Abstract
Objective
To identify the essential attributes of biopsychosocial rehabilitation for chronic low back pain in the working population.
Design
A concept analysis was conducted according to the 8-step method of Walker and Avant. This framework provides a clear concept and theoretical and operational definitions.
Methods
Five databases were searched, followed by a systematic screening. Subsequently, attributes, illustrative cases, antecedents, consequences and empirical referents were formulated.
Results
Of the 3793 studies identified, 42 unique references were included. Eleven attributes were identified: therapeutic exercise, psychological support, education, personalization, self-management, participation, follow-up, practice standard, goal-setting, social support, and dietary advice. Subsequently, illustrative cases were described. Antecedents, such as motivation, preparedness and a multidisciplinary team, were found, together with consequences such as decreased pain, less sick-leave and increased function and work status. Finally, examples of empirical referents were given.
Conclusion
This study identified the attributes that are necessary to develop biopsychosocial rehabilitation intervention programmes for chronic low back pain. The defined concept of biopsychosocial rehabilitation for chronic low back pain may serve as a solid base to further develop and apply interventions. Future research should focus on the objectification of biopsychosocial rehabilitation and conceptualization regarding how personalization is done.
LAY ABSTRACT
Low back pain that persists for more than 3 months is a worldwide problem with great economic consequences. Rehabilitation focusing on all the aspects of the individual, called biopsychosocial rehabilitation, has already proved to be an efficacious treatment. The requirements for such a programme are not yet clear. Therefore, the aim of this research is to clarify the concept of biopsychosocial rehabilitation and depict the essential elements that form this concept. After reviewing the recent literature, this study identified 11 essential elements, together with actions that need to be taken before the treatment, the results of the treatment and examples of cases and assessment tools. The essential elements are presented in the results and the concept is clarified for future researchers to build upon. An assessment tool for the entire concept should be developed in the future, together with conceptualization on how to adapt treatment for each individual.
Key words: low back pain, chronic pain, models, biopsychosocial, interdisciplinary research, rehabilitation, review
A cute low back pain (LBP) is a worldwide problem; its prevalence increases with age and it primarily affects the female population (1, 2). When symptoms persist for more than 3 months, a patient enters the chronic stage (3). Psychosocial factors, such as work–family imbalance and job insecurity, are also reported to influence chronic low back pain (CLBP) (4). Furthermore, disability in people with CLBP has been predicted in previous research based on earlier disability, comorbidities, age and somatization (5, 6). Due to high healthcare utilization and workday losses, the burden is not limited to the individual level (7). Health gain, for example, in CLBP, is not solely understood in terms of a reduction in morbidity; it also considers the improvement of the person’s functioning and his or her ability to participate in society (8). This view has led to the importance of adopting a biopsychosocial (BPS) model to deal with CLBP. In contrast to the previously used biomedical model, a BPS model covers biological, psychological and socioeconomic elements. It considers the individual and their environment instead of solely focusing on the illness (9). A BPS model is part of the International Classification of Functioning, Disability and Health (ICF), which was first described by the WHO in 2001 (10). The ICF is a framework for organizing and documenting information on functioning and disability. It conceptualizes functioning as a “dynamic interaction between a person’s health condition, environmental factors and personal factors” (10).
As a consequence of this shift, several worldwide guidelines have incorporated a BPS approach for the management of LBP, including the guideline of the Belgian Health Care Knowledge Centre (KCE) (11–14). The use of a BPS framework to guide LBP management is recommended, starting with non-pharmacological treatment, including education supporting self-management and resumption of activities of daily living (ADL), exercise and psychological support when dealing with persistent symptoms (15). Regarding rehabilitation in general, a BPS approach has also been adopted with a focus on functioning. A recent comparative analysis of different definitions led to a new definition of rehabilitation: a “multimodal, person-centered, collaborative process (Intervention-general) including interventions targeting a person’s capacity (by addressing body structures, functions, and activities/participation) and/or contextual factors related to performance (Intervention-specific) with the goal of optimizing the functioning (Outcome) of persons with health conditions currently experiencing disability or likely to experience disability, or persons with disability (Population)” (16). This definition clearly shows the incorporation of the BPS model and the ICF.
Although there is a growing body of knowledge; greater clarity on the definition of rehabilitation; and several studies have identified the effectiveness of a BPS approach for subacute LBP and CLBP to improve pain, disability, work-related outcomes and quality of life, there is a rapidly growing number of people with chronic conditions (17–22). This phenomenon indicates that there are obstacles that prevent rehabilitation of these patients with a BPS approach. Based on the sheer number of randomized controlled trials and systematic reviews on the topic, the described biopsychosocial rehabilitation (BPS-R) programmes have been operationalized in different ways and with different types of interventions, ranging from brief, purely educational programmes to highly intensive, tailored and goal-oriented intervention programmes (23–25). One of the obstacles of defining a BPS-R intervention programme is the absence of consensus regarding the exact attributes that should be incorporated for the working population with CLBP. The features included in the studies, such as educational programmes, cognitive behavioral therapy, exercise therapy and graded activity, among many others, may enhance the outcome of the intervention programme (26). However, there is no rationale in terms of whether these interventions should meet certain criteria to be considered a BPS-R intervention programme.
Conceptualization of a BPS-R intervention programme is necessary to compare different programmes in studies investigating effectiveness and to help implementation in future studies. The scarce evidence regarding the application of a BPS-R intervention programme is ambiguous and imprecise. Recent studies have emphasized the complexity and high level of care coordination together with the absence of conceptualization (27, 28). Therefore, the aim of this concept analysis is to fill this knowledge gap by identifying essential attributes of a BPS-R intervention programme and to offer a conceptualization for the working population with CLBP based on the recent literature.
METHODS
A concept analysis allows the researcher to systematically investigate and articulate key characteristics of an abstract and hard-to-define phenomenon by identifying the key components and understanding how they might relate to other concepts (29). There are several methodologies available to execute a concept analysis. The method of Walker and Avant (30) is an adaptation based on the model by Wilson (31) and is mostly used in literature because of its easy comprehensibility and executability (29). This methodology consists of 8 steps: selecting a concept, determining the aims of the analysis, selecting the literature, determining the attributes, identifying a model case, identifying additional cases, identifying the antecedents and consequences, and defining the empirical referents.
Step 1: selecting a concept
The concept of a BPS-R intervention programme for the working population with CLBP was the topic of interest for this concept analysis. The main reason lies in the ambiguity of the concept and the differences in understanding among team members when designing a BPS-R intervention programme.
Step 2: determining the aim of the analysis
The main aim of this concept analysis was to identify the key attributes that should be incorporated in a BPS-R intervention programme for CLBP according to recent evidence.
Step 3: selecting the literature
There is no specific guideline to select the literature for a concept analysis. Hence, a systematic literature evaluation was used to increase the credibility of the search. The literature evaluation began in October 2022 and was conducted in 5 databases (MEDLINE (via PubMed), Embase (via embase.com), Web of Science, Scopus and PsycINFO (via EBSCO)) for the time period ranging from 2010 to November 2022. The aim of the review was not to collect data on the effectiveness and the methodological strength of the studies, but rather to collect data on the content of the concept and to define key attributes (see step 4). Therefore, all methodologies were considered, provided that the reference included a description of the attributes or key components of the BPS-R concept (see the inclusion criteria below). A general search string was built and customized for each database. The search string used in MEDLINE is shown in Table SI. The retained references, stored in EndNote (Camelot UK Bidco Limited (“Clarivate Analytics”); London, UK), were processed in Rayyan (http://rayyan.qcri.org) to screen them based on title, abstract and keywords. The inclusion criteria were: (i) interventions described as a BPS-R intervention or a programme covering several components of the BPS model, (ii) references from 2010 to 2022, (iii) the working population (from 18 to 65 years), (iv) written in English, (v) the CLBP population as defined by the International Classification of Diseases 11th Revision (ICD-11) (32)) and (vi) a thorough and clear description of rehabilitation content. The exclusion criteria were: (i) M-health or E-health, (ii) other pathologies related to the lower back, (iii) no rehabilitation specifications, (iv) single modality interventions, (v) pharmacological interventions, and (vi) prevention and screening. The full texts of the references that remained after the first screening were read to extract the rehabilitation content. When the included article explicitly referred to other publications for more elaboration on the rehabilitation content, these references were also included. Two reviewers independently screened the results; disagreements were resolved by discussion until mutual agreement.
Step 4: determining the attributes
Attributes are defined as hallmarks or key characteristics that distinguish the concept from other similar or related concepts (33). A systematic, purposeful and iterative approach was applied to discover the defining attributes by: (i) reading the articles, (ii) identifying the attributes, (iii) placing them into a coding scheme using NVivo (QSR International, LLC of 35 Corporate Drive, Burlington, MA, USA), (iv) grouping and classifying them into categories, (v) discussing the categories and underlying sub-categories among the authors, and (vi) renaming the categories and sub-categories as attributes and sub-attributes. This iterative process lasted until agreement among the team of 10 authors was reached. The authors had different fields of expertise: neurosurgery, physical and rehabilitation medicine, occupational medicine, physical therapy, occupational therapy, and biomedical sciences.
Step 5: identifying a model case
Subsequently, a model case was developed by the authors to illustrate the theoretically ideal BPS-R intervention programme according to the results obtained in this concept analysis.
Step 6: identifying additional cases
The authors described 2 additional cases: a contrary case and a borderline case. The contrary case contained no or few attributes of a BPS-R intervention programme. The borderline case contained some, but not all, of the defined attributes.
Step 7: identifying the antecedents and consequences
Antecedents and consequences were defined simultaneously with the attributes. Antecedents are elements that occur prior to the BPS-R intervention. The consequences are the elements that occur as a result of the intervention. A similar methodology and discussion as in step 4 were executed until agreement was reached.
Step 8: determining the empirical referents
To check whether the attributes are measurable, empirical referents were defined for each attribute. If the attributes are measurable, then they are easier to incorporate in practice or future literature.
RESULTS
Steps 1–3
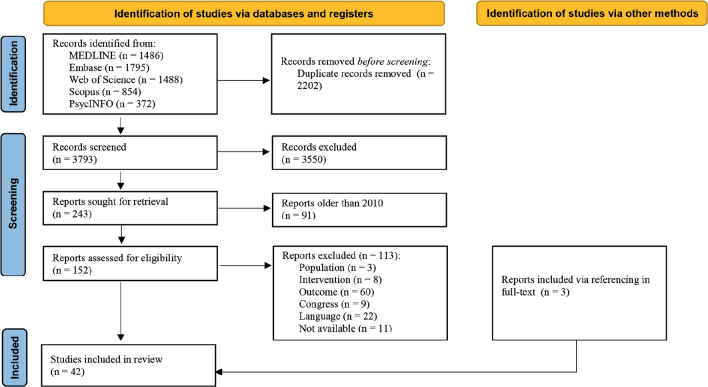
The first 2 steps of this methodology are described in the Methods. The flowchart of the study selection in step 3 is depicted in Fig. 1. The 2 independent reviewers had substantial and almost perfect agreement scores (34). The agreement between the reviewers was 73% for title and abstract screening and 87% for full-text screening. An overview of the 42 included studies is shown in Table I. The included references have a variety of study designs: 16 experimental studies, 7 study protocols, 5 prospective studies, 5 descriptive papers, 4 literature searches, 2 preliminary reports, 2 retrospective studies, and 1 clinical update.
Fig. 1.
Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagram.
Table I.
Summary of the included studies
| No. | Year | Author (Ref.) | Title |
|---|---|---|---|
| 1 | 2010 | Bosy et al. (23) | An interdisciplinary pain rehabilitation programme: description and evaluation of outcomes |
| 2 | 2010 | Demoulin et al. (36) | Effectiveness of a semi-intensive multidisciplinary outpatient rehabilitation program in chronic low back pain |
| 3 | 2010 | Dufour et al. (37) | Treatment of chronic low back pain: a randomized, clinical trial comparing group-based multidisciplinary biopsychosocial rehabilitation and intensive individual therapist-assisted back muscle strengthening exercises |
| 4 | 2010 | Giaquinto et al. (54) | A bio-psycho-social approach for treating sub-acute low back pain |
| 5 | 2010 | Luk et al. (42) | A multidisciplinary rehabilitation programme for patients with chronic low back pain: a prospective study |
| 6 | 2010 | Rodriguez-Blanco et al. (45) | Study protocol of effectiveness of a biopsychosocial multidisciplinary intervention in the evolution of non-specific sub-acute low back pain in the working population: cluster randomized trial |
| 7 | 2011 | Jensen et al. (60) | One-year follow-up in employees sick-listed because of low back pain: randomized clinical trial comparing multidisciplinary and brief intervention |
| 8 | 2011 | Roche-Leboucher et al. (44) | Multidisciplinary intensive functional restoration versus outpatient active physiotherapy in chronic low back pain: a randomized controlled trial |
| 9 | 2011 | Verkerk et al. (50) | Course and prognosis of recovery for chronic non-specific low back pain: design, therapy program and baseline data of a prospective cohort study |
| 10 | 2011 | Wetherell et al. (70) | A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain |
| 11 | 2012 | Bergström et al. (52) | Effectiveness of different interventions using a psychosocial subgroup assignment in chronic neck and back pain patients: a 10-year follow-up |
| 12 | 2012 | Moradi et al. (60) | Efficacy of multidisciplinary treatment for patients with chronic low back pain: a prospective clinical study in 395 patients |
| 13 | 2012 | Rozenberg et al. (64) | Treatment strategy for chronic low back pain |
| 14 | 2013 | Hofmann et al. (24) | Effects of behavioral exercise therapy on the effectiveness of a multidisciplinary rehabilitation for chronic non-specific low back pain: study protocol for a randomized controlled trial This article also includes supplementary material describing the BPS intervention. |
| 15 | 2013 | Nazzal et al. (43) | Management options of chronic low back pain. A randomized blinded clinical trial |
| 16 | 2013 | Steiner et al. (49) | Added value of an intensive multidisciplinary functional rehabilitation programme for chronic low back pain patients |
| 17 | 2014 | Hussain et al. (59) | Interventional pain management for failed back surgery syndrome |
| 18 | 2014 | Jay et al. (41) | Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain, stress and work ability among laboratory technicians: randomized controlled trial protocol |
| 19 | 2014 | Monticone et al. (53) | A multidisciplinary rehabilitation programme improves disability, kinesiophobia and walking ability in subjects with chronic low back pain: results of a randomized controlled pilot study |
| 20 | 2015 | Jay et al. (40) | Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain and stress among laboratory technicians: randomized controlled trial |
| 21 | 2015 | Semrau et al. (65) | Long-term effects of interprofessional biopsychosocial rehabilitation for adults with chronic non-specific low back pain: a multicentre, quasi-experimental study This article also includes supplementary material describing the BPS intervention. |
| 22 | 2016 | Saragiotto et al. (47) | Multidisciplinary biopsychosocial rehabilitation for nonspecific chronic low back pain |
| 23 | 2017 | Booth et al. (57) | Exercise for chronic musculoskeletal pain: a biopsychosocial approach |
| 24 | 2017 | Cabak et al. (58) | Biopsychosocial rehabilitation programme for patients with chronic back pain. Pilot study |
| 25 | 2017 | Iversen et al. (39) | Resistance training in addition to multidisciplinary rehabilitation for patients with chronic pain in the low back: study protocol |
| 26 | 2017 | Motoya et al. (56) | Short-term effect of back school based on cognitive behavioral therapy involving multidisciplinary collaboration |
| 27 | 2017 | Ronzi et al. (46) | Efficiency of three treatment strategies on occupational and quality of life impairments for chronic low back pain patients: is the multidisciplinary approach the key feature to success? |
| 28 | 2017 | Van Erp et al. (68) | Development and content of the biopsychosocial primary care intervention “Back on Track” for a subgroup of people with chronic low back pain |
| 29 | 2018 | Iversen et al. (71) | Resistance band training or general exercise in multidisciplinary rehabilitation of low back pain? A randomized trial |
| 30 | 2018 | Rogers et al. (63) | A 12-h combined physical and psychological treatment programme for patients with persistent back pain |
| 31 | 2018 | Schmidt et al. (25) | The Sano study: justification and detailed description of a multidisciplinary biopsychosocial rehabilitation programme in patients with chronic low back pain This article also includes supplementary material describing the BPS intervention. |
| 32 | 2019 | Ibrahim et al. (38) | Recovering the capability to work among patients with chronic low Back pain after a four-week, multidisciplinary biopsychosocial rehabilitation program: 18-month follow-up study |
| 33 | 2019 | Mas et al. (55) | Effectiveness of a multidisciplinary biopsychosocial intervention for non-specific subacute low back pain in a working population: a cluster randomized clinical trial |
| 34 | 2019 | Thomson et al. (67) | Identifying psychosocial characteristics that predict outcome to the UPLIFT programme for people with persistent back pain: protocol for a prospective cohort study |
| 35 | 2020 | Ampiah et al. (35) | Implementation of a biopsychosocial physiotherapy management approach for patients with non-specific chronic low back pain in Ghana: a study protocol for a mixed-methods, sequential, feasibility, pretest-posttest quasi-experimental study |
| 36 | 2020 | Darnall et al. (73) | Comparative effectiveness of cognitive behavioral therapy for chronic pain and chronic pain self-management within the context of voluntary patient-centered prescription opioid tapering: The EMPOWER Study Protocol |
| 37 | 2020 | Santa Barbara et al. (69) | Descriptive analysis of an interdisciplinary musculoskeletal program |
| 38 | 2021 | Semrau et al. (48) | Effects of behavioral exercise therapy on the effectiveness of multidisciplinary rehabilitation for chronic non-specific low back pain: a randomized controlled trial |
| 39 | 2021 | Skovbo et al. (66) | Description of content, structure and theoretical model of a group-based pain management programme in the treatment of patients with persistent non-specific low back pain and psychological risk factors in a secondary sector setting |
| 40 | 2021 | You et al. (51) | Effectiveness of a multidisciplinary rehabilitation program in real-world patients with chronic back pain: a pilot cohort data analysis |
| 41 | 2022 | Panicker et al. (72) | Evaluation of chronic, noncancer pain management initiative in a multidisciplinary pain clinic |
| 42 | 2022 | Pomarensky et al. (62) | Management of chronic musculoskeletal pain through a biopsychosocial lens |
BPS: biopsychosocial.
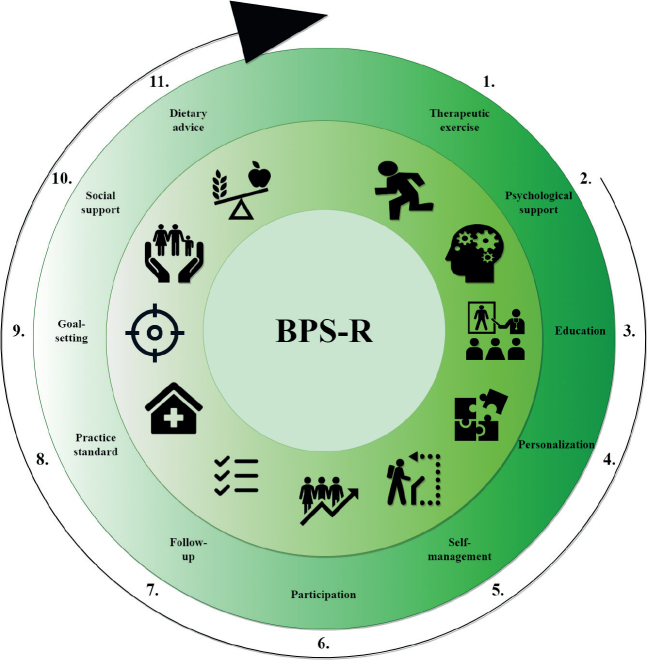
Step 4: attributes
The concept analysis resulted in a total of 11 attributes of a BPS-R intervention programme for CLBP (Fig. 2). Eight of the main attributes include sub-attributes. An overview of the attributes and their corresponding sub-attributes is shown in Table II. Each attribute depicting an essential component of a BPS-R intervention programme in this population is described in detail below.
Fig. 2.
The 11 main attributes of a biopsychosocial rehabilitation (BPS-R) intervention programme for chronic low back pain.
Table II.
Overview of main attributes and sub-attributes
| Main attributes | References with the main attribute (out of 42), n | Sub-attributes | References with the sub-attribute (out of 42), n |
|---|---|---|---|
| 1. Therapeutic exercise | 40 | Exercise | 37 |
| Active approach | 27 | ||
| Reconditioning | 20 | ||
| 2. Psychological support | 38 | Thoughts and behaviors | 27 |
| Psychological counseling | 24 | ||
| Reassuring | 8 | ||
| Positive reinforcement | 5 | ||
| 3. Education | 36 | Educational approach | 35 |
| Detailed information available | 16 | ||
| 4. Personalization | 34 | Individualization/tailoring | 32 |
| Guidance | 15 | ||
| Interdisciplinary communication | 9 | ||
| Patient-centeredness | 6 | ||
| Therapist consistency | 4 | ||
| Graded activity | 4 | ||
| Biofeedback | 2 | ||
| Protocol induced | 2 | ||
| Shared decision making | 2 | ||
| 5. Self-management | 33 | Self-governing | 15 |
| Pain management | 15 | ||
| Managing flare-ups | 9 | ||
| Medication management | 8 | ||
| Self-efficacy | 3 | ||
| Prevention | 3 | ||
| Safety netting | 2 | ||
| 6. Participation | 32 | Implementation in meaningful activities of daily living | 25 |
| Return to work | 19 | ||
| 7. Follow-up | 25 | Re-evaluation | 21 |
| Adherence measures | 9 | ||
| 8. Practice standard | 23 | Expertise | 17 |
| Evidence based | 15 | ||
| Standardization | 10 | ||
| 9. Goal-setting | 20 | None | 20 |
| 10. Social support | 12 | None | 12 |
| 11. Dietary advice | 4 | None | 4 |
Attribute 1: therapeutic exercise. “Therapeutic exercise” is the most identified attribute from this analysis, appearing in 40 of the 42 references. A BPS-R intervention programme for CLBP requires an exercise component, suggesting that the patient is active and cooperates during the intervention. This attribute is characterized by 3 sub-attributes: exercise, an active approach, and reconditioning.
There are 9 exercise modalities mentioned in 37 of the references attributing exercises to a BPS-R intervention programme: strength (23–25, 35–51), endurance (24, 25, 37, 38, 42, 43, 47, 48, 50–52), stretching and mobilizations (23–25, 37, 38, 41–3, 47–49, 53), stability and motor control (23, 25, 38, 41, 49, 50, 53, 54), relaxation exercises (24, 36, 38, 45, 49, 50, 55, 56), postural training (23, 43, 45, 53–55), proprioception (36, 38, 45, 49, 55), lumbopelvic exercises (34, 44, 53), and hydrotherapy (25, 38, 42, 49). Some of the references did not specify the exercise therapy used during the programme (51, 57–68). An active approach appears in 27 of the 42 included references. This sub-attribute includes active participation in rehabilitation, remaining active in leisure time and actively addressing obstacles (23–25, 35, 36, 40, 41, 45, 46, 48, 51–53, 56–57, 60–70). Reconditioning exercises, to improve the cardio-respiratory condition of the patient, are specified in 20 references and have similarities with the first formulated sub-attribute considering the goal of reconditioning can only be achieved via exercise (24, 25, 36–39, 42–44, 46–52, 53, 57, 64, 71).
Attribute 2: psychological support. The second most prevalent attribute consists of 4 sub-attributes that form a cluster called “psychological support”. This attribute implies all the actions taken to aid the patient’s overall mental well-being; it appears in 38 of the 42 included references.
The 4 sub-attributes are thoughts and behaviors (23, 24, 35, 38, 40, 41, 45–53, 55–57, 59, 61, 64–68, 70, 72), psychological counseling (23–25, 36, 39, 41, 42, 44–49, 51–55, 58–61, 70, 72), reassuring the patient (23, 37, 43, 54, 55, 57, 60, 64), and positive reinforcement (54, 57, 62, 65, 66). Thoughts and behaviors are influenced by cognitive behavioral therapy (CBT) and addressing beliefs, behavior, (de-catastrophizing) thoughts, emotions, expectations and preferences to positively influence the patient and rehabilitation. Interventions that affect thoughts and behaviors and those that focus on the psychological state of the patient are both crucial elements to include in a BPS-R intervention programme for CLBP.
Attribute 3: education. “Education” includes actions taken that increase the knowledge of the patient or aim to do so. This attribute appears in 36 of the 42 included references. It consists of 2 sub-attributes: educational approach and detailed information.
Regarding the first sub-attribute, there are several education types in the references. Pain education (23, 25, 37, 40, 50, 57, 61–63, 67, 72, 73), psycho-/CBT education (23, 24, 40, 45, 48, 51, 66, 67), back ergonomics (36, 37, 42, 45), anatomy and physiology (24, 37, 50, 54), and education on the BPS model (38, 49, 50, 65) were taught the most. Other prevalent education topics included education on body awareness (24, 54); re-educating the body-self neuro-matrix (40); giving a booklet (45, 55); lessons on fear avoidance and beliefs (40, 53, 61); risk factors (50, 56, 66, 73); symptom maintenance (56); expectations (64); prevalence and course of disease (65, 73); and activity pacing, management of flare-ups and load-capacity balance (50, 67). Eight references did not report in-depth information on the educational approach (35, 43, 47, 58, 60, 68, 69, 71).
For the second sub-attribute, detailed information was given in 16 of the 42 included references, including tangible information in the form of “the back book” (35, 45, 47), brochures/manuals/pamphlets (25, 58, 65, 69), hand-outs/leaflets (24, 45, 50, 55, 56, 65), other booklets (38, 64, 68, 70, 73) audio/video material (55, 64) and sites/links (64, 65, 73).
Attribute 4: personalization. The attribute “personalization” appears in 34 of the 42 included references and implies the actions taken to adapt a BPS-R intervention programme to the individual. Considering that this attribute is not a straightforward concept, it consists of 9 sub-attributes.
The first and second sub-attributes: individualization/tailoring (23–25, 36–41, 44–46, 48–55, 57, 58, 60–62, 64, 66–69, 71, 72) and guidance (23–25, 38–41, 46, 48, 51, 57, 58, 63, 64, 71), appear the most, in 32 and 15 references, respectively. The other 7 sub-attributes are less prevalent: interdisciplinary communication (23–25, 38, 60, 65, 66, 69, 72), patient-centeredness (24, 25, 57, 64, 65, 72), therapist consistency (24, 48, 55, 65), graded activity (23, 62, 66, 67), biofeedback (23, 54), protocol induced (44, 45), and shared decision-making (50, 61).
Individualization/tailoring is defined as the therapy adaptations to customize the intervention, optimally suiting the patient and context surrounding the patient. Many of the included references did not provide a clear description of content of this individualization and tailoring or how this is achieved. The sub-attribute guidance implies supervision and monitoring of the patient by the therapist. The sub-attribute protocol induced implies that the patient exclusively participates in the intervention and ceases all other therapies. An overarching personalized exercise is described as graded activity (23, 62, 66, 67). This specific type of exercise has overarching modalities, such as endurance and strength. This specific feature allows adaptation of a self-selected activity based on the patient’s goals.
Attribute 5: self-management. “Self-management” refers to the actions taken during rehabilitation to aid the patient to take control of their own life and problems. It appears in 33 of the 42 included references. The 7 sub-attributes that are mentioned the most are, first, self-governing (24, 35, 38, 47, 48, 50–53, 56, 62, 65, 67, 68, 73) and managing pain (23, 25, 37, 40, 41, 43, 44, 47, 52, 56, 58–60, 63, 65), both in 15 references. Self-governing implies the ability of the individual to self-manage the difficulties they encounter. While in managing pain, the patient acquires skills to cope with pain. The remaining 5 sub-attributes are less prevalent: managing flare-ups (36, 45, 48, 51, 63, 65, 67, 69, 70), managing medication intake (23, 25, 55, 59, 63, 66, 72, 73), increasing self-efficacy (62, 66, 73), taking preventative measures (36, 59, 69), and the use of safety netting (35, 65). These sub-attributes are self-explanatory, apart from safety netting, which is defined as the actions instructed by the therapist that allow the patient to recognize deteriorations in the corresponding problem and address them appropriately.
Attribute 6: participation. “Participation” refers to the actions during rehabilitation that aim to facilitate return to work (RTW) and meaningful ADL. The attribute appeared in 32 of the 42 included references and consists of 2 sub-attributes, namely implementation in meaningful ADL (23–25, 35, 36, 38, 39, 41, 45, 47–50, 52–55, 57, 58, 61–63, 65, 67, 68) and RTW (23, 25, 36, 38–44, 47, 49, 52, 60, 61, 64–67), appearing in 25 and 19 references, respectively.
The implementation of meaningful ADL in therapy implies affecting the lifestyle, habits and ergonomics of patients and stimulating implementation of these acquired skills in the long term. RTW focusses on the implementation of therapy with the direct goal of improving work participation and regaining the roles the patient used to fill. This differs between patients and can represent RTW as well as resuming hobbies and reinstating other social roles. Work stimulation exercises (36, 42) can also be seen as a part of this attribute; however, there is overlap with the exercise sub-attribute.
Attribute 7: follow-up. “Follow-up” refers to actions before and after a BPS-R intervention programme to re-evaluate and ensure adherence during the programme. It appears in 25 of the 42 included references and consists of 2 sub-attributes. The first sub-attribute, re-evaluation, appears in 21 references (23–25, 35, 36, 39, 41, 42, 46, 48–51, 56, 58, 60, 68–72). It is defined as the consecutive evaluation of the patient after the first evaluation. The second sub-attribute is adherence measures (24, 25, 38–41, 45, 55, 71), appearing in 9 references. This implies the measures that are taken to enhance the chance of patients adhering to the treatment or study protocol. Examples of actions are distribution of take-home charts (24), development of a detailed plan for the future by the patient (38), offering booster sessions (39) and sending reminder e-mails (41).
Attribute 8: practice standard. “Practice standard” appears in 23 of the 42 included references. It includes 3 sub-attributes: the addition of expertise (appears in 17 of the 42 references), evidence (appears in 15 of the 42 references) and standardization (appears in 10 of the 42 references). Expertise implies that the therapist has received proper training (23–25, 35, 40, 41, 43, 45, 48, 50, 51, 55, 65, 70, 73) or is experienced in the field (23, 35, 39, 45, 66, 73). Evidence-based therapies used in the programme mean that the study was based on practice guidelines or previously executed systematic reviews (25, 35, 39, 44, 55, 67), the general available literature (23, 43, 51, 65, 72, 73) or previous research (24, 41, 70). Finally, there is standardization of the assessment (24, 48), intervention programme (24, 25, 45, 55, 65, 68, 71, 73) or treatment setting (61).
Attribute 9: goal-setting. “Goal-setting” has no sub-attributes. Goal-oriented therapy or goal-setting appears in 20 of the 42 included references as follows: individual/meaningful goals (35, 38, 49, 50, 52, 57, 68), goals negotiated with stakeholders (23), progressive goals (54), goal-oriented therapy (24), setting goals for activities of everyday life (24, 48, 70) and unspecified goals (37, 39, 43, 51, 62, 63, 65, 66).
Attribute 10: social support. “Social support” appears in 12 of the 42 included references and has no sub-attributes. Involving family members (23, 25, 68, 72), stimulating social interaction (40, 45, 66) and focusing on the relation between pain and social competence (48) are ways to include social support in a BPS-R intervention programme. In the remaining references, the social approach is not clearly reported or specified (24, 39, 61, 64).
Attribute 11: dietary advice. “Dietary advice” also has no sub-attributes. It appears in 4 references and includes giving dietary advice (44, 46), dietary counseling (25) or involving nutritionists (48) in the intervention programme.
Step 5: model case
Box I includes the fictional model case of Eric. This case includes the 11 attributes identified by this concept analysis. Hence, this case presents a BPS-R intervention programme. Note that the attributes appear in italics for this model case as well as the borderline and contrary cases.
Box I.
The model case.
Model case: Eric
Eric is a 56-year-old mechanic working for a large industrial company. Nine years ago, he was in a car accident. He did not sustain any major trauma, except for the pain is his back that he thought would resolve in time. However, the pain never really decreased, and Eric tried to continue his job but occasionally had to call in sick and eventually even quit his job. At the request of his partner, Eric consulted his general practitioner, who referred him to a multidisciplinary practice specialized in working with people suffering from chronic low back pain using the latest evidence (attribute 8: practice standard). After broad history taking together with his wife (attribute 10: social support) and initial assessment of Eric’s biopsychosocial status, he cooperated with the multiple disciplines to identify, set and work towards goals that are relevant to him. A physiotherapist, occupational therapist, psychologist and dietician collaborated on improving Eric’s situation and reaching his personal goals (attribute 9: goal-setting). The therapy focused on the capacities of Eric (attribute 4: personalization) and the requirements of his job, hobbies and activities of daily living. Eric began to understand the mechanisms behind his symptoms due to the education (attribute 3: education) he received from the different professionals and gained insight into how to manage his symptoms. His thoughts and behaviors were rationalized (attribute 2: psychological support) and he got to express his feelings towards himself and his family. The frequency of therapy decreased (attribute 7: follow-up) from 3 times a week to once every 2 weeks. When his disability and pain were at a reasonable level for Eric, task-specific activities (attribute 1: therapeutic exercise) were included in his rehabilitation programme to optimize return to work at his former job. Eric started hiking again with his wife and 2 daughters and maintained a healthy diet (attribute 11: dietary advice). Therapy focused on work-related tasks and tasks he had to perform at home (attribute 6: participation), like gardening. He returned to his former workplace and terminated the follow-up at the practice as he was confident he could now manage the problem on his own (attribute 5: self-management).
Step 6: additional cases
The borderline and contrary cases are shown in Boxes II and III, respectively. The borderline case, describing the story of Lily, contains some but not all of the formulated attributes. In contrast to the model case of Eric, the contrary case, covering Glen’s story, does not contain any of the attributes.
Box II.
The borderline case.
Borderline case: Lily
Lily is 32 years old and works in a local bakery. She recently moved in with her boyfriend. She had suffered from low back pain for the past 2 years and had undergone one operation to remove a herniated disc. Her back pain is still interfering with her job, hobbies and social life. She visits a physiotherapist once a week to exercise (attribute 1: therapeutic exercise) and strengthen her back. She tries to eat healthily (attribute 11: dietary advice) and increase her activity levels by jogging, swimming or cycling with a friend (attribute 10: social support) 2 times a week. She is very competitive and continues to set new goals (attribute 9: goal-setting) for herself. At work, her employer tries to be understanding and even optimized the working area (attribute 6: participation) for her and the other employees. An ergonomic specialist came to educate (attribute 3: education) the employees on ergonomics in the workplace. To manage her stress, Lily talks to a psychologist (attribute 2: psychological support) once a month. She would like to visit the psychologist together with her boyfriend, but he does not believe it will affect their situation.
Box III.
The contrary case.
Contrary case: Glen
Glen is 42 years old and has suffered from low back pain since he turned 30. When asked about the origin of the problem, he believes it originated from his bad posture and active job. According to Glen, back pain runs in the family, so it will never improve. He does not like hospitals or doctors or asking for help. When he is in severe pain, he rests and takes pain medication until the pain normalizes again. He has pain all the time but continues to work at the public library. Once every week he goes to a massage salon to relax his back and recharge after an exhausting working week.
Step 7: antecedents and consequences
Antecedents. In this concept analysis, there was 1 antecedent at the patient level (i.e. motivation), 1 at the professional level (i.e. a multidisciplinary team) and 1 at the interplay between both levels (i.e. preparedness). A BPS-R intervention programme focusing on the aspects of the individual requires a diligent and motivated patient. The references included in this concept analysis focus on the active part the patient plays in their rehabilitation, with or without passive interventions. The second antecedent formulated in this concept analysis is the existence of a multidisciplinary team. Multiple healthcare providers and/or disciplines are mentioned in the references, including physicians, physiotherapists, occupational therapist, dieticians and psychologists, among others. To treat all dimensions of the patient, professionals of all disciplines are required to successfully complete the intervention. The third and final antecedent is preparedness. This implies that the therapist, as well as the patient, need to be prepared to go the extra mile in rehabilitation. When 1 of both parties is not prepared to put in the work, success cannot be achieved.
Consequences. Consequences are defined as the elements occurring after the concept and are therefore the result of a BPS-R intervention programme. The included references contain many consequences, including biological, psychological and social outcomes. A decrease in pain (23, 36–38, 40, 42, 43, 47, 51, 53, 55, 59–61, 70, 72) and disability (37, 38, 42, 44, 47, 53, 56, 57, 58, 60, 63, 69–71) and an increase in function (36, 38, 42, 43, 46, 48, 57, 58, 61, 65, 69) and RTW/work status (23, 42, 43, 49, 60) are the most reported. Other reported consequences of the intervention are decreased pain medication (23, 71); kinesiophobia and fear avoidance (36, 53, 56); sick-leave (44, 52, 60); depression and anxiety (38, 51, 70); catastrophizing (51, 53, 56); fatigue (51); and increased mood (23), knowledge (36), movement behavior/activity (36, 48), self-rated health (60), physical outcomes (43, 43, 53), pain self-efficacy (63, 70), quality of life (38, 46, 53, 57, 61), workability (38, 47, 49), social ability/role/condition (46, 51, 58) and self-management (48). Two of the consequences are also an attribute and a sub-attribute: self-management is attribute 5 and self-efficacy is a sub-attribute of self-management.
Step 8: empirical referents
There are no empirical referents mentioned in the included references to measure the entire concept of a BPS-R intervention programme. Hence, examples of assessment tools for the individual attributes were gathered (Table III). This subdivision may facilitate a future empirical referent that covers the concept as a whole. In Table III, there are 1 or 2 empirical referents for each attribute, but this list is not exhaustive: other assessment tools could also be considered appropriate for certain attributes. Note that in a recent concept analysis on self-management, the authors formulated attributes and proposed assessment tools by using the same methodology (74).
Table III.
Empirical referents identified for each attribute
| Attribute | Empirical referent |
|---|---|
| 1. Therapeutic exercise | International Physical Activity Questionnaire (IPAQ) (91) Wearables (92) |
| 2. Psychological support | Patient Health Questionnaire (PHQ) (93) |
| 3. Education | Neurophysiology of Pain Questionnaire (NPQ) (94) |
| 4. Personalization | Patient Participation in Rehabilitation Questionnaire (PPRQ) (95) |
| 5. Self-management | Self-Management Ability Scale-30 (SMAS-30) (96) Self-Management Behavior Questionnaire (SMBQ) (97) |
| 6. Participation | Ghent Participation Scale (98) Impact on participation and autonomy (99) |
| 7. Follow-up (re-evaluation and adherence measures) | ROB2 tool: sections 2.5 and 3.3 (100) Treatment Adherence Perception Questionnaire, TAPQ (101) |
| 8. Practice standard (expertise, evidence-based, standardization) | ROB2 tool (100) |
| 9. Goal-setting | Patient Goal Priority Questionnaire (PGPQ) (102) Goal attainment scale (103) |
| 10. Social support | Medical Outcome Study (MOS) – social support study (104) |
| 11. Dietary advice | Diet History Questionnaire (DHQ) (105) |
DISCUSSION
The aim of this concept analysis was to identify the essential attributes of a BPS-R intervention programme for the working population with CLBP according to the methodology formulated by Walker and Avant (30). After collecting the evidence from the 42 included references, there were 11 attributes, 3 cases, antecedents, consequences and empirical referents to conceptualize a BPS-R intervention programme for CLBP.
According to a recent systematic review of guidelines, investigating the evidence-based treatment for neck pain and LBP across Europe, education, exercise therapy, behavior-oriented treatment, RTW programmes and multidisciplinary cooperation are prescribed as appropriate conservative treatment modalities (75). Moreover, the authors recommended a multidisciplinary approach for specific subgroups; for example, highly motivated patients with CLBP (75). These findings are in line with the 2017 KCE guideline, which describes evaluation and management of acute LBP, CLBP and radicular pain and fit well within the increasing use and implementation of the ICF for rehabilitation delivery (11). Similarly, a British Journal of Sports Medicine editorial emphasized the importance of exercise, psychosocial factors and education, confirming the concept analysis in the current study (76). This concept analysis describes the education modalities in detail, showing that the currently used education in BPS-R intervention programmes in the recent literature is often more comprehensive. Likewise, exercise therapy, behavior-oriented therapy and RTW also feature in attributes 1, 2 and 6. Lastly, multidisciplinary cooperation also appears as an antecedent for BPS-R intervention programmes and is mentioned in the guidelines.
Motor control training for LBP has been covered in a recent article; the authors suggested sub-grouping to allow for more personalized treatment (77). Identification of individual factors on a biopsychosocial level serves as a basis for personalized spine care and underscores the importance of personalization in rehabilitation (78, 79). In addition, a study on the perceptions of physiotherapists towards CLBP management from a BPS perspective described the struggles of healthcare providers (physiotherapists in this case). Ultimately, the authors determined that the key objective is patient self-management (80).
The follow-up attribute, which comprises re-evaluating the patient’s situation and including adherence measures in the study protocol, and the practice standard attribute (expertise, evidence-based and standardization) are part of good clinical practice and should be incorporated in all valuable BPS-R intervention programmes. More importantly, the goal-setting attribute is inherently personalized and shares common ground with the personalization and self-management attributes. Furthermore, goal-setting is used in rehabilitation to facilitate self-management and is highly dependent on the therapist’s beliefs and attitudes (81). Likewise, graded activity is included under the attribute personalization and could also been seen as a part of the first attribute when considering this is an exercise modality to increase activity levels. In this concept analysis, it is included in attribute 4 (personalization) due to the specific instructions to personalize this type of exercise to the individual.
Apart from biological and psychological considerations, social aspects of the patient are often neglected when administering a BPS-R intervention programme for CLBP (28). Of note, researchers recently identified 14 psychosocial determinants related to the length of sick-leave, indicating the relevance for inclusion in rehabilitation (82). The neglect of social aspects is also apparent in the results: only 12 of the included references mentioned the attribute social support. Finally, only 4 of the included references mentioned the attribute dietary advice. Certain nutritional interventions with or without physical therapy reduce pain and improve outcomes regarding daily activities in patients with CLBP and other chronic pathologies (83–85). Therefore, dietary advice may play a role in addressing CLBP even though it has not been described frequently in the current literature.
While empirical referents have been proposed for each attribute (Table III), this list is not exhaustive. Other tools may also be appropriate to objectify the attributes. An assessment tool to measure the entire concept of a BPS-R intervention programme has not yet been developed. However, there is the “BPS scale” that can reliably and validly measure the BPS competencies of healthcare providers (86).
Based on the available evidence, the antecedents motivation and preparedness may seem trivial, but they are vital for completing a successful rehabilitation. Moreover, a multidisciplinary care approach, implying the use of a multidisciplinary team, is warranted for patients with CLBP (78). The progression from multidisciplinary to inter- and transdisciplinary rehabilitation is worth mentioning and should be included in future research considering that the current concept analysis only considered multidisciplinary care (87).
Finally, the results of this concept analysis show a good fit with the most recent definition of rehabilitation (16). The attributes that emerged from this concept analysis create opportunities to operationalize the definition of rehabilitation into intervention programmes.
Strengths and limitations
A major strength of this concept analysis is that no prior study had identified the critical attributes included in a BPS-R intervention programme for the working population with CLBP. In a recent study of the evidence-based interventions to treat CLBP, the authors proposed multidisciplinary care as an effective approach, but it was not incorporated in the future clinical trial because of the complexity and the high level of care coordination (27). Another reason for conflicting, missing and ambiguous results from the literature can be found in a recent critical review that highlighted the absence of multiple important factors (interpersonal or institutional power relations, and cultural, ethical and social health aspects) of the BPS model in physiotherapeutic research on LBP. In addition, conceptualization of the BPS model in physiotherapy is absent in both the literature and practice (28). A second strength of this concept analysis is the systematic formulation of the attributes, antecedents and consequences together with illustrative cases and assessment tools. This could be highly valuable to underpin or improve future research investigating the effectiveness or other aspects of a BPS-R intervention programme.
There are some limitations to this concept analysis. The first is the absence of a quality assessment covering the included references. In general, a risk of bias assessment is not an integral part of a concept analysis. In addition, a typical feature of a concept analysis is to include all retrieved references to obtain a complete view of the available literature. Due to the variety of reference types that were collected through the concept analysis methodology, no risk of bias assessment was performed, hence caution is warranted when interpreting the results. As a second limitation, the search was limited to the time period from 2010 until November 2022. By starting the search from 2010, some older, high-quality evidence for the concept may have been missed. The authors decided to start the search by going back 10 years (the design of this study commenced in 2020 and included literature until 2022) to incorporate recent evidence regarding BPS-R intervention programmes, and thus improve the relevance to current healthcare and applicability for the future (88). Thirdly, spiritual care has been added as the fourth dimension in the BPS model as a way to stimulate hope and improve mental and physical health in patients with chronic pain (89). Considering the scarcity of evidence and inconclusiveness, spiritual aspects were not included in this concept analysis. Recently, objectification of the spiritual dimension has been performed with the Spiritual Distress and Resources Questionnaire, which is a valid and reliable screening tool; thus, this aspect could be considered in future research (90). Lastly, the objective of this concept analysis was to categorize findings that are connected to each other; thus, categorization was difficult and discussion was inevitable. The decisions were made after thorough discussion between the authors until agreement was reached.
Recommendations
Considering the limitations of this concept analysis, future research should try to objectify the concept of a BPS-R intervention programme to facilitate assessment and comparison between studies. Although personalization is one of the core attributes of BPS-R intervention programmes for patients with CLBP, a certain degree of standardization should be applied when developing these programmes. There should be a minimal set of attributes present to label a programme a BPS-R intervention. Furthermore, personalization could be a concept in and of itself considering its many contextual factors and complexity. However, the exact operationalization of this concept into a BPS-R intervention programme still needs to be determined. In addition, this concept analysis might stimulate further research dissecting this topic and contribute to conceptualization, which is required based on previous research (28). The attributes formulated in this article offer guidance in developing and applying BPS-R intervention programmes in future research.
Follow-up research is already ongoing by means of an international multi-stage Delphi study to build a checklist based on the attributes, antecedents and consequences, and to clarify the content and the operationalization of the attributes such as personalization, as discussed above. This additional step is considered necessary to validate and increase the credibility of the findings and to provide an international consensus. After validation and a general consensus, the tool can be used in future research or practise.
In conclusion, the effectiveness of a BPS-R intervention programme in people with CLBP has been thoroughly investigated, but the lack of conceptualization hampers its integration into clinical practice and research. The aim of this concept analysis was to showcase the attributes of a BPS-R intervention programme for CLBP. Using the methodology described by Walker and Avant (30), we defined 11 attributes, 3 cases, antecedents, consequences and empirical referents to break down, clarify and measure this concept. There should be further incorporation of this concept as well as exploration of the objectification of the entire concept and conceptualization on how to personalize treatment.
Supplementary Material
BIOPSYCHOSOCIAL REHABILITATION IN THE WORKING POPULATION WITH CHRONIC LOW BACK PAIN: A CONCEPT ANALYSIS
ACKNOWLEDGEMENTS
Conflict of interest
Lisa Goudman is a postdoctoral research fellow funded by the Research Foundation Flanders (FWO), Belgium (project number 12ZF622N). Dries Ceulemans, Olivia Lavreysen and Jonas Callens are PhD students working on a project funded by the Research Foundation Flanders (FWO-TBM project number T000821N). Maarten Moens has received speaking fees from Medtronic, Nevro and Saluda Medical. The STIMULUS research group received independent research grants from Medtronic.
Funding Statement
Lisa Goudman is a postdoctoral research fellow funded by the Research Foundation Flanders (FWO), Belgium (project number 12ZF622N). Dries Ceulemans, Olivia Lavreysen and Jonas Callens are PhD students working on a project funded by the Research Foundation Flanders (FWO-TBM project number T000821N). Maarten Moens has received speaking fees from Medtronic, Nevro and Saluda Medical. The STIMULUS research group received independent research grants from Medtronic.
REFERENCES
- 1.Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, et al. What low back pain is and why we need to pay attention. Lancet 2018; 391: 2356–2367. DOI: 10.1016/S0140-6736(18)30480-X [DOI] [PubMed] [Google Scholar]
- 2.Wu A, March L, Zheng X, Huang J, Wang X, Zhao J, et al. Global low back pain prevalence and years lived with disability from 1990 to 2017: estimates from the Global Burden of Disease Study 2017. Ann Transl Med 2020; 8: 299. DOI: 10.21037/atm.2020.02.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Treede R-D, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, et al. A classification of chronic pain for ICD-11. Pain 2015; 156: 1003–1007. DOI: 10.1097/j.pain.0000000000000160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang H, Haldeman S, Lu M-L, Baker D. Low back pain prevalence and related workplace psychosocial risk factors: a study using data from the 2010 National Health Interview Survey. J Manipulative Physiol Ther 2016; 39: 459–472. DOI: 10.1016/j.jmpt.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jegan NRA, Brugger M, Viniol A, Strauch K, Barth J, Baum E, et al. Psychological risk and protective factors for disability in chronic low back pain – a longitudinal analysis in primary care. BMC Musculoskelet Disord 2017; 18: 114. DOI: 10.1186/s12891-017-1482-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stewart Williams J, Ng N, Peltzer K, Yawson A, Biritwum R, Maximova T, et al. Risk factors and disability associated with low back pain in older adults in low- and middle-income countries. Results from the WHO Study on Global AGEing and Adult Health (SAGE). PLoS One 2015; 10: e0127880. DOI: 10.1371/journal.pone.0127880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alonso-García M, Sarría-Santamera A. The economic and social burden of low back pain in spain: a national assessment of the economic and social impact of low back pain in spain. Spine 2020; 45: E1026–E1032. DOI: 10.1097/BRS.0000000000003476 [DOI] [PubMed] [Google Scholar]
- 8.Stucki G, Bickenbach J. 1.1 Basic concepts, definitions and models. J Int Soc Phys Rehabil Med 2019; 2: S8. DOI: 10.4103/jisprm.jisprm_5_19 [DOI] [Google Scholar]
- 9.Kusnanto H, Agustian D, Hilmanto D. Biopsychosocial model of illnesses in primary care: a hermeneutic literature review. J Family Med Prim Care 2018; 7: 497–500. DOI: 10.4103/jfmpc.jfmpc_145_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ustün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disabil Rehabil 2003; 25: 565–571. DOI: 10.1080/0963828031000137063 [DOI] [PubMed] [Google Scholar]
- 11.Wambeke PV, Leuven U. Low back pain and radicular pain: assessment and management. 2017. [accessed 2023 April 1]. Available from: https://kce.fgov.be/sites/default/files/2021-11/KCE_287_Low_back_pain_Report.pdf.
- 12.Koes BW, van Tulder M, Lin C-WC, Macedo LG, McAuley J, Maher C. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 2010; 19: 2075–2094. DOI: 10.1007/s00586-010-1502-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nicol V, Verdaguer C, Daste C, Bisseriex H, Lapeyre É, Lefèvre-Colau M-M, et al. Chronic low back pain: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med 2023; 12: 1685. DOI: 10.3390/jcm12041685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Connell NE, Cook CE, Wand BM, Ward SP. Clinical guidelines for low back pain: a critical review of consensus and inconsistencies across three major guidelines. Best Pract Res Clin Rheumatol 2016; 30: 968–980. DOI: 10.1016/j.berh.2017.05.001 [DOI] [PubMed] [Google Scholar]
- 15.Foster NE, Anema JR, Cherkin D, Chou R, Cohen SP, Gross DP, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. Lancet 2018; 391: 2368–2383. DOI: 10.1016/S0140-6736(18)30489-6 [DOI] [PubMed] [Google Scholar]
- 16.Negrini S, Selb M, Kiekens C, Todhunter-Brown A, Arienti C, Stucki G, et al. Rehabilitation definition for research purposes. A global stakeholders’ initiative by Cochrane Rehabilitation. Eur J Phys Rehabil Med 2022; 58: 333–341. DOI: 10.23736/S1973-9087.22.07509-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.admin-kce . Care for people living with chronic conditions. For a Healthy Belgium. 2023. [cited 2023 April 1]. Available from: https://www.healthybelgium.be/en/health-system-performance-assessment/specific-domains/chronic-care2.
- 18.Bernaers L, Cnockaert E, Braeckman L, Mairiaux P, Willems TM. Disability and return to work after a multidisciplinary intervention for (sub)acute low back pain: a systematic review. Clin Rehabil 2023; 37: 964–974. DOI: 10.1177/02692155221146447 [DOI] [PubMed] [Google Scholar]
- 19.Hajat C, Stein E. The global burden of multiple chronic conditions: a narrative review. Prev Med Rep 2018; 12: 284–293. DOI: 10.1016/j.pmedr.2018.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJEM, Ostelo RWJG, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain: Cochrane systematic review and meta-analysis. BMJ 2015; 350: h444. DOI: 10.1136/bmj.h444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marin TJ, Van Eerd D, Irvin E, Couban R, Koes BW, Malmivaara A, et al. Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Cochrane Database Syst Rev 2017; 6: CD002193. DOI: 10.1002/14651858.CD002193.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ochsenkuehn FR, Crispin A, Weigl MB. Chronic low back pain: a prospective study with 4 to 15 years follow-up after a multidisciplinary biopsychosocial rehabilitation program. BMC Musculoskelet Disord 2022; 23: 977. DOI: 10.1186/s12891-022-05963-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bosy D, Etlin D, Corey D, Lee JW. An interdisciplinary pain rehabilitation programme: description and evaluation of outcomes. Physiother Can 2010; 62: 316–326. DOI: 10.3138/physio.62.4.316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hofmann J, Peters S, Geidl W, Hentschke C, Pfeifer K. Effects of behavioral exercise therapy on the effectiveness of a multidisciplinary rehabilitation for chronic non-specific low back pain: study protocol for a randomised controlled trial. BMC Musculoskelet Disord 2013; 14: 89. DOI: 10.1186/1471-2474-14-89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schmidt AM, Terkildsen Maindal H, Laurberg TB, Schiøttz-Christensen B, Ibsen C, Bak Gulstad K, et al. The Sano study: justification and detailed description of a multidisciplinary biopsychosocial rehabilitation programme in patients with chronic low back pain. Clin Rehabil 2018; 32: 1431–1439. DOI: 10.1177/0269215518780953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Knezevic NN, Candido KD, Vlaeyen JWS, Van Zundert J, Cohen SP. Low back pain. Lancet 2021; 398: 78–92. DOI: 10.1016/S0140-6736(21)00733-9 [DOI] [PubMed] [Google Scholar]
- 27.Mauck MC, Aylward AF, Barton CE, Birckhead B, Carey T, Dalton DM, et al. Evidence-based interventions to treat chronic low back pain: treatment selection for a personalized medicine approach. Pain Rep 2022; 7: e1019. DOI: 10.1097/PR9.0000000000001019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mescouto K, Olson RE, Hodges PW, Setchell J. A critical review of the biopsychosocial model of low back pain care: time for a new approach? Disabil Rehabil 2022; 44: 3270–3284. DOI: 10.1080/09638288.2020.1851783 [DOI] [PubMed] [Google Scholar]
- 29.Schiller CJ. Teaching concept analysis to graduate nursing students. Nurs Forum 2018; 53: 248–254. DOI: 10.1111/nuf.12233 [DOI] [PubMed] [Google Scholar]
- 30.Walker L, Avant K. Strategies for theory construction in nursing. 5th ed. Edinburgh: Pearson; 2014. [Google Scholar]
- 31.Wilson, J. Thinking with concepts. New York, NY: Cambridge University Press; 1963. [Google Scholar]
- 32.World Health Organization . ICD-11: International Classification of Diseases 11th Revision. [cited 2023 April 1]. Available from: https://icd.who.int/en
- 33.The essential concepts of nursing Cutcliffe John R McKenna Hugh the essential concepts of nursing 368 Elsevier 9780443073724 0443073724. Nurs Stand 2006; 20(28): 36. DOI: 10.7748/ns2006.03.20.28.36.b444 [DOI] [PubMed] [Google Scholar]
- 34.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174. [PubMed] [Google Scholar]
- 35.Ampiah PK, Hendrick P, Moffatt F. Implementation of a biopsychosocial physiotherapy management approach for patients with non-specific chronic low back pain in Ghana: a study protocol for a mixed-methods, sequential, feasibility, pretest-posttest quasi-experimental study. Phys Ther Rev 2021; 26: 109–123. DOI: 10.1080/10833196.2020.1832721 [DOI] [Google Scholar]
- 36.Demoulin C, Grosdent S, Capron L, Tomasella M, Somville P-R, Crielaard J-M, et al. Effectiveness of a semi-intensive multidisciplinary outpatient rehabilitation program in chronic low back pain. Joint Bone Spine 2010; 77: 58–63. DOI: 10.1016/j.jbspin.2009.11.003 [DOI] [PubMed] [Google Scholar]
- 37.Dufour N, Thamsborg G, Oefeldt A, Lundsgaard C, Stender S. Treatment of chronic low back pain: a randomized, clinical trial comparing group-based multidisciplinary biopsychosocial rehabilitation and intensive individual therapist-assisted back muscle strengthening exercises. Spine 2010; 35: 469–476. DOI: 10.1097/BRS.0b013e3181b8db2e [DOI] [PubMed] [Google Scholar]
- 38.Ibrahim ME, Weber K, Courvoisier DS, Genevay S. Recovering the capability to work among patients with chronic low Back pain after a four-week, multidisciplinary biopsychosocial rehabilitation program: 18-month follow-up study. BMC Musculoskelet Disord 2019; 20: 439. DOI: 10.1186/s12891-019-2831-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Iversen VM, Vasseljen O, Mork PJ, Berthelsen IR, Børke J-BB, Berheussen GF, et al. Resistance training in addition to multidisciplinary rehabilitation for patients with chronic pain in the low back: study protocol. Contemp Clin Trials Commun 2017; 6: 115–121. DOI: 10.1016/j.conctc.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jay K, Brandt M, Hansen K, Sundstrup E, Jakobsen MD, Schraefel MC, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain and stress among laboratory technicians: randomized controlled trial. Pain Physician 2015; 18: 459–471. [PubMed] [Google Scholar]
- 41.Jay K, Brandt M, Sundstrup E, Schraefel M, Jakobsen MD, Sjøgaard G, et al. Effect of individually tailored biopsychosocial workplace interventions on chronic musculoskeletal pain, stress and work ability among laboratory technicians: randomized controlled trial protocol. BMC Musculoskelet Disord 2014; 15: 444. DOI: 10.1186/1471-2474-15-444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Luk KDK, Wan TWM, Wong YW, Cheung KMC, Chan KYK, Cheng ACS, et al. A multidisciplinary rehabilitation programme for patients with chronic low back pain: a prospective study. J Orthop Surg 2010; 18: 131–138. DOI: 10.1177/230949901001800201 [DOI] [PubMed] [Google Scholar]
- 43.Nazzal ME, Saadah MA, Saadah LM, Al-Omari MA, Al-Oudat ZA, Nazzal MS, et al. Management options of chronic low back pain. A randomized blinded clinical trial. Neurosciences 2013; 18: 152–159. [PubMed] [Google Scholar]
- 44.Roche-Leboucher G, Petit-Lemanac’h A, Bontoux L, Dubus-Bausière V, Parot-Shinkel E, Fanello S, et al. Multidisciplinary intensive functional restoration versus outpatient active physiotherapy in chronic low back pain: a randomized controlled trial. Spine 2011; 36: 2235–2242. DOI: 10.1097/BRS.0b013e3182191e13 [DOI] [PubMed] [Google Scholar]
- 45.Rodriguez-Blanco T, Fernández-San-Martin I, Balagué-Corbella M, Berenguera A, Moix J, Montiel-Morillo E, et al. Study protocol of effectiveness of a biopsychosocial multidisciplinary intervention in the evolution of non-specific sub-acute low back pain in the working population: cluster randomised trial. BMC Health Serv Res 2010; 10: 12. DOI: 10.1186/1472-6963-10-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ronzi Y, Roche-Leboucher G, Bègue C, Dubus V, Bontoux L, Roquelaure Y, et al. Efficiency of three treatment strategies on occupational and quality of life impairments for chronic low back pain patients: is the multidisciplinary approach the key feature to success? Clin Rehabil 2017; 31: 1364–1373. DOI: 10.1177/0269215517691086 [DOI] [PubMed] [Google Scholar]
- 47.Saragiotto BT, de Almeida MO, Yamato TP, Maher CG. Multidisciplinary biopsychosocial rehabilitation for nonspecific chronic low back pain. Phys Ther 2016; 96: 759–763. DOI: 10.2522/ptj.20150359 [DOI] [PubMed] [Google Scholar]
- 48.Semrau J, Hentschke C, Peters S, Pfeifer K. Effects of behavioral exercise therapy on the effectiveness of multidisciplinary rehabilitation for chronic non-specific low back pain: a randomised controlled trial. BMC Musculoskelet Disord 2021; 22: 500. DOI: 10.1186/s12891-021-04353-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Steiner A-S, Sartori M, Leal S, Kupper D, Gallice J-P, Rentsch D, et al. Added value of an intensive multidisciplinary functional rehabilitation programme for chronic low back pain patients. Swiss Med Wkly 2013; 143: w13763. DOI: 10.4414/smw.2013.13763 [DOI] [PubMed] [Google Scholar]
- 50.Verkerk K, Luijsterburg PAJ, Ronchetti I, Miedema HS, Pool-Goudzwaard A, van Wingerden J-P, et al. Course and prognosis of recovery for chronic non-specific low back pain: design, therapy program and baseline data of a prospective cohort study. BMC Musculoskelet Disord 2011; 12: 252. DOI: 10.1186/1471-2474-12-252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.You DS, Ziadni MS, Cooley CE, Talavera DC, Mackey SC, Poupore-King H. Effectiveness of a multidisciplinary rehabilitation program in real-world patients with chronic back pain: a pilot cohort data analysis. J Back Musculoskelet Rehabil 2021; 34: 965–973. DOI: 10.3233/BMR-200305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bergström C, Jensen I, Hagberg J, Busch H, Bergström G. Effectiveness of different interventions using a psychosocial subgroup assignment in chronic neck and back pain patients: a 10-year follow-up. Disabil Rehabil 2012; 34: 110–118. DOI: 10.3109/09638288.2011.607218 [DOI] [PubMed] [Google Scholar]
- 53.Monticone M, Ambrosini E, Rocca B, Magni S, Brivio F, Ferrante S. A multidisciplinary rehabilitation programme improves disability, kinesiophobia and walking ability in subjects with chronic low back pain: results of a randomised controlled pilot study. Eur Spine J 2014; 23: 2105–2113. DOI: 10.1007/s00586-014-3478-5 [DOI] [PubMed] [Google Scholar]
- 54.Giaquinto S, Bruti L, Dall’Armi V, Gison A, Palma E. A bio-psycho-social approach for treating sub-acute low back pain. Disabil Rehabil 2010; 32: 1966–1971. DOI: 10.3109/09638281003797349 [DOI] [PubMed] [Google Scholar]
- 55.Mas RR, López-Jiménez T, Pujol-Ribera E, Martín MIF-S, Moix-Queraltó J, Montiel-Morillo E, et al. Effectiveness of a multidisciplinary BIOPSYCHOSOCIAL intervention for non-specific SUBACUTE low back pain in a working population: a cluster randomized clinical trial. BMC Health Serv Res 2019; 19: 962. DOI: 10.1186/s12913-019-4810-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Motoya R, Otani K, Nikaido T, Ono Y, Matsumoto T, Yamagishi R, et al. Short-term effect of back school based on cognitive behavioral therapy involving multidisciplinary collaboration. Fukushima J Med Sci 2017; 63: 81–89. DOI: 10.5387/fms.2016-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Booth J, Moseley GL, Schiltenwolf M, Cashin A, Davies M, Hübscher M. Exercise for chronic musculoskeletal pain: a biopsychosocial approach. Musculoskeletal Care 2017; 15: 413–421. DOI: 10.1002/msc.1191 [DOI] [PubMed] [Google Scholar]
- 58.Cabak A, Rudnicka A, Kulej L, Tomaszewski W. Biopsychosocial Rehabilitation Programme for Patients with Chronic Back Pain. Pilot Study. Ortop Traumatol Rehabil 2017; 19: 165–174. DOI: 10.5604/15093492.1238033 [DOI] [PubMed] [Google Scholar]
- 59.Hussain A, Erdek M. Interventional pain management for failed back surgery syndrome. Pain Pract 2014; 14: 64–78. DOI: 10.1111/papr.12035 [DOI] [PubMed] [Google Scholar]
- 60.Jensen C, Jensen OK, Christiansen DH, Nielsen CV. One-year follow-up in employees sick-listed because of low back pain: randomized clinical trial comparing multidisciplinary and brief intervention. Spine 2011; 36: 1180–1189. DOI: 10.1097/BRS.0b013e3181eba711 [DOI] [PubMed] [Google Scholar]
- 61.Moradi B, Hagmann S, Zahlten-Hinguranage A, Caldeira F, Putz C, Rosshirt N, et al. Efficacy of multidisciplinary treatment for patients with chronic low back pain: a prospective clinical study in 395 patients. J Clin Rheumatol 2012; 18: 76–82. DOI: 10.1097/RHU.0b013e318247b96a [DOI] [PubMed] [Google Scholar]
- 62.Pomarensky M, Macedo L, Carlesso LC. Management of Chronic Musculoskeletal Pain Through a Biopsychosocial Lens. J Athl Train 2022; 57: 312–318. DOI: 10.4085/1062-6050-0521.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rogers D, Nightingale P, Gardner A. A 12-h combined physical and psychological treatment programme for patients with persistent back pain. Musculoskeletal Care 2018; 16: 318–321. DOI: 10.1002/msc.1235 [DOI] [PubMed] [Google Scholar]
- 64.Rozenberg S, Foltz V, Fautrel B. Treatment strategy for chronic low back pain. Joint Bone Spine 2012; 79: 555–559. DOI: 10.1016/j.jbspin.2012.09.003 [DOI] [PubMed] [Google Scholar]
- 65.Semrau J, Hentschke C, Buchmann J, Meng K, Vogel H, Faller H, et al. Long-term effects of interprofessional biopsychosocial rehabilitation for adults with chronic non-specific low back pain: a multicentre, quasi-experimental study. PLoS One 2015; 10: e0118609. DOI: 10.1371/journal.pone.0118609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Skovbo MH, Agerbo K, Jakobsen A, Clausen SA, Langagergaard V, Rolving N. Description of content, structure and theoretical model of a group-based pain management programme in the treatment of patients with persistent non-specific low back pain and psychological risk factors in a secondary sector setting. Clin Rehabil 2021; 35: 1077–1088. DOI: 10.1177/0269215521995185 [DOI] [PubMed] [Google Scholar]
- 67.Thomson H, Evans K, Dearness J, Kelley J, Conway K, Morris C, et al. Identifying psychosocial characteristics that predict outcome to the UPLIFT programme for people with persistent back pain: protocol for a prospective cohort study. BMJ Open 2019; 9: e028747. DOI: 10.1136/bmjopen-2018-028747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.van Erp RMA, Huijnen IPJ, Köke AJA, Abbink FE, den Hollander M, Smeets RJEM. Development and content of the biopsychosocial primary care intervention “Back on Track” for a subgroup of people with chronic low back pain. Physiotherapy 2017; 103: 160–166. DOI: 10.1016/j.physio.2016.04.004 [DOI] [PubMed] [Google Scholar]
- 69.Santa Barbara MT, Cortazzo M, Emerick T, Furnier J, Duff J, Shapiro S, et al. Descriptive analysis of an interdisciplinary musculoskeletal program. PM R 2020; 12: 639–646. DOI: 10.1002/pmrj.12288 [DOI] [PubMed] [Google Scholar]
- 70.Wetherell JL, Afari N, Rutledge T, Sorrell JT, Stoddard JA, Petkus AJ, et al. A randomized, controlled trial of acceptance and commitment therapy and cognitive-behavioral therapy for chronic pain. Pain 2011; 152: 2098–2107. DOI: 10.1016/j.pain.2011.05.016 [DOI] [PubMed] [Google Scholar]
- 71.Iversen VM, Vasseljen O, Mork PJ, Gismervik S, Bertheussen GF, Salvesen Ø, et al. Resistance band training or general exercise in multidisciplinary rehabilitation of low back pain? A randomized trial. Scand J Med Sci Sports 2018; 28: 2074–2083. DOI: 10.1111/sms.13091 [DOI] [PubMed] [Google Scholar]
- 72.Panicker L, Prasun MA, Stockmann C, Simon J. Evaluation of chronic, noncancer pain management initiative in a multidisciplinary pain clinic. Pain Manag Nurs 2022; 23: 122–127. DOI: 10.1016/j.pmn.2021.09.003 [DOI] [PubMed] [Google Scholar]
- 73.Darnall BD, Mackey SC, Lorig K, Kao M-C, Mardian A, Stieg R, et al. Comparative effectiveness of cognitive behavioral therapy for chronic pain and chronic pain self-management within the context of voluntary patient-centered prescription opioid tapering: the EMPOWER study protocol. Pain Med 2020; 21: 1523–1531. DOI: 10.1093/pm/pnz285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Van de Velde D, De Zutter F, Satink T, Costa U, Janquart S, Senn D, et al. Delineating the concept of self-management in chronic conditions: a concept analysis. BMJ Open 2019; 9: e027775. DOI: 10.1136/bmjopen-2018-027775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Corp N, Mansell G, Stynes S, Wynne-Jones G, Morsø L, Hill JC, et al. Evidence-based treatment recommendations for neck and low back pain across Europe: a systematic review of guidelines. Eur J Pain 2021; 25: 275–295. DOI: 10.1002/ejp.1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.O’Sullivan K, O’Sullivan PB, O’Keeffe M. The Lancet series on low back pain: reflections and clinical implications. Br J Sports Med 2019; 53: 392–393. DOI: 10.1136/bjsports-2018-099671 [DOI] [PubMed] [Google Scholar]
- 77.van Dieën JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW. Analysis of motor control in patients with low back pain: a key to personalized care? J Orthop Sports Phys Ther 2019; 49: 380–388. DOI: 10.2519/jospt.2019.7916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tagliaferri SD, Miller CT, Owen PJ, Mitchell UH, Brisby H, Fitzgibbon B, et al. Domains of chronic low back pain and assessing treatment effectiveness: a clinical perspective. Pain Pract 2020; 20: 211–225. DOI: 10.1111/papr.12846 [DOI] [PubMed] [Google Scholar]
- 79.Zaina F, Balagué F, Battié M, Karppinen J, Negrini S. Low back pain rehabilitation in 2020: new frontiers and old limits of our understanding. Eur J Phys Rehabil Med 2020; 56: 212–219. DOI: 10.23736/S1973-9087.20.06257-7 [DOI] [PubMed] [Google Scholar]
- 80.Cowell I, O’Sullivan P, O’Sullivan K, Poyton R, McGregor A, Murtagh G. Perceptions of physiotherapists towards the management of non-specific chronic low back pain from a biopsychosocial perspective: a qualitative study. Musculoskelet Sci Pract 2018; 38: 113–119. DOI: 10.1016/j.msksp.2018.10.006 [DOI] [PubMed] [Google Scholar]
- 81.Gardner T, Refshauge K, McAuley J, Hübscher M, Goodall S, Smith L. Goal setting practice in chronic low back pain. What is current practice and is it affected by beliefs and attitudes? Physiother Theory Pract 2018; 34: 795–805. DOI: 10.1080/09593985.2018.1425785 [DOI] [PubMed] [Google Scholar]
- 82.Goorts K, Boets I, Decuman S, Du Bois M, Rusu D, Godderis L. Psychosocial determinants predicting long-term sickness absence: a register-based cohort study. J Epidemiol Community Health 2020; 74: 913–918. DOI: 10.1136/jech-2020-214181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Nijs J, Tumkaya Yilmaz S, Elma Ö, Tatta J, Mullie P, Vanderweeën L, et al. Nutritional intervention in chronic pain: an innovative way of targeting central nervous system sensitization? Expert Opin Ther Targets 2020; 24: 793–803. DOI: 10.1080/14728222.2020.1784142 [DOI] [PubMed] [Google Scholar]
- 84.Tatta J, Nijs J, Elma Ö, Malfliet A, Magnusson D. The critical role of nutrition care to improve pain management: a global call to action for physical therapist practice. Phys Ther 2022; 102: pzab296. DOI: 10.1093/ptj/pzab296 [DOI] [PubMed] [Google Scholar]
- 85.Torlak MS, Bagcaci S, Akpinar E, Okutan O, Nazli MS, Kuccukturk S. The effect of intermittent diet and/or physical therapy in patients with chronic low back pain: a single-blinded randomized controlled trial. Explore (NY) 2022; 18: 76–81. DOI: 10.1016/j.explore.2020.08.003 [DOI] [PubMed] [Google Scholar]
- 86.Van de Velde D, Eijkelkamp A, Peersman W, De Vriendt P. How competent are healthcare professionals in working according to a bio-psycho-social model in healthcare? The current status and validation of a scale. PLoS One 2016; 11: e0164018. DOI: 10.1371/journal.pone.0164018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Gordon RM, Corcoran JR, Bartley-Daniele P, Sklenar D, Sutton PR, Cartwright F. A transdisciplinary team approach to pain management in inpatient health care settings. Pain Manag Nurs 2014; 15: 426–435. DOI: 10.1016/j.pmn.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 88.Gottlieb LN. Ageism of knowledge: outdated research. Can J Nurs Res 2003; 35: 3–6. [PubMed] [Google Scholar]
- 89.Garschagen A, Steegers MAH, van Bergen AHMM, Jochijms JAM, Skrabanja TLM, Vrijhoef HJM, et al. Is there a need for including spiritual care in interdisciplinary rehabilitation of chronic pain patients? Investigating an innovative strategy. Pain Pract 2015; 15: 671–687. DOI: 10.1111/papr.12234 [DOI] [PubMed] [Google Scholar]
- 90.Peng-Keller S, Moergeli H, Hasenfratz K, Naef R, Rettke H, Hefti R, et al. Including the spiritual dimension in multimodal pain therapy. Development and validation of the Spiritual Distress and Resources Questionnaire (SDRQ). J Pain Symptom Manage 2021; 62: 747–756. DOI: 10.1016/j.jpainsymman.2021.02.021 [DOI] [PubMed] [Google Scholar]
- 91.Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003; 35: 1381–1395. DOI: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- 92.Brickwood K-J, Watson G, O’Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth 2019; 7: e11819. DOI: 10.2196/11819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Costantini L, Pasquarella C, Odone A, Colucci ME, Costanza A, Serafini G, et al. Screening for depression in primary care with Patient Health Questionnaire-9 (PHQ-9): a systematic review. J Affect Disord 2021; 279: 473–483. DOI: 10.1016/j.jad.2020.09.131 [DOI] [PubMed] [Google Scholar]
- 94.Catley MJ, O’Connell NE, Moseley GL. How good is the neurophysiology of pain questionnaire? A Rasch analysis of psychometric properties. J Pain 2013; 14: 818–827. DOI: 10.1016/j.jpain.2013.02.008 [DOI] [PubMed] [Google Scholar]
- 95.Melin J, Årestedt K. The Patient Participation in Rehabilitation Questionnaire (PPRQ): psychometric evaluation and revision for use in neurological rehabilitation. Disabil Rehabil 2020; 42: 1454–1461. DOI: 10.1080/09638288.2018.1528303 [DOI] [PubMed] [Google Scholar]
- 96.Schuurmans H, Steverink N, Frieswijk N, Buunk BP, Slaets JPJ, Lindenberg S. How to measure self-management abilities in older people by self-report. The development of the SMAS-30. Qual Life Res 2005; 14: 2215–2228. DOI: 10.1007/s11136-005-8166-9 [DOI] [PubMed] [Google Scholar]
- 97.Curtin RB, Walters BAJ, Schatell D, Pennell P, Wise M, Klicko K. Self-efficacy and self-management behaviors in patients with chronic kidney disease. Adv Chronic Kidney Dis 2008; 15: 191–205. DOI: 10.1053/j.ackd.2008.01.006 [DOI] [PubMed] [Google Scholar]
- 98.Van de Velde D, Coorevits P, Sabbe L, De Baets S, Bracke P, Van Hove G, et al. Measuring participation as defined by the World Health Organization in the International Classification of Functioning, Disability and Health. Psychometric properties of the Ghent Participation Scale. Clin Rehabil 2017; 31: 379–393. DOI: 10.1177/0269215516644310 [DOI] [PubMed] [Google Scholar]
- 99.Berenschot L, Grift Y. Validity and reliability of the (adjusted) Impact on Participation and Autonomy questionnaire for social-support populations. Health Qual Life Outcomes 2019; 17: 41. DOI: 10.1186/s12955-019-1106-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. DOI: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 101.Sanford K, Rivers AS. Treatment Adherence Perception Questionnaire: assessing patient perceptions regarding their adherence to medical treatment plans. Psychol Assess 2020; 32: 227–238. DOI: 10.1037/pas0000782 [DOI] [PubMed] [Google Scholar]
- 102.Asenlöf P, Siljebäck K. The Patient Goal Priority Questionnaire is moderately reproducible in people with persistent musculoskeletal pain. Phys Ther 2009; (89): 1226–1234. DOI: 10.2522/ptj.20090030 [DOI] [PubMed] [Google Scholar]
- 103.Krasny-Pacini A, Hiebel J, Pauly F, Godon S, Chevignard M. Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med 2013; 56: 212–230. DOI: 10.1016/j.rehab.2013.02.002 [DOI] [PubMed] [Google Scholar]
- 104.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991; 32: 705–714. DOI: 10.1016/0277-9536(91)90150-b [DOI] [PubMed] [Google Scholar]
- 105.Solbak NM, Robson PJ, Lo Siou G, Al Rajabi A, Paek S, Vena JE, et al. Administering a combination of online dietary assessment tools, the Automated Self-Administered 24-Hour Dietary Assessment Tool, and Diet History Questionnaire II, in a cohort of adults in Alberta’s Tomorrow Project. J Acad Nutr Diet 2021; 121: 1312–1326. DOI: 10.1016/j.jand.2021.01.014 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
BIOPSYCHOSOCIAL REHABILITATION IN THE WORKING POPULATION WITH CHRONIC LOW BACK PAIN: A CONCEPT ANALYSIS