Abstract
In a cross-sectional survey of US acute care hospitals, antimicrobial stewardship programs were present in most Veterans Affairs and nonfederal hospitals but varied in team composition, scope, and impact. Diagnostic stewardship was common across hospitals. Veterans Affairs hospitals had increased reach in outpatient settings. Telestewardship remains an opportunity in all hospital systems.
Keywords: antimicrobial stewardship, infection control, patient safety
Graphical Abstract
Graphical Abstract.
Adverse events mediated by inappropriate and unnecessary antibiotic use can be prevented through infection prevention and antimicrobial stewardship practices [1, 2]. Multidisciplinary stewardship programs have been a requirement for US hospital accreditation since 2017 and generally involve an infectious diseases (ID) physician, an infection preventionist, a pharmacist, and a practitioner [3]. Even before this national accreditation requirement was established, Veterans Affairs (VA) hospitals enacted requirements for multidisciplinary antimicrobial stewardship programs (ASPs) in >120 acute care hospitals and >100 VA nursing homes [4–6]. Given the long-standing record of antimicrobial stewardship in the VA system, we compared antimicrobial stewardship team composition in VA and nonfederal hospitals in the United States. We specifically investigated the topics of diagnostic stewardship and telestewardship, which are both growing domains within the field.
METHODS
This work was part of a continuing survey in which, every 4 years, infection preventionists are asked what practices their hospitals are using to prevent common health care–associated infections [7–10]. Survey methods have been described, and the survey is provided as Supplementary Appendix 1 [11]. For the first 3 survey waves, a national random sample was selected from all nonfederal hospitals with an intensive care unit and at least 50 hospital beds in the 2003 American Hospital Association Database. For the fourth and current waves, we selected a new random sample of 900 hospitals of all bed sizes (including those with <50 beds) from all nonfederal hospitals with an intensive care unit based on data from the 2013 American Hospital Association annual survey. Surveys were sent 127 VA hospitals and to a random sample of 881 nonfederal community hospitals. Surveys were initially sent in mid-April 2021, and reminders to nonresponders were sent after 2 weeks and again at 1, 2, and 3 months following the initial survey distribution. The majority of surveys were returned by December 2021. Institutional review board approval or exemption was obtained from the University of Michigan and the VA Ann Arbor Healthcare System.
We generated and examined descriptive statistics (proportions for categorical data and median and IQR for continuous variables) for all hospital characteristics and specific antimicrobial stewardship practices. Comparisons by hospital type (VA vs non-VA) were done by chi-square and Wilcoxon rank sum tests as appropriate. All analyses were conducted in SAS version 9.4 (SAS Inc).
RESULTS
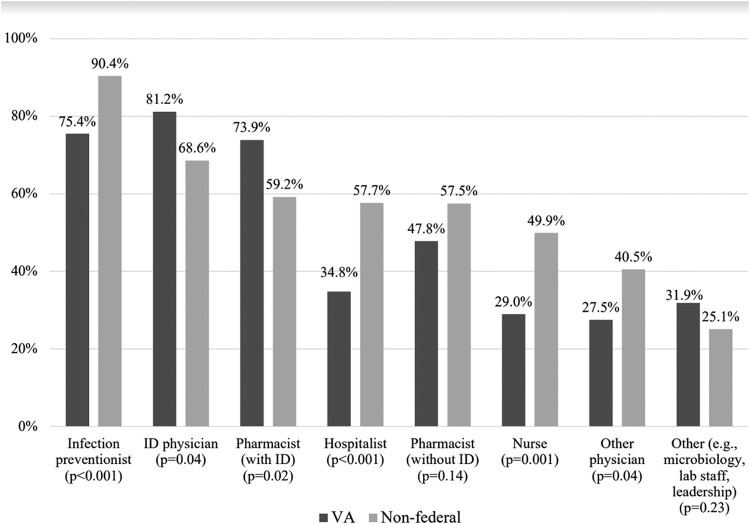
A total of 71 (56%) VA and 415 (47%) nonfederal hospitals returned surveys. Characteristics for participating hospitals are provided in Table 1. Antimicrobial stewardship team composition is illustrated in Figure 1. A total of 69 (97%) VA and 402 (97%) nonfederal responding hospitals answered survey questions pertaining to ASPs. Of these respondents, all 69 (100%) VA hospitals and 395 (98.3%) nonfederal hospitals had an ASP in place. Although antimicrobial stewardship team composition varied, ASPs were often multidisciplinary, with ID physicians, pharmacists with and without ID training, nurses, hospitalists, and infection preventionists in both VA and nonfederal settings. Antimicrobial stewardship teams in VA hospitals had higher percentages of ID physicians (81.2% vs 68.6%, P = .04) and pharmacists trained in ID (73.9% vs 59.2%, P = .02) as compared with nonfederal hospitals. Furthermore, VA stewardship teams more frequently had ID physicians and pharmacists trained in ID than nonfederal hospital stewardship teams (63.8% vs 48.6%, P = .02).
Table 1.
Comparison of VA and Nonfederal Hospital Characteristics
| VA | Nonfederal | P value | |
|---|---|---|---|
| Total beds | |||
| Acute care | 85 (31–127) | 150 (49–272) | <.001 |
| Intensive care unit | 15 (6–24) | 14 (6–26) | .52 |
| Percentage of private rooms | 72.5 (37.5–99) | 100 (70–100) | <.001 |
| Affiliated with medical school | 49 (69.0) | 141 (34.2) | <.001 |
| Hospital epidemiologist on staff | 39 (56.5) | 161 (40.4) | .01 |
| No. of full-time infection preventionists | 2 (1–4) | 1 (1–2) | <.001 |
Data are presented as No. (%) or median (IQR).
Abbreviation: VA, Veterans Affairs.
Figure 1.
Members of antibiotic stewardship teams. ID, infectious diseases; VA, Veterans Affairs.
The reach of ASPs varied between VA and nonfederal hospitals. VA ASPs more frequently had interventions in outpatient or ambulatory settings than nonfederal ASPs (60.9% vs 20.3%, P < .001). Discharge stewardship interventions were uncommon in both settings (27.5% VA vs 24.1% nonfederal, P = .53). More than half (56.5%) of VA hospitals had ASP interventions reaching nursing homes, long-term care facilities, or rehabilitation facilities, while only 12.2% of nonfederal hospitals had similar relationships with their ASPs (P < .001). We also found that providing telestewardship (10.5% VA vs 5.0% nonfederal, P = .09) and receiving it (6.2% vs 12.1%, P = .16) was rare in VA and nonfederal hospitals.
When asked about specific disease-based strategies, the most common type of ASP intervention was diagnostic stewardship aimed at reducing unnecessary urine culturing (59.1% VA vs 56.4% nonfederal, P = .68). Another common diagnostic stewardship strategy employed in both settings was reducing stool gastrointestinal pathogen panel by polymerase chain reaction tests (42.4% VA vs 38.4% nonfederal, P = .54).
In our questions on Clostridioides difficile (CDI) prevention, we found that diagnostic stewardship practices, such as discouraging testing for CDI among patients taking laxatives, were common in both settings (58.5% VA vs 66.6% nonfederal, P = .2). Communication of hospital-wide CDI rates was also common (82.1% VA vs 85.8% nonfederal, P = .43).
DISCUSSION
Within this national survey of US hospitals, ASPs were present in most hospitals and were often multidisciplinary. This is in line with goals of the US Centers for Disease Control and Prevention and likely was encouraged by regulatory requirements nationally. As prevalence of ASPs has risen in the United States, the multidisciplinary nature of teams has also grown and is likely increasing nationally and worldwide [12, 13]. We suspect that one of the reasons why multidisciplinary ASPs are common in the VA system is the recent development and validation of a staffing calculator that factors in hospital size, expected ASP activities, mean time to complete each ASP activity, and time spent related to stewardship (ie, committees, guidelines, and didactic education) [14].
The VA recommends, at minimum, full-time equivalent investments of 1.0 and 0.25 per 100 occupied beds for an ID pharmacist and an ID physician, respectively. Nurses were more likely to be members of ASP teams in nonfederal hospitals, but we anticipate that nursing presence on VA ASPs will increase in future surveys given the expansion of multidisciplinary teams in medicine. Having multidisciplinary full-time equivalent requirements for ASPs is novel and should help increase the impact and scope of ASPs in the VA system.
We found that, when compared with nonfederal systems, many VA ASPs had interventions reaching locations outside the hospital where health care was delivered, including nursing homes, long-term care facilities, or rehabilitation facilities associated with hospitals. This may be due to the integrated infrastructure that VA hospitals have as compared with nonfederal hospitals and to the decreased burden of care fragmentation when switching between health systems [15]. We anticipate that reach of these programs will continue to grow in nursing homes where ASPs were mandated by the Joint Commission in 2017 [16–18]. System-wide antimicrobial stewardship, as it becomes more common, may also lead to centralized ASPs reaching patients within a network or system in a more effective manner [19]. Outpatient stewardship is a growing field, and outpatient ASPs are part of a new Joint Commission requirement, which will likely lead to further system-wide stewardship initiatives and additional opportunities to survey [20].
Regarding diagnostic stewardship, our study found that diagnostic strategies, particularly focused on testing for CDI, were common in VA and nonfederal hospitals (Supplementary Table 1). Diagnostic stewardship is a growing field, often focused on strategies to reduce unnecessary testing [21]. A multidisciplinary team can help support diagnostic stewardship given that these interventions often work along a stream of workflow that can include frontline providers, such as the emergency department, the microbiology laboratory, and inpatient primary teams.
It was surprising to see that so few hospitals had telestewardship programs in place for providing or receiving help with antimicrobial stewardship. Telestewardship was a developing area of antimicrobial stewardship in the United States prior to the COVID-19 pandemic and became even more of a national topic of interest in the pandemic era [18]. A recent systematic review of 14 telestewardship studies found a collective decrease in targeted antimicrobial use and improved fiscal outcomes with variable effects on length of stay, mortality, and CDI rates [22]. Given the increasing requirements for having ASPs in place and the limited ID workforce, we believe that repeated surveys in the future will show an upward trend. As the VA has done in the past with ASPs, mandating telestewardship services or supporting them with dedicated full-time equivalents in hospital systems could make an impact on having these services.
Our study had limitations. We relied on health systems self-reporting in answering the survey. While we attempted to obtain a nationally representative sample, it is possible that there was selection bias in which hospitals chose to respond to the survey. The infection preventionists who received the survey may not be have been fully knowledgeable about all the details of the ASP at their facilities. Finally, we did not collect data on the availability of members of the ASP team, so we are unable to comment on whether the lack of ID involvement in some ASPs reflected a lack of ID physicians or simply a lack of availability to participate in the program.
From these cross-sectional 2021 data, we found evidence that supports most recent work from the Centers for Disease Control and Prevention indicating that most acute care hospitals in the United States have ASPs; however, the programs themselves vastly differ by team composition and impact [23]. We look forward to work that better understands the impact that a multidisciplinary ASP can have on patient outcomes and if uptake of less common implementations, such as telestewardship and discharge stewardship, continue to grow in the United States [9, 24].
Supplementary Material
Contributor Information
Armani M Hawes, Department of Internal Medicine, Johns Hopkins University School of Medicine, Baltimore, Maryland, USA.
M Todd Greene, Department of Internal Medicine, Veterans Affairs Ann Arbor Healthcare System, Ann Arbor, Michigan, USA; Department of Internal Medicine, University of Michigan Medical School, Ann Arbor, Michigan, USA; Department of Internal Medicine, VA/UM Patient Safety Enhancement Program, Ann Arbor, Michigan, USA.
David Ratz, Department of Internal Medicine, Veterans Affairs Ann Arbor Healthcare System, Ann Arbor, Michigan, USA; Department of Internal Medicine, VA/UM Patient Safety Enhancement Program, Ann Arbor, Michigan, USA.
Karen E Fowler, Department of Internal Medicine, Veterans Affairs Ann Arbor Healthcare System, Ann Arbor, Michigan, USA; Department of Internal Medicine, VA/UM Patient Safety Enhancement Program, Ann Arbor, Michigan, USA.
Ronald E Kendall, Department of Internal Medicine, Veterans Affairs Ann Arbor Healthcare System, Ann Arbor, Michigan, USA.
Payal K Patel, Department of Internal Medicine, VA/UM Patient Safety Enhancement Program, Ann Arbor, Michigan, USA; Division of Infectious Diseases, Department of Internal Medicine, Intermountain Health, Salt Lake City, Utah, USA.
Supplementary Data
Supplementary materials are available at Open Forum Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Author contributions. M. T. G., K. E. F., and D. R. had full access to all data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: A. M. H., M. T. G., K. E. F., and P. K. P. Acquisition, analysis, or interpretation of data: M. T. G., K. E. F., and D. R. Drafting of the manuscript: A. M. H., M. T. G., P. K. P., and R. E. K. Critical revision of the manuscript for important intellectual content: all authors. Statistical analysis: M. T. G. and D. R. Obtained funding: M. T. G. and K. E. F.. Administrative, technical, or material support: M. T. G., K. E. F., and D. R. Supervision: M. T. G. and P. K. P.
Data availability. Data available upon request.
Patient consent statement. This study did not include factors necessitating patient consent.
Financial support. This work was supported by the VA National Center for Patient Safety through the VA National Center for Patient Safety.
All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. File TM Jr, Solomkin JS, Cosgrove SE. Strategies for improving antimicrobial use and the role of antimicrobial stewardship programs. Clin Infect Dis 2011; 53(suppl 1):S15–22. [DOI] [PubMed] [Google Scholar]
- 2. File TM Jr, Srinivasan A, Bartlett JG. Antimicrobial stewardship: importance for patient and public health. Clin Infect Dis 2014; 59(suppl 3):S93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis 2016; 62:e51–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kelly AA, Jones MM, Echevarria KL, et al. A report of the efforts of the Veterans Health Administration National Antimicrobial Stewardship Initiative. Infect Control Hosp Epidemiol 2017; 38:513–20. [DOI] [PubMed] [Google Scholar]
- 5. Chou AF, Graber CJ, Jones M, et al. Characteristics of antimicrobial stewardship programs at Veterans Affairs hospitals: results of a nationwide survey. Infect Control Hosp Epidemiol 2016; 37:647–54. [DOI] [PubMed] [Google Scholar]
- 6. Appaneal HJ, Caffrey AR, Lopes VV, et al. Predictors of potentially suboptimal treatment of urinary tract infections in long-term care facilities. J Hosp Infect 2021; 110:114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alegria W, Patel PK. The current state of antifungal stewardship in immunocompromised populations. J Fungi 2021; 7:352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Vaughn VM, Greene MT, Ratz D, et al. Antibiotic stewardship teams and Clostridioides difficile practices in United States hospitals: a national survey in the Joint Commission antibiotic stewardship standard era. Infect Control Hosp Epidemiol 2020; 41:143–8. [DOI] [PubMed] [Google Scholar]
- 9. Vaughn VM, Hersh AL, Spivak ES. Antibiotic overuse and stewardship at hospital discharge: the reducing overuse of antibiotics at discharge home framework. Clin Infect Dis 2022; 74:1696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Advani S, Vaughn VM. Quality improvement interventions and implementation strategies for urine culture stewardship in the acute care setting: advances and challenges. Curr Infect Dis Rep 2021; 23:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Saint S, Kowalski CP, Forman J, et al. A multicenter qualitative study on preventing hospital-acquired urinary tract infection in US hospitals. Infect Control Hosp Epidemiol 2008; 29:333–41. [DOI] [PubMed] [Google Scholar]
- 12. Sadeq AA, Shamseddine JM, Babiker ZOE, et al. Impact of multidisciplinary team escalating approach on antibiotic stewardship in the United Arab Emirates. Antibiotics 2021; 10:1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Liu Y-X, Liang C, Yang Y, et al. Reduction in antimicrobial use associated with a multifaceted antimicrobial stewardship programme in a tertiary teaching hospital in Shanghai: a segmented regression analysis. Ann Palliat Med 2021; 10:7360–9. [DOI] [PubMed] [Google Scholar]
- 14. Echevarria K, Groppi J, Kelly AA, Morreale AP, Neuhauser MM, Roselle GA. Development and application of an objective staffing calculator for antimicrobial stewardship programs in the Veterans Health Administration. Am J Health Syst Pharm 2017; 74:1785–90. [DOI] [PubMed] [Google Scholar]
- 15. Sturm L, Flood M, Montoya A, Mody L, Cassone M. Updates on infection control in alternative health care settings. Infect Dis Clin North Am 2021; 35:803–25. [DOI] [PubMed] [Google Scholar]
- 16. Buckel WR, Stenehjem EA, Hersh AL, Hyun DY, Zetts RM. Harnessing the power of health systems and networks for antimicrobial stewardship. Clin Infect Dis 2022; 75:2038–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Livorsi DJ, Abdel-Massih R, Crnich CJ, et al. An implementation roadmap for establishing remote infectious disease specialist support for consultation and antibiotic stewardship in resource-limited settings. Open Forum Infect Dis 2022; 9:ofac588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Suzuki H, Shealy S, Throneberry K, Stenehjem E, Livorsi D. Opportunities and challenges in improving antimicrobial use during the era of telehealth expansion: a narrative review. Antimicrob Steward Healthc Epidemiol 2021; 6:e26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aronow W. Clinical causes of death of 2372 older persons in a nursing home during 15-year follow-up. J Am Med Dir Assoc 2000; 1:95–6. [PubMed] [Google Scholar]
- 20. Joint Commission . Antimicrobial stewardship in ambulatory health care. 2019. Available at: https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/r3_23_antimicrobial_stewardship_amb_6_14_19_final2.pdf. Accessed June 1, 2023.
- 21. Fabre V, Carroll KC, Cosgrove SE. Blood culture utilization in the hospital setting: a call for diagnostic stewardship. J Clin Microbiol 2022; 60:e01005-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mailig M, Cookson NA, Schulz LT. Telestewardship programs support clinical care and improve fiscal outcomes across the continuum through partnership between hospitals and health systems: a systematic review. Am J Health Syst Pharm 2022; 79:1663–73. [DOI] [PubMed] [Google Scholar]
- 23. Centers for Disease Control and Prevention . Antibiotic use in the United States, 2022 update: progress and opportunities. 2023. Available at: https://www.cdc.gov/antibiotic-use/stewardship-report/current.html. Accessed June 1, 2023.
- 24. Pierce J, Stevens MP. The emerging role of telehealth in antimicrobial stewardship: a systematic review and perspective. Curr Treat Options Infect Dis 2021; 13:175–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.