stryker GMRSTM Global Modular Replacement System | 2% |
| Smith & Nephew SpectronTM | 2% |
Clinical follow-up was recommended at 6 weeks, 6 months, 1 year, 2 years, 5 years, 10 years, and 15 years. Patients with less than 4-year clinical follow-up were contacted by phone or mail for updates on their clinical status. Follow-up was completed predominantly in person (81%). Correspondence by phone or mail was used to obtain follow-up in 19% of patients.
All intra- and post-operative complications were recorded, as well as all reoperations and re-revisions. Re-revision was the primary study endpoint and was defined as exchange of one or more components and/ or open reduction and internal fixation of the femur or acetabulum. Survivorship free from re-revision was calculated at 5 years and 10 years using Kaplan-Meier survivorship estimation.12 Failure rates at 5- and 10-year were reported as the difference between 1 and the Kaplan-Meier survival estimate.
Clinical outcomes were assessed through patient-reported outcome scores gathered preoperatively, at minimum 4-year follow-up, and at latest follow-up. These included the modified Harris Hip- (mHHS)13 and UCLA Activity14 scores. Scores in patients who underwent index revision for infection were not included in our report or analysis of scores.
Statistical Analysis
Statistical analysis was performed to assess patient factor differences (age, sex, BMI, comorbidities, prior revision history, bone defect, femoral head size, bearing material) between surviving hips and those that were re-revised (for any reason, and for each of the most common re-revision indications). Categorical variables were compared using Chi-square tests and continuous variables with two-tailed t tests. A p value less than 0.05 defined significance.
Results
At 10-year mean follow-up (range, 4–20), forty hips (27.8%) had been re-revised. Indications for re-revision included dislocation (13.5%, n=19), PJI (7.8%, n=11), aseptic loosening of the acetabular (2.8%, n=4) or femoral (0.7%, n=1) component, periprosthetic femur fracture (1.4%, n=2), component failure (1.4%, n=2), and polyethylene wear (0.7%, n=1). The two component failures included a fractured femoral stem, and a fractured constrained liner secondary to a fall. As such, the 10-year survivorship free of re-revision for any cause was 78% at 5 years (95% Confidence Interval [CI]=70%–85%) and 71% at 10 years (95% CI=62%–78%). When excluding index revisions performed for PJI, survivorship free of re-revision was 80% at 5 years (95% CI=72%–86%) and 73% at 10 years (95% CI=64%–80%).
The greatest overall contributor to failure at both five and ten years was dislocation (12% [95% CI=8–19%], 16% [95% CI=10–23%]), followed by PJI (6% [95% CI=3–12%], 10% [95% CI=5–18%]) and aseptic loosening (2% [95% CI=1–7%], 4% [95% CI=1–11%]), Table 2.
Table 2.
Reasons for Re-Revision
| Failure in Overall Cohort | ||
|---|---|---|
| 5-year Failure | 10-year Failure | |
| % [95% CI] | % [95% CI] | |
| Full Cohort | ||
| Any Reason | 22.3 [14.8-30.2] | 29.3 [22.1-38.1] |
| Loosening | 2.4 [0.8-7.4] | 3.9 [1.4-10.5] |
| Instability | 12.1 [7.6-19.1] | 15.5 [10.0-23.4] |
| Infection | 6.0 [3.0-11.7] | 9.7 [5.4-17.8] |
| Excluding Index Indication: Infection) | ||
| Any Reason | 20.1 [13.9-28.5] | 27.0 [19.6-36.5] |
| Loosening | 2.8 [0.9-8.5] | 4.5 [1.6-12.1] |
| Instability | 11.3 [6.7-18.7] | 15.1 [9.5-23.7] |
| Infection | 5.2 [2.4-11.2] | 7.8 [3.9-15.2] |
| Failure by Index Revision Indication | ||
| Wear +/- Osteolysis | ||
| Any Reason | 8.1 [2.7-23.1] | 8.1 [2.7-23.1] |
| Loosening | 5.4 [1.4-19.9] | 5.4 [1.4-19.9] |
| Instability | 2.8 [0.4-18.1] | 2.8 [0.4-18.1] |
| Infection | - | - |
| Loosening | ||
| Any Reason | 8.5 [2.8-24.1] | 12.5 [4.8-30.4] |
| Loosening | 3.1 [0.4-20.2] | 3.1 [0.4-20.2] |
| Instability | - | 4.3 [0.6-27.1] |
| Infection | 5.6 [1.4-20.4] | 5.6 [1.4-20.4] |
| Instability | ||
| Any Reason | 54.3 [37.6-69.3] | 74.3 [56.9-88.9] |
| Loosening | - | 14.3 [2.1-66.6] |
| Instability | 40.8 [24.6-62.4] | 52.5 [33.4-74.5] |
| Infection | 10.0 [3.3-27.9] | 25.7 [10.5-55.0] |
| Infection | ||
| Any Reason | 35.0 [18.5-59.7] | 42.2 [23.4-67.7] |
| Loosening | - | - |
| Instability | 10.8 [2.8-36.9] | 17.2 [5.8-44.6] |
| Infection | 10.8 [2.8-36.9] | 20.7 [10.6-54.0] |
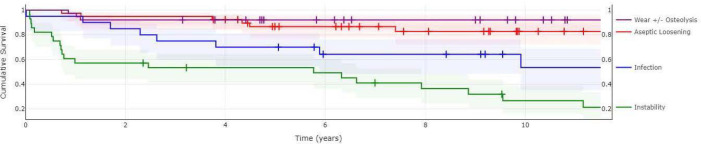
Survivorship free from re-revision differed considerably by index revision indication and was greater for indications of wear/osteolysis (92% at 10 years [95% CI=77–97%]) and aseptic loosening (88% [95% CI=70– 95%]) compared to dislocation (26% [95% CI=11–43%]) and PJI (58% [95% CI=32–77]), Figure 1.
Figure 1.
Survivorship by index revision indication (80% confidence intervals).
There were eight (6%) complications that did not require re-revision. These included: four dislocations that were closed reduced with no sequelae thereafter, two hematomas treated with I&D, one superficial infection treated with I&D, and one DVT. All other complications were those resulting in re-revision.
Factors Associated with Re-revision
Prior ipsilateral revision surgery was found to be a significant risk factor for re-revision (Relative Risk [RR] 2.65 [95% CI=1.56–4.50], p<0.005). Hips with at least one prior revision for dislocation were considerably more likely to undergo re-revision for dislocation (RR 5.41 [95% CI=2.57–11.41], p<0.001), and hips with at least one prior revision for PJI were more likely to undergo re-revision for PJI (RR 4.33 [95% CI=1.32–14.17], p=0.016). Female sex was associated with elevated risk for re-revision for dislocation (RR 3.44 [95% CI=1.06–11.20], p=0.040). There were no associations between failure (for any reason, or for any specific reason) and age, BMI, comorbidities, femoral head size, or presence or absence of an acetabular or femoral defect for which bone graft was used, Table 3.
Table 3.
Risks Factors for Re-revision
| Risk Factors for Re-revision | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Re-Revision for: | Any Cause n=40 | Loosening n=5 | Instability n=19 | Infection n=11 | |||||
| Nonrevised | Revised | p= | Revised | p= | Revised | p= | Revised | p= | |
| Age | |||||||||
| Average | 48.6 | 48.0 | 0.691 | 44.2 | 0.276 | 48.6 | 0.994 | 48.1 | 0.520 |
| >40 | 81% | 85% | 0.593 | 80% | 0.380 | 84% | 0.047 | 73% | 0.425 |
| <50 | 47% | 50% | 0.365 | 20% | 0.245 | 63% | 0.184 | 45% | 0.946 |
| Sex | |||||||||
| Female | 60% | 80% | 0.026 | 80% | 0.380 | 84% | 0.047 | 73% | 0.425 |
| BMI | |||||||||
| Average | 29.4 | 29.2 | 0.851 | 27.1 | 0.454 | 29.4 | 0.728 | 28.5 | 0.704 |
| >30 | 41% | 33% | 0.437 | 20% | 0.344 | 40% | 0.924 | 33% | 0.700 |
| Comorbities | |||||||||
| Any | 30% | 23% | 0.389 | 20% | 06.42 | 26% | 0.766 | 18% | 0.422 |
| Rheumatoid Arthritis | 15% | 10% | 0.447 | - | - | 10% | 0.620 | 18% | 0.770 |
| Lupus | 12% | 13% | 0.920 | 20% | 0.589 | 16% | 0.637 | - | - |
| Prior Ipsi. Revision | |||||||||
| Any | 27% | 60% | <0.005 | 40% | 0.516 | 68% | <0.005 | 82% | <0.005 |
| Instability | 2% | 23% | <0.001 | 20% | 0.018 | 42% | <0.001 | 18% | 0.013 |
| Infection | 4% | 15% | 0.021 | 20% | 0.099 | 11% | 0.228 | 27% | <0.001 |
| Bone Deficiency | |||||||||
| Acetabular | 29% | 20% | 0.289 | 50% | 0.368 | 16% | 0.234 | 27% | 0.904 |
| Femoral | 11% | 8% | 0.544 | - | - | 5% | 0.453 | 9% | 0.854 |
| Femoral Head Size (mm) | |||||||||
| Median | 32 | 32 | - | 32 | - | 32 | - | 32 | - |
| Mean | 32.3 | 31.8 | 0.225 | 32.6 | 0.857 | 32.5 | 0.658 | 32.2 | 0.708 |
| <32 | 21% | 35% | 0.078 | 20% | 0.966 | 37% | 0.129 | 27% | 0.619 |
| Polyethylene Liner* | |||||||||
| Conventional | 12% | 23% | 0.137 | 20% | 0.568 | 29% | 0.086 | - | - |
| Highly Crosslinked | 88% | 77% | 80% | 71% | 100% | ||||
*Constrained liners excluded.
Index Revision Indication: Dislocation
Among the 28 patients who underwent index revision for dislocation, 20 (71%) were re-revised at a mean of 3 years (median 0.75) for dislocation (39.3% [58% of all re-revisions for dislocation]), PJI (17.9%), and aseptic loosening (7.1%). Though head diameter was not associated with failure in the overall cohort, hips that underwent index revision for dislocation that were re-revised for dislocation had smaller head diameters than those that survived (median 28mm vs 34mm, p=0.016). All non-revised hips in this group had a head size ≥32mm, while 55% of those re-revised for dislocation had a head size <32mm (p=0.012). Rates of re-revision for dislocation were similar between those with and without a constrained liner (36% vs. 41%, p=0.799), though those that received a constrained liner had more commonly failed previous revision surgery. No other factors, including age (49±8 vs 48±9, p=0.915) or BMI (30.1±8 vs 29.3±7, p=0.653), were associated with elevated risk of re-revision for recurrent dislocation within this group.
Function
Among surviving hips, mean mHHS improved from 49.7 preoperatively to 71.1 at 6 years (n=66, range, 24–100) and 63.1 at 12 years (n=66, range, 15–100). At these same intervals, UCLA Activity scores had improved from 4.1 preoperatively to 5.0 (n=66, range, 2–10) and 4.6 (n=66, range, 2–10), Table 4.
Table 4.
PRO Scores
| PRO Clinical Status Changes (Full Cohort) | |||
|---|---|---|---|
| Preoperative | 6 Years | 12 Years | |
| mHHS | 49.7 | 71.1 | 63.1 |
| Score >70 | 13% | 60% | 40% |
| Score >80 | 5% | 43% | 26% |
| Improvement >20 | - | 50% | 34% |
| Improvement Score >70 OR >20 | - | 71% | 48% |
| UCLA | 4.1 | 5.0 | 4.6 |
| >5 | 39% | 49% | 27% |
| 8-10 | 7% | 19% | 19% |
Score improvements and final scores were comparable between index indication groups. Groups were similar with respect to age, sex, years between primary THA and index revision, and revision history, Table 5.
Table 5.
PRO Scores and Patient Characteristics by Index Revision Indication Group
| Patient-Reported Outcome Scores and Patient Characteristics by Index Revision Indication Group | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mHHS | UCLA | |||||||||||
| Baseline | 6 Years | 12 Years | Baseline | 6 Years | 12 Years | n hips (% of survivors) | Mean age at surgery | %F | Years from THA Mean (SD) | Prior Revision | n (mean) | |
| All | 49.7 | 71.1 | 63.1 | 4.1 | 5.0 | 4.6 | 66 (72%) | 49 | 65% | 11.3 (8) | 23% | 1.4 |
| Loosening | 45.0 | 70.8 | 69.6 | 3.9 | 4.9 | 4.5 | 27 (79%) | 47 | 62% | 10.9 (8) | 26% | 1.7 |
| Wear | 52.8 | 70.4 | 64.8 | 4.7 | 5.5 | 5.1 | 25 (73%) | 50 | 65% | 13.6 (7) | 17% | 1.5 |
| Instability | 28.9 | 56.4 | 48.4 | 3.0 | 4.0 | 3.0 | 6 (75%) | 50 | 50% | 11.9 (12) | 50% | 1.0 |
Discussion
As the volume of younger patients undergoing THA continues to increase,5-7 the importance of understanding the indications and prognoses of revision surgery in this population has grown considerably.8 Despite this importance, published outcome data has remained largely limited to surgeries performed prior to the wide adoption of more durable fixation techniques and bearings, Table 6.
Table 6.
Studies Reporting 10-Year Survivorship of Revision THA in Younger Patients
| Study Year | Age (mean) [rng] | Surgery Dates | n hips | Follow-up (years) | Survivorship free from re-revision for: | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Min. | (mean) | [range] | Any Cause | Aseptic Loosening | |||||||
| 5 year | 10 year | 5 year | 10 year | ||||||||
| Stromberg | 1994 | <55 (47) [31-55] | 1979-1982 | 59 | 8 | (10) | [8-13] | - | - | 86% | 48% |
| Stromberg | 1996 | <55 (47) [29-55] | 1984-1986 | 70 | 4 | (7) | [4-10] | - | - | - | 76% |
| Lee | 2013 | <50 (43) [22-50] | 1983-2008 | 151 | 2 | (11) | [2-26] | - | 63% | - | 74%* |
| Kuijpers | 2020 | <55 (49) [18-54] | 2007-2018 | 1037 | 0.1 | (4) | [0.1-12] | 78% [75-81] | 72% [67-76] | 95% [92-96] | 90% [85-94] |
| Present Study | 2022 | <60 (48) [20-60] | 2000-2016 | 141 | 4 | (10) | [4-20] | 78% [70-85] | 70% [62-78] | 98% [93-99] | 96% [90-99] |
*Approximated (70% failures due to aseptic loosening).
Survivorship data presented as % [95% CI].
In our series, re-revision free survivorship was 80% and 73% at 5 and 10 years, which is notably higher than rates previously reported. At 10-year mean follow-up, Stromberg et al. reported on 59 revision THAs performed for aseptic loosening in patients less than 55 years of age years with a first-generation cementing technique. Survivorship free from re-revision for aseptic loosening was 86% at four years and 48% at ten years (acetabular 65%, femoral 61%).9 In a similar cohort of 70 hips, the same authors reported this rate to be 76% at eight years with a second-generation cementing technique (acetabular 80%, femoral 85%).10 At 11-year mean follow-up, Lee et al. reported on 151 revision THAs performed primarily for aseptic loosening (86%) in patients less than 50 years of age with cementless components. Survivorship was 88% at five years and 63% at ten years (acetabular 71%, femoral 80%), with failures again due primarily to aseptic loosening (70% of failures).11 In contrast, we observed considerably lower rates of failure due to aseptic loosening, with only a 4% failure rate due to aseptic loosening at 10 years.
Our results are comparable to those of one of the only studies to evaluate similarly modern revision THA outcomes in this younger population. Kuijpers et al. reported outcomes of 1,037 revision THAs in the Dutch Arthroplasty Register in patients less than 55 years of age for index indications aseptic loosening (32%), dislocation (20%), infection (16%), and cup/liner wear (4%). They reported re-revision-free survivorship rates of 78% and 72% at five and ten years. Five- and ten-year failure due to aseptic loosening was 5% (acetabular 3.1%, femoral 2.3%) and 10% (7.0%, 2.7%).15
Owing to these lower rates of early loosening-related failure, re-revision-free survivorship in the current study and the study of Kuijpers et al. was considerably higher than rates previously reported in this younger population, and compared favorably to rates reported in general revision THA populations at both five (81–83%)16-17 and ten (72%)18 years. Overall 10-year failure rates for both instability (16%) and infection (10%), were comparable to rates reported in general revision THA populations at similar intervals (dislocation 1–27%, infection 1–22%).19-22
To our knowledge, the current study is the first to report clinical outcome scores in a large contemporary series of revision THAs in this younger population. Despite improvements in survivorship from earlier studies, patients reported similarly modest23-25 improvements in outcome scores at 6 years (mHHS +21.4, UCLA +0.9) and 12 years (mHHS +13.4, UCLA +0.5). In contrast, a 2003 meta-analysis of revision THA outcomes in the general population (mean age 67), noted a mean mHHS improvement of 37.3 [95% CI 34.7–39.9] at 5-year mean follow-up.26 This lag of scores behind survivorship improvements over time was similarly observed by a meta-analysis of primary THA outcomes in patients less than 30 years of age, where it was suggested to be due to the higher incidence of systemic disease in very young patients undergoing THA. Our similar finding in this broader age range (<60) of younger patients may highlight the significance of an independent effect of higher demands or expectations in younger populations in limiting felt improvements. We did not observe a significant relationship between age and reported score improvement within this cohort. Incidence of previously studied comorbidities were low and these were not found to be significantly associated with either re-revision rates or score improvements.
There are several limitations to this study. First, THA surgery is continuously evolving, and it is possible that outcomes of today’s revision surgeries differ meaningfully from those reported by this study. However, in a recent report on revision THAs performed between 2010 and 2016 in a cohort similar to the current study’s, re-revision-free survivorship at 5 years (81% [95% CI 76–86%]) was similar to that in the current study (80% [95% CI 72– 86%]), and instability was similarly the leading indication for re-revision (44%) in that study (5-year instability-related failure rate of 8%, vs. 11% in the current study).27 Second, this patient population was treated at a high-volume tertiary care center and may represent comparatively more severe revision cases than the average young patient undergoing revision THA. Third, radiographic data may have allowed for detection of more subtle outcome differences and risk factors for re-revision. Finally, a larger cohort may have permitted multivariate determination of risk factors for re-revision, which would have been valuable given the number of potentially influential factors and the complexity of their relationships with one another.
Conclusion
Revision THA in patients less than 60 years of age was associated with considerably lower rates of early loosening-related failure than historically reported. Recurrent dislocation and infection appear to remain challenges in this population for which an improved understanding of risk factors and mitigation strategies would be of benefit. Despite improvements in survivorship from earlier studies, patient-reported functional improvements remained relatively unchanged.
References
- 1.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–85. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 2.Santaguida PL, Hawker GA, Hudak PL, Glazier R, Mahomed NN, Kreder HJ, Coyte PC, Wright JG. Patient characteristics affecting the prognosis of total hip and knee joint arthroplasty: a systematic review. Can J Surg. 2008;51(6):428–36. [PMC free article] [PubMed] [Google Scholar]
- 3.Wainwright C, Theis JC, Garneti N, Melloh M. Age at hip or knee joint replacement surgery predicts likelihood of revision surgery. J Bone Joint Surg Br. 2011;93(10):1411–5. doi: 10.1302/0301-620X.93B10.27100. [DOI] [PubMed] [Google Scholar]
- 4.Mei XY, Gong YJ, Safir O, Gross A, Kuzyk P. Long-term outcomes of total hip arthroplasty in patients younger than 55 years: a systematic review of the contemporary literature. Can J Surg. 2019;62(4):249–258. doi: 10.1503/cjs.013118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwartz AM, Farley KX, Guild GN, Bradbury TL., Jr. Projections and Epidemiology of Revision Hip and Knee Arthroplasty in the United States to 2030. J Arthroplasty. 2020;35(6S):S79–S85. doi: 10.1016/j.arth.2020.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Singh JA, Vessely MB, Harmsen WS, Schleck CD, Melton LJ, 3rd, Kurland RL, Berry DJ. A population-based study of trends in the use of total hip and total knee arthroplasty, 1969-2008. Mayo Clin Proc. 2010;85(10):898–904. doi: 10.4065/mcp.2010.0115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skyttä ET, Jarkko L, Antti E, Huhtala H, Ville R. Increasing incidence of hip arthroplasty for primary osteoarthritis in 30- to 59-year-old patients. Acta Orthop. 2011;82(1):1–5. doi: 10.3109/17453674.2010.548029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strömberg CN, Herberts P. A multicenter 10-year study of cemented revision total hip arthroplasty in patients younger than 55 years old. A follow-up report. J Arthroplasty. 1994;9(6):595–601. doi: 10.1016/0883-5403(94)90112-0. [DOI] [PubMed] [Google Scholar]
- 10.Strömberg CN, Herberts P. Cemented revision total hip arthroplasties in patients younger than 55 years old. A multicenter evaluation of second-generation cementing technique. J Arthroplasty. 1996;11(5):48999. doi: 10.1016/s0883-5403(96)80099-4. [DOI] [PubMed] [Google Scholar]
- 11.Lee PT, Lakstein DL, Lozano B, Safir O, Back-stein J, Gross AE. Mid-to long-term results of revision total hip replacement in patients aged 50 years or younger. Bone Joint J. 2014;96-B(8):1047–51. doi: 10.1302/0301-620X.96B8.31587. PMID: 25086120. [DOI] [PubMed] [Google Scholar]
- 12.Kaplan EL, Meier P. Nonparametric Estimation from Incomplete Observations. J American Statistical Association. 1958;53(282):457–81. [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An endresult study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 14.Amstutz HC, Thomas BJ, Jinnah R, et al. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–41. [PubMed] [Google Scholar]
- 15.Kuijpers MFL, Hannink G, van Steenbergen LN, Schreurs BW. Outcome of revision hip arthroplasty in patients younger than 55 years: an analysis of 1,037 revisions in the Dutch Arthroplasty Register. Acta Orthop. 2020;91(2):165–70. doi: 10.1080/17453674.2019.1708655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ong KL, Lau E, Suggs J, Kurtz SM, Manley MT. Risk of subsequent revision after primary and revision total joint arthroplasty. Clin Orthop Relat Res. 2010;468(11):3070–3076. doi: 10.1007/s11999-010-1399-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J. Revision hip arthroplasty: infection is the most common cause of failure. Clin Orthop Relat Res. 2010;468(8):2046–2051. doi: 10.1007/s11999-010-1251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lie SA, Havelin LI, Furnes ON, Engesaeter LB, Vollset SE. Failure rates for 4762 revision total hip arthroplasties in the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2004;86(4):504–9. PMID: 15174543. [PubMed] [Google Scholar]
- 19.Mahomed NN, Barrett JA, Katz JN, Phillips CB, Losina E, Lew RA, Guadagnoli E, Harris WH, Poss R, Baron JA. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85(1):27–32. doi: 10.2106/00004623-200301000-00005. PMID: 12533568. [DOI] [PubMed] [Google Scholar]
- 20.Zhan C, Kaczmarek R, Loyo-Berrios N, Sangl J, Bright RA. Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am. 2007;89(3):526–33. doi: 10.2106/JBJS.F.00952. PMID: 17332101. [DOI] [PubMed] [Google Scholar]
- 21.Blom AW, Taylor AH, Pattison G, Whitehouse S, Bannister GC. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg Br. 2003;85(7):956–9. doi: 10.1302/0301-620x.85b7.14095. PMID: 14516026. [DOI] [PubMed] [Google Scholar]
- 22.Garvin KL, Hanssen AD. Infection after total hip arthroplasty. Past, present, and future. J Bone Joint Surg Am. 1995;77(10):1576–88. doi: 10.2106/00004623-199510000-00015. PMID: 7593069. [DOI] [PubMed] [Google Scholar]
- 23.Strömberg CN, Herberts P, Ahnfelt L. Revision total hip arthroplasty in patients younger than 55 years old. Clinical and radiologic results after 4 years. J Arthroplasty. 1988;3(1):47–59. doi: 10.1016/s0883-5403(88)80052-4. PMID: 3361320. [DOI] [PubMed] [Google Scholar]
- 24.Espehaug B, Havelin LI, Engesaeter LB, Langeland N, Vollset SE. Patient satisfaction and function after primary and revision total hip replacement. Clin Orthop Relat Res. 1998;(351):135–48. PMID: 9646756. [PubMed] [Google Scholar]
- 25.Lübbeke A, Katz JN, Perneger TV, Hoffmeyer P. Primary and revision hip arthroplasty: 5-year outcomes and influence of age and comorbidity. J Rheumatol. 2007;34(2):394–400. PMID: 17143967. [PubMed] [Google Scholar]
- 26.Saleh KJ, Celebrezze M, Kassim R, Dykes DC, Gioe TJ, Callaghan JJ, Salvati EA. Functional outcome after revision hip arthroplasty: a metaanalysis. Clin Orthop Relat Res. 2003;416:254–64. doi: 10.1097/01.blo.0000093006.90435.43. PMID: 14646768. [DOI] [PubMed] [Google Scholar]
- 27.Sarpong NO, Kaidi AC, Syku M, Mensah C, Blevins JL, Chalmers BP. Survivorship and Risk Factors for Re-Revision after Aseptic Revision Total Hip Arthroplasty in Patients Aged ≤55 Years [published online ahead of print, 2022 Mar 19]. J Arthroplasty. 2022. S0883-5403(22)00342-4. [DOI] [PubMed]