Fig. 2. Barrier systems against translocation of microorganisms.
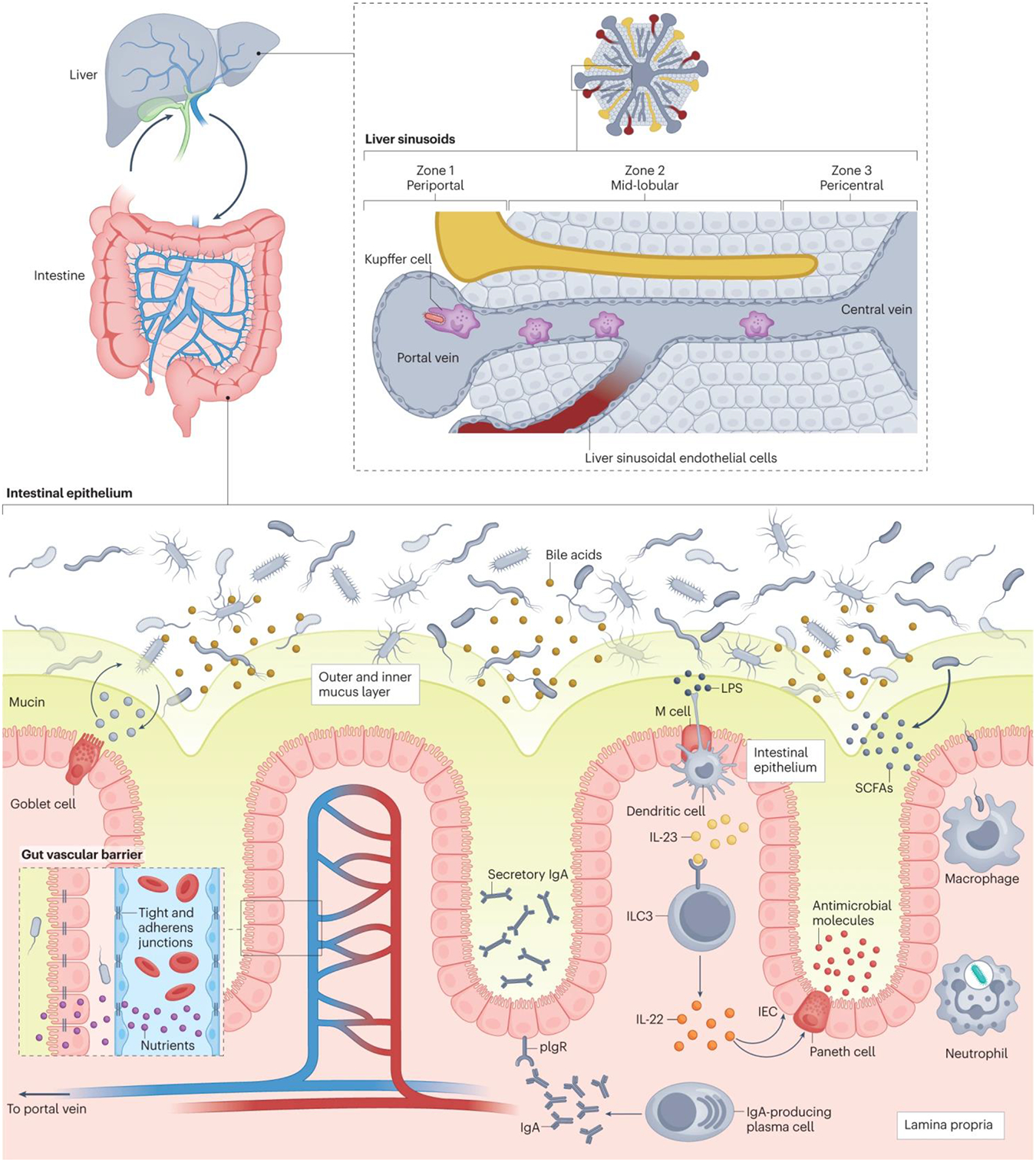
There are multiple layers of defense that prevent translocation of gut bacteria into the systemic circulation. The intestinal epithelium is the first interface, as it separates the bacteria in the gut lumen from the lamina propria below. A mucus layer (green), composed of mucins produced by goblet cells, separates the bacteria from the underlying intestinal epithelial cells. In the lamina propria (beige), whole bacteria that cross the intestinal epithelium are phagocytosed by macrophages and neutrophils. Plasma cells produce immunoglobulin A (IgA), which binds to pIgR, a receptor on enterocytes, for transport across the epithelium and secretion into the mucus layer, where this secretory IgA binds and neutralizes harmful pathobionts and pathogens. M cells in the intestinal epithelium relay microbial antigens to dendritic cells, which activate Type 3 innate lymphoid cells (ILC3) (via interleukin 23 (IL-23)) to produce interleukin 22 (IL-22). IL-22 ultimately signals Paneth cells and intestinal epithelial cells (IEC) to secrete antimicrobial molecules into the mucus layer. Short-chain fatty acids (SCFAs), produced by bacterial microbial degradation of fiber, are an energy source for enterocytes and enhance the antimicrobial activity of macrophages. Another physical barrier against bacterial translocation is the gut vascular barrier (inset box). Tight junctions and adherens junctions on endothelial cells regulate the permeability of the gut vascular barrier, allowing passage of nutrients and small molecules into the enteral circulation but restricting the passage of viable bacteria and microbial antigens. Finally, gut microorganisms that do translocate into the enteral circulation will face the liver barrier via the portal vein. In the liver, blood from the portal vein flows into the central vein via sinusoids (grey), which are lined with liver sinusoidal endothelial cells that release chemokines in response to microorganisms and microbial products. This creates a chemokine gradient that recruits Kupffer cells to the periportal zone, where they can neutralize translocated microorganims. LPS, lipopolysaccharide.
