Abstract
Introduction
Inversion of the patient, forced diuresis after hydration, and mechanical percussion technique was developed for lower renal pole (LRP) stones with extracorporeal shock wave (ESWL). In this study, we aimed to analyze the effect of percussion, diuresis and inversion (PDI) therapy on the success rates of retrograde intrarenal surgery (RIRS) for the LRP stones.
Material and methods
114 patients who underwent RIRS for LRP stones <2cm were included in this study. Patients' demographic, clinical, radiological and anatomical features and success status were recorded prospectively. The patients were divided into two groups. One group received RIRS procedure only (non-PDI group) and the other group received PDI therapy after the RIRS procedure (PDI group).
Results
PDI was performed to 60 (52.6%) patients, and not performed to 54 (47.4%) patients. The success rate (58.3%) for the PDI group was higher than the non-PDI group (25.9%), and this difference was statistically significant (p <0.001). In multivariate logistic regression analysis, stone size (OR = 1.306; 95% CI = 1.019–1.674; p <0.001), IU (OR = 1.702; 95% CI = 1.383–2.096; p <0.001) and not performing PDI therapy (p <0.001) OR = 9.455; 95% Cl = 2.426–10.853; p = 0.001) were revealed to be independent risk factors for failure.
Conclusions
PDI therapy increases the success rates of RIRS performed for the LRP stones.
Keywords: lower renal pole stone, PDI, retrograde intrarenal surgery
INTRODUCTION
Renal stones comprise a heterogeneous set of cases, where the need for active therapy is defined by various factors, such as stone growth, the manifestation of symptoms, infection, and patient preferences. Recommendations relating to the decision about surveillance or active removal are not supported by high-level evidence and 7–26% of the cases result in the surgical intervention [1]. Another element of heterogeneosity of renal stones is the wide range in the stone size and position, which affects significantly the optimal operative procedure for active removal.
Stones in the lower renal pole (LRP) comprise a subset of cases characterized by an inherent difficulty in the evacuation of stone burden, which is attributed to the relative position of inferior calyces in combination with the effect of gravity. Indeed, the European guidelines propose a modified algorithm, especially for the LRP stones 1–2 cm, which depends on the geometric features of the kidney and the stone hardness [2]. For the same stone class, American guidelines vary slightly, since they recommend against the use of extracorporeal shock wave lithotripsy (ESWL) for LRP stones 1–2 cm, regardless of the renal geometry [3].
Retrograde intrarenal surgery (RIRS) constitutes one of the available modalities for the removal of LRP stones, especially, after the introduction of high-power laser generators and ureteroscopes with maximum deflection capability. According to European guidelines, RIRS is indicated as the first option for LRP stones <2 cm, while it is considered the second option for more voluminous stones [2]. The comparison of the three available modalities for the LPR stones <2 cm demonstrated that stone-free rate (SFR) reached the higher percentage after percutaneous nephrolithotomy (PNL) at the cost of higher morbidity and longer hospital stay, while ESWL was the less invasive and effective [4]. In another study, the authors collected and pooled the reported data on the effectiveness and safety of the available modalities [5]. RIRS seemed to achieve inferior results compared to PNL, miniPNL, and better SFRs than microPNL, and ESWL, while the complication rates of the modalities were not significantly different.
Regarding RIRS, the latest technological advances have extended its efficacy and safety in almost every stone class. Nevertheless, in the case of LRP stones, RIRS is still subject to restrictions relating to renal geometry. According to a study reporting the pooled data until 2019, steep infundibular-pelvic angle (IPA) was the most important factor for the RIRS success, while infundibular width (IW) and infundibular length (IL) did not influence outcomes [6]. In 2021, Tastemur et al. studied the factors affecting RIRS outcomes and concluded that an IPA <42.65°, IL >27.5 mm and stone volume were independent risk factors for RIRS failure [7]. A recent study from Inoue et al. focused on the accessibility of the lower calyces by reusable flexible ureteroscope and concluded that an IPA <45.8° and IW <7.8 mm were negative predictors for reaching lower calyces during RIRS [8]. The continuously growing experience in applying RIRS for LRP stones has driven the introduction of novel techniques, such as the relocation of stones to more convenient points of intrarenal anatomy before laser fragmentation, which allowed the further improvement of SFR [9].
Considering the geometrical nature of the difficulty in evacuating the burden of LRP stones, a number of techniques were developed to invert the adverse factors to stone removal, such as the patient inversion, the forced diuresis after hydration and the mechanical percussion on the area of the operated kidney. These techniques were tested with success for increasing SFR after ESWL. Chiong et al. reported a significant improvement in stone clearance from 35.5% to 62.5% after applying a percussion-diuresis-inversion (PDI) therapy on ESWL-treated patients [10]. Albanis et al. applied a hydration-diuresis-inversion protocol during the ESWL procedure and achieved a significant SFR improvement from 71.5% to 83.3% [11]. Leong et al. studied the effect of only inversion during ESWL, which invoked a trend for improved SFR, but without statistically significant differences compared to patients without inversion maneuver [12]. Another study reported on the outcomes of PDI application after the ESWL procedure and concluded that PDI can improve by 1.9 times the SFR in the respective patient group [13]. Ahmed et al. studied prospectively the effect of intraprocedural increased diuresis and inversion on the ESWL results [14]. The authors reached to the conclusion that the additional diuresis-inversion protocol achieved significantly higher SFRs at all follow-up time points. Of note, in all of the above studies, no differences were found between the complication rates of the comparing groups.
Considering the available data on PDI application on ESWL results as promising, we designed the current study to measure the effect of PDI on the RIRS outcomes regarding LRP stones. Any positive effect of PDI on these outcomes would be of great clinical significance since it would allow the further improvement of RIRS performance in this difficult stone class.
MATERIAL AND METHODS
We analyzed 131 patients who underwent RIRS for LRP stones <2 cm between 01.06.2021 and 31.01.2022 in our clinic prospectively. The patients were prospectively randomized (using simple randomization by computer) to two groups. One group received RIRS procedure only (non-PDI group) and the other group received PDI therapy after the RIRS procedure (PDI group). Patients with LRP stones <2 cm and approving the treatment method were included in the study. Patients with a history of cerebrovascular disease, uncontrolled hypertension, bleeding diathesis disorder, anticoagulation therapy, distal ureteral stenosis, pregnancy, severe skeletal malformation, severe obesity, urinary tract infection were excluded from the study. Finaly, 114 patients were included in this study.
Our study was prepared in accordance with the Principles of Helsinki, it was reviewed and approved by the 2nd Clinical Research Ethics Commitee of Ankara City Hospital on 10.03.2021 (Ethics committee approval number: E2-21-158).
Age, sex, body mass index (BMI), preoperative double-J (DJ) stent presence, ESWL history presence were obtained from the anamnesis of the patients and recorded. The operation durations were also recorded.
Stone size, density, number (single or multiple), side (left-right) were evaluated according to preoperative computed tomography. Stone size was measured as the longest diameter of the stone. For the multiple stone number patients, stone size was calculated as the sum of all stones longest diameter.
IPA was measured as the internal angle formed at the intersection of the ureteropelvic axis and the central axis of the lower pole infundibulum. IL was measured as the distance from the furthest point below the calyx containing the stone to the midpoint of the lower border of the renal pelvis.
Patients with positive urine cultures were treated with appropriate antibiotics for at least 7 days. Preoperative urine cultures of all patients were sterile. All patients were given prophylaxis with intravenous 2 g cefazolin within 1 hour before surgery. RIRS was performed in all patients in the lithotomy position under general anesthesia.
Before RIRS, ureterorenoscopy was performed with a 9.5 F rigid renoscope (Karl Storz, Tuttingen, Germany) for dilatation. A 9.5–11 F ureteral access sheath (Flexor® Ureteral Access Sheath, Cook Medical, USA) was placed in the ureter to reduce intrarenal pressure and provide optimal viewing. After the access sheath reached the collector system, the collector system was reached by entering through the access channel with a 7.5 F flexible ureterorenoscope (Karl Storz, Flex X2, GmbH, Tuttlingen, Germany). The stone was fragmented using a holmium-yttrium-aluminum-garnet (Ho:YAG) laser (200 µm) sent from the working channel of the flexible ureterorenoscope. At the end of the operation, DJ catheter and urethral catheter were applied to all cases.
PDI therapy was performed as follows: In the postoperative period, oral hydration was applied to the patients by allowing them to drink 500 ml of water within 30 minutes after oral intake permission. 30 minutes later, the patient was fixed to the bed for inversion, the patient bed was adjusted to 30° Trendelenburg position. Then, percussion was performed in prone position for 5 minutes, in the position that the operated side was elevated to 45° with the pillow for 5 minutes, in full flank position for 5 minutes and in the supine position for 5 minutes, by hitting the flank area with the palm of the hand for a total of 20 minutes. Subsequently, the bed was placed in the neutral position while the patient was in the supine position and rested for 10 minutes. The process was terminated after 30 minutes.
Patients were evaluated with non-contrast abdominopelvic computed tomography (CT) at 1 month postoperatively. Absence of stones in the urinary tract was accepted as success.
Data coding and statistical analyzes were performed on the computer using the SPSS 22 software package program (IBM SPSS Statistics, IBM Corporation, Chicago, IL). The conformity of the variables to the normal distribution was examined using the Shapiro-Wilk tests. Mann-Whitney U test was used to compare non-categorical parameters between groups. Chi-square or Fisher's exact tests were used for categorical variables. Risk factors for RIRS success in lower pole stones were determined by univariate logistic regression analysis. Whether the possible factors identified in this analysis were independent risk factors were evaluated using the Bacward LR method with multivariate analysis. Cases with a p value below 0.05 were considered statistically significant.
RESULTS
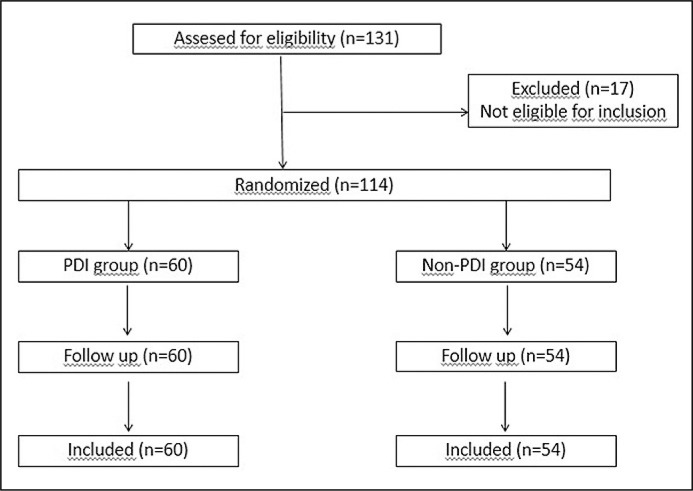
A total of 114 patients who underwent RIRS for LRP stones were included in the study. 60 (52.6%) of patients were in PDI group and 54 (47.4%) patients were in non-PDI group (Figure 1). The mean age of patients was 45.1 ±9.7 years. 81 (71.1%) patients were male and 33 (28.9%) patients were female. The success rate was 43% in all cases. There was no significant difference between two groups in terms of age, gender, BMI, stone size, stone density, stone number, operation time, lateralization, preoperative DJ stent history, ESWL history, IPA, IL and IW. The success rate was higher in the PDI group (58.3% vs 25.9%, p <0.001) Comparative analyzes of demographic, clinical and radiological characteristics of patients between two groups was shown in Table 1.
Figure 1.
Flow chart of patients.
Table 1.
Comparative analysis of demographic, clinical and radiological characteristics of patients who underwent RIRS for lower renal pole stone with or without PDI therapy in the postoperative period
| Total(n = 114) | PDI group(n = 60, % 52.6) | Non-PDI group(n = 54, % 47.4) | p | |
|---|---|---|---|---|
| Age (year) | 45.1 ±9.7 | 44 ±6.4 | 46.4 ±12.3 | 0.267m |
| Sex Men, n (%) Women, n (%) |
81 (71.1) 33 (28.9) |
35 (58.3) 25 (41.7) |
46 (85.2) 8 (14.8) |
0.24k |
| BMI (kg/m2) (mean ±SD) | 29.1 ±3.6 | 28.7 ±3.1 | 29.6 ±4.1 | 0.208m |
| Stone size (mm) (mean ±SD) | 12.6 ±2.9 | 12.8 ±2.6 | 12.5 ±3.2 | 0.471m |
| Stone density (HU) (mean ±SD) | 995.5 ±238 | 1029.3 ±186.5 | 958 ±281.6 | 0.532m |
| Stone number Single, n (%) Multiple, n (%) |
103 (90.4) 11 (9.6) |
55 (91.7) 5 (8.3) |
48 (88.9) 6 (11.1) |
0.609f |
| Operation time (min) (mean ±SD) | 57.5 ±13.8 | 54.3 ±8.7 | 61 ±17.3 | 0.072m |
| Lateralization Right, n (%) Left, n (%) |
51 (44.7) 63 (55.3) |
27 (45) 33 (55) |
24 (44.4) 30 (55.6) |
0.121k |
| Preoperative DJ stent history Yes, n (%) No, n (%) |
43 (37.7) 71 (62.3) |
19 (31.7) 41 (68.3) |
24 (44.4) 30 (55.6) |
0.563k |
| ESWL history Yes, n (%) No, n (%) |
42 (36.8) 72 (63.2) |
20 (33.3) 40 (66.7) |
22 (40.7) 32 (59.3) |
0.71k |
| IPA (degree) (mean ±SD) | 54.5 ±8.9 | 56.3 ±9.3 | 52.5 ±8 | 0.104m |
| IL (mm) (mean ±SD) | 25.8 ±5.7 | 24.6 ±6.1 | 27.1 ±5 | 0.051m |
| IW (mm) (ortalama ±SD) | 4.7 ±1.3 | 4.6 ±0.8 | 4.8 ±1.8 | 0.39m |
| Success, n (%) | 49 (43) | 35 (58.3) | 14 (25.9) | <0.001k |
RIRS – retrograde intrarenal surgery, PDI – percussion, diuresis ve inversion, BMI – body mass index, HU – Hounsfield unit, DJ – double J, ESWL – extracorporeal shock wave lithotripsy, IPA – infundibulopelvic angle, IL – infundibular length, IW – infundibular width, SD – standard deviation,
– Mann Whitney U test,
– Ki-kare Test,
– Fisher’s exact test
In univariate logistic regression analysis, age (OR = 0.959; 95% Cl = 0.921–1; p = 0.048), stone size (OR = 1.27; 95% Cl = 1.096–1.471; p = 0.001), IPA (OR = 0.857; 95% CI = 0.081–0.908; p <0.001), IL (OR = 1.569; 95% CI = 1.333–1.848; p <0.001), IW (OR = 0.673; 95% CI = 0.482–0.941; p = 0.02) and not performing PDI (OR = 4; 95% CI = 1.804–8.868; p <0.001) were found as risk factors for the success of RIRS procedure for LRP stones. Subsequently, in multivariate logistic regression analysis, only stone size (OR = 1.306; 95% CI = 1.019–1.674; p <0.001), IL (OR = 1.702; 95% CI = 1.383–2.096; p <0.001) and not performing PDI (OR = 9.455; 95% Cl = 2.426–10.853; p = 0.001) were stated as independent risk factors (Table 2). Patient placed in prone Trandelenburg position on 30°-angled bed for 20 minutes percussion, diuresis and inversion (PDI) therapy is presented at Figure 2.
Table 2.
Determination of the risk factors for failure on RIRS for lower renal pole stones with univariate and multivariate regression analysis
| Univariate | Multivariate | |||
|---|---|---|---|---|
| OR (% 95 CI) | p | OR (% 95 CI) | p | |
| Age (per year) | 0.959 (0.921–1) | 0.048 | 0.939 (0.872–1.011) | 0.096 |
| Sex (Male) | 0.615 (0.272–1.389) | 0.242 | ||
| BMI (per kg/m2) | 1.035 (0.933–1.148) | 0.518 | ||
| Stone size (per mm) | 1.27 (1.096–1.471) | 0.001 | 1.306 (1.019–1.674) | 0.035 |
| Stone density (per HU) | 1.001 (0.999–1.002) | 0.508 | ||
| Stone number (multiple) | 1.883 (0.461–7.691) | 0.378 | ||
| Lateralization (Left) | 1.809 (0.853–3.834) | 0.122 | ||
| Preoperative DJ stent presence | 1.255 (0.581–2.709) | 0.563 | ||
| ESWL history presence | 0.865 (0.401–1.862) | 0.71 | ||
| IPA (per degree) | 0.857 (0.81–0.908) | <0.001 | 0.982 (0.9–1.07) | 0.673 |
| IL (per mm) | 1.569 (1.333–1.848) | <0.001 | 1.702 (1.383–2.096) | <0.001 |
| IW (per mm) | 0.673 (0.482–0.941) | 0.02 | 0.905 (0.61–1.342) | 0.619 |
| Not performing PDI | 4 (1.804–8.868) | 0.001 | 9.455 (2.426–10.853) | 0.001 |
RIRS – retrograde intrarenal surgery, PDI – percussion, diuresis and inversion, BMI – body mass index, HU – Hounsfield unit, DJ – double J, ESWL – extracorporeal shock wave lithotripsy, IPA – infundibulopelvic angle, IL – infundibular length, IW – infundibular width
Figure 2.
Patient placed in prone Trandelenburg position on 30°-angled bed for 20 minutes percussion, diuresis and inversion (PDI) therapy
DISCUSSION
From the above results can be extrapolated, that the effect of PDI seen on the stone clearance after ESWL, is also present in the patients, which undergo RIRS for LRP stones. The comparing groups (PDI, non-PDI) demonstrated no significant differences in terms of factors that can affect the result of RIRS, such as BMI, stone size, stone density, renal geometry, and previous treatments, which renders them comparable. The success rate of the comparing groups was significantly different since 32% more patients in the PDI group were stone-free at the preselected FU time point. In order to delineate the effect of possible confounders on the above result, we proceeded with multivariate analysis through logistic regression. The factors found significant in the univariate analysis were age, stone size, the parameters of renal geometry, and the application of PDI. After the inclusion of these factors in the multivariate model, only stone size, IL, and PDI application retained their statistical significance as independent determiners of RIRS results. Among these independent factors, PDI application demonstrated a strong effect, since the absence of PDI increased the possibility of RIRS failure by more than nine times.
After a thorough search in the available literature, we found few reports relating to the contribution of physical methods, such as external percussion, and patient inversion in the improvement of RIRS outcomes. In 2017, Wu et al. investigated the effect of an external vibration device (Lithecbole) on patients with residual fragments after the RIRS procedure [15]. The study resulted in increased SFR at every follow-up time point for the patients, who received supplementary external vibration sessions. Another study about the effect of the same physical method (Lithecbole) on the SFR after RIRS, investigated the optimal time point to apply the above-mentioned method and concluded, that it should be applied in the early postoperative period (3 days after RIRS) [16]. In 2020, a meta-analysis by Yuan et al. collected and pooled the available data on the Lithecbole application [17]. The analysis demonstrated that this method can increase SFR regardless of the stone position. An alternative approach was proposed in the study by Yang et al., where the patients with stone remnants after RIRS were divided into a control group and an inverse position group [18]. The last group achieved higher SFR at every follow-up time point compared to the control group. Recently, promising results were reported from an experimental study based on renal models, which were set to an inverted position by using an automated system, that calculated the optimal inversion degree by processing the extrapolated from the computer tomography renal geometry [19]. More precisely, the automated system provided individualized inversion, which allowed the optimization of stone burden evacuation.
Among the above results, there was no study focusing on the LRP stones and their evacuation by physical methods, such as PDI. Another advantage of the current study is the further statistical processing of the data, which allowed the delineation of the independent factors affecting the results after RIRS for LRP stones. PDI demonstrated a very strong effect, which reflects its potential in improving the RIRS outcomes, even for the difficult stone classes.
In our opinion, the physical methods for improving SFR should be applied in a combined manner, because the existing experience from PDI after ESWL demonstrates that this approach produces the most promising results. Moreover, there is much to be done regarding the standardization of PDI application, and various parameters, such as session duration, number of sessions, and protocol configuration remain to be tested for optimized results.
CONCLUSIONS
LRP stones constitute a challenging stone class, where gravity and renal geometry can hinder the evacuation of stone burden. The effect of the above factors, which reduces the success rate of RIRS can be neutralized by the application of physical methods, such as mechanical percussion, forced diuresis, and inversion of the patient. In the current study, PDI therapy contributed significantly and independently to the SFR improvement. This result comes in line with the existing experience from post-ESWL PDI application and renders PDI worth of further investigation for its applicability to optimize RIRS outcomes.
CONFLICTS OF INTEREST
The authors declare no conflicts of interest.
References
- 1.Han DS, Cher BA, Lee D, et al. The durability of active surveillance in patients with asymptomatic kidney stones: a systematic review. J Endourol. 2019; 33: 598-605. [DOI] [PubMed] [Google Scholar]
- 2.EAU Guidelines . Edn. presented at the EAU Annual Congress Amsterdam 2022. Arnhem, the Netherlands: EAU Guidelines Office; 2022. [Google Scholar]
- 3.Assimos D, Krambeck A, Miller NL, et al. Surgical Management of Stones: American Urological Association/Endourological Society Guideline, PART II. J Urol. 2016; 196: 1161-1169. [DOI] [PubMed] [Google Scholar]
- 4.Donaldson JF, Lardas M, Scrimgeour D, et al. Systematic review and meta-analysis of the clinical effectiveness of shock wave lithotripsy, retrograde intrarenal surgery, and percutaneous nephrolithotomy for lower-pole renal stones. Eur Urol. 2014; 67: 612-616. [DOI] [PubMed] [Google Scholar]
- 5.Tsai SH, Chung HJ, Tseng PT, et al. Comparison of the efficacy and safety of shockwave lithotripsy, retrograde intrarenal surgery, percutaneous nephrolithotomy, and minimally invasive percutaneous nephrolithotomy for lower-pole renal stones: A systematic review and network meta-analysis. Medicine (Baltimore). 2020; 99: e19403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karim SS, Hanna L, Geraghty R, et al. Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal surgery (RIRS) for lower pole stones: outcomes with a systematic review of literature. Urolithiasis. 2020; 48: 263-270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tastemur S, Senel S, Kizilkan Yet al. Evaluation of the anatomical factors affecting the success of retrograde intrarenal surgery for isolated lower pole kidney stones. Urolithiasis. 2022; 50: 65-70. [DOI] [PubMed] [Google Scholar]
- 8.Inoue T, Hamamoto S, Okada S, et al. Pelvicalyceal anatomy on the accessibility of reusable flexible ureteroscopy to lower pole calyx during retrograde intrarenal surgery. Int J Urol. 2023; 30: 220-225 [DOI] [PubMed] [Google Scholar]
- 9.Golomb D, Goldberg H, Tapiero S, et al. Retrograde intrarenal surgery for lower pole stones utilizing stone displacement technique yields excellent results. Asian J Urol. 2023; 10: 58-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiong E, Tay SPH, Li MK, et al. Randomized controlled study of mechanical percussion, diuresis, and inversion therapy to assist passage of lower pole renal calculi after shock wave lithotripsy. Urology. 2005; 65: 1070-1074. [DOI] [PubMed] [Google Scholar]
- 11.Albanis S, Ather HM, Papatsoris AG, et al. Inversion, hydration and diuresis during extracorporeal shock wave lithotripsy: does it improve the stone-free rate for lower pole stone clearance? Urol Int. 2009; 83: 211-216. [DOI] [PubMed] [Google Scholar]
- 12.Leong WS, Liong ML, Liong YV, et al. Does simultaneous inversion during extracorporeal shock wave lithotripsy improve stone clearance: a long-term, prospective, single-blind, randomized controlled study. Urology. 2014; 83: 40-44. [DOI] [PubMed] [Google Scholar]
- 13.Saleem MA, Younis M, Khan JH, et al. Comparison of Lower Pole Renal Calculi Clearance after Extracorporeal Shock Wave Lithotripsy with and without percussion, diuresis and inversion maneuver. Pak J Med. 2015; 9: 293-295. [Google Scholar]
- 14.Ahmed AF, Shalaby E, Maarouf A, et al. Diuresis and inversion therapy to improve clearance of lower caliceal stones after shock wave lithotripsy: A prospective, randomized, controlled, clinical study. Indian J Urol. 2015; 31: 125-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu W, Yang Z, Xu C, et al. External Physical Vibration Lithecbole Promotes the Clearance of Upper Urinary Stones after Retrograde Intrarenal Surgery: A Prospective, Multicenter, Randomized Controlled Trial. J Urol. 2017; 197: 1289-1295. [DOI] [PubMed] [Google Scholar]
- 16.Zhang Y, Xu C, Wang Y, et al. When is the best time to perform external physical vibration lithecbole (EPVL) after retrograde intrarenal surgery (RIRS): a multi-center study based on randomized controlled trials. Urolithiasis. 2020; 48: 533-539. [DOI] [PubMed] [Google Scholar]
- 17.Yuan C, Jian Z, Jin X, et al. Efficacy and safety of external physical vibration lithecbole after extracorporeal shock wave lithotripsy or retrograde intrarenal surgery for urinary stone: a systematic review and meta-analysis. J Endourol. 2021; 35: 712-720. [DOI] [PubMed] [Google Scholar]
- 18.Yang J, Tao R-z, Lu P, et al. Efficacy analysis of self-help position therapy after holmium laser lithotripsy via flexible ureteroscopy. BMC Urol. 2018; 18: 1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang T, Song R, Meng X, et al. A single center study that evaluates the preclinical use of a newly developed software and moving bed system to facilitate the spontaneous excretion of residual fragments after primary stone treatment (RIRS or PCNL). World J Urol. 2022; 40: 585-591. [DOI] [PMC free article] [PubMed] [Google Scholar]