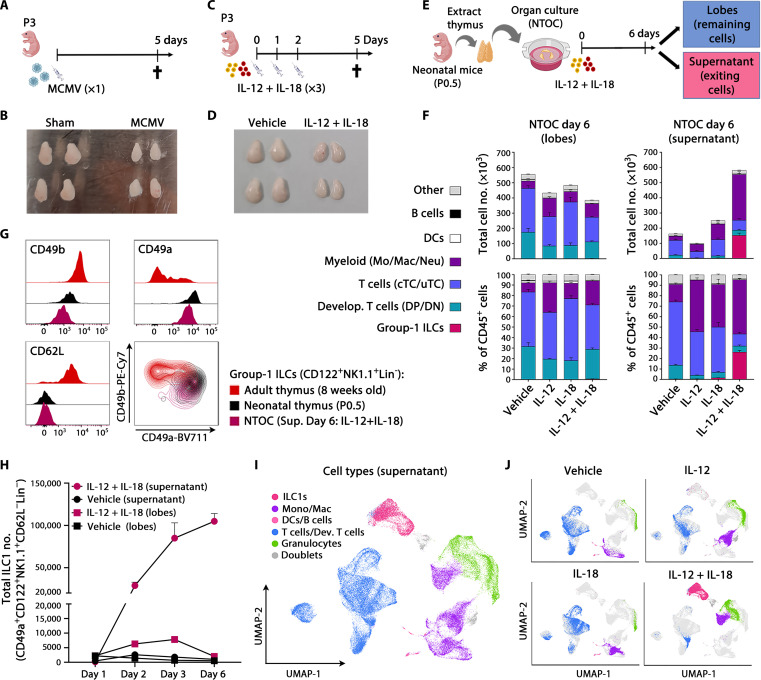
Fig. 1. Type 1 inflammation induces expansion of thymus-exiting ILC1s during NTOC.
(A) Schematic of MCMV infections in neonates. (B) Picture of thymic lobes 5 days after infection with MCMV or sham, representative of five independent experiments, as shown in (A). (C) Schematic of IL-12 + IL-18 injections in neonates. (D) Picture of thymic lobes 5 days after the first injection with IL-12 + IL-18 or vehicle, representative of four independent experiments, as shown in (C). (E) Schematic of NTOC strategy for cellular analysis; dividing each well into lobes and supernatant. (F) Stacked bar plots of NTOC performed as illustrated in (E), showing the total number (top) and percentage (bottom) of CD45+ cell types in thymic lobes (left) and supernatant (right) (gating shown in fig. S1C). Data are representative of five independent experiments and shown for n = 3 biological replicates per condition with error bars displaying SEM. DCs, dendritic cells; DN, double negative; DP, double positive; cTC, conventional T cells; uTC, unconventional T cells; Mo, monocytes; Mac, macrophages; Neu, neutrophils. (G) Flow cytometry comparison of ILC1 and cNK markers on group-1 ILCs (CD122+NK1.1+Lin−) from the thymus in adults (8 weeks old), neonates (P0.5), and IL-12 + IL-18–stimulated NTOC supernatant (day 6). Histograms and density plots are representative of n = 6 biological replicates from two independent experiments. (H) Kinetic analysis of ILC1 expansion in NTOC (lobes and supernatant) as shown in (E). Data are representative of three independent experiments and shown for n = 3 biological replicates per condition. The y axis is divided into two different segments. Error bars display mean with SEM. (I) Uniform Manifold Approximation and Projection (UMAP) plot of scRNA-seq data on day 6 NTOC supernatant cells as shown in (E), from four conditions: (i) vehicle, (ii) IL-18, (iii) IL-12, and (iv) IL-12 + IL-18. The major cell types are divided by color. (J) Split UMAPs of the four conditions as in (I); Lin−, Lineage negative, defined as TCRβ−TCRγδ−CD3e−CD4−CD8β−Ter-119−Ly-6G−CD19−CD11c−F4/80−.