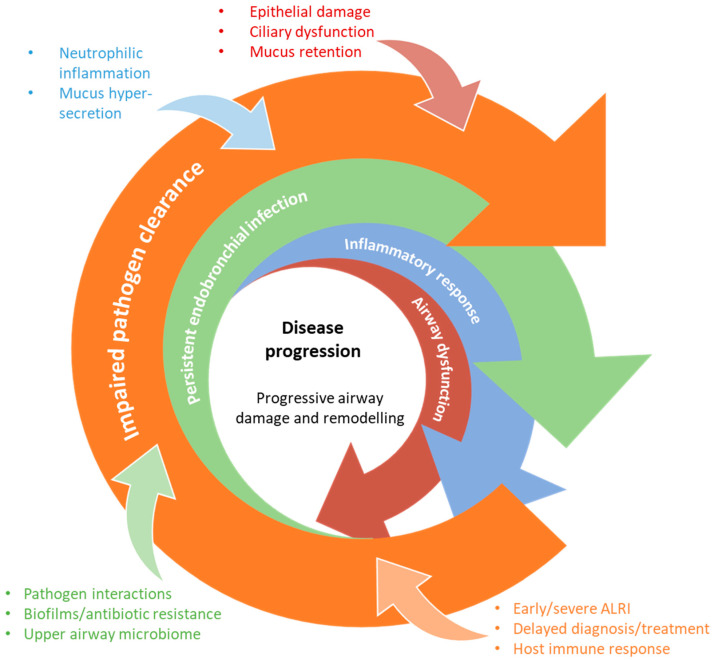
Figure 2.
The “vicious vortex” pathogenesis hypothesis of CSLD. Adapted from the model originally proposed by Flume and colleagues [21]. Following an initial trigger event, host- and pathogen-associated factors interact in a non-linear fashion to drive disease progression. Chronic and progressive neutrophilic airway inflammation and mucus hypersecretion/hyper-responsiveness leads to destruction of the bronchial wall, loss of cilia, and subsequent mucociliary dysfunction and mucus retention. This impacts on pathogen clearance, resulting in a self-perpetuating cycle of endobronchial infection, inflammation, and ongoing tissue damage.