Abstract
Ageing is a crucial risk factor for Alzheimer’s disease (AD) and is characterised by systemic changes in both intracellular and extracellular microenvironments that affect the entire body instead of a single organ. Understanding the specific mechanisms underlying the role of ageing in disease development can facilitate the treatment of ageing-related diseases, such as AD. Signs of brain ageing have been observed in both AD patients and animal models. Alleviating the pathological changes caused by brain ageing can dramatically ameliorate the amyloid beta- and tau-induced neuropathological and memory impairments, indicating that ageing plays a crucial role in the pathophysiological process of AD. In this review, we summarize the impact of several age-related factors on AD and propose that preventing pathological changes caused by brain ageing is a promising strategy for improving cognitive health.
Keywords: Alzheimer’s disease, Brain ageing, Hallmarks of ageing, Cell senescence, Chronic inflammation, Anti-ageing therapy
Background
With the rapid increase of the global ageing population, the age-related disorders, especially Alzheimer’s disease (AD), have emerged as a serious threat to the public health. AD is a neurodegenerative disorder and a leading cause of dementia in the elderly [1]. At present, more than 50 million individuals in the world have AD [2]. The incidence of AD increases with age, especially after age 65. In particular, 1 in 10 people aged ≥ 65 years has AD. Consequently, ageing is considered the primary risk factor for AD. However, the mechanisms underlying the age-related susceptibility to AD remain unclear [3].
The hallmarks of ageing, first proposed in 2013 [4], are defined based on the following three premises: (1) they should be related to age, (2) they can be experimentally manipulated to accelerate ageing and (3) they can stop or reverse ageing upon therapeutic intervention. Referring to López-Otín et al. [5] and Gorgoulis et al. [6], this review summarizes the relationship between AD and ageing based on the following 10 factors: genomic instability, macromolecular damage, epigenetic alterations, deregulated nutrient sensing, mitochondrial dysfunction, cellular senescence, stem cell exhaustion, altered intercellular communication, chronic inflammation and dysbiosis. These factors are closely associated with each other and are critical for understanding the occurrence and development of ageing as well as developing therapeutic strategies for age-related disorders [7].
‘Healthy brain ageing’ refers to the presence of abnormal ageing hallmarks confined to the body’s controllable range without causing harmful effects. In contrast, ‘pathological brain ageing’ refers to the presence of abnormal ageing hallmarks over the body’s controllable range. The progression from early (prodromal) to established AD is caused not only by ageing but also by the pathological deposition of amyloid beta (Aβ) or neurofibrillary tangles (NFTs) in the brain. Studies have demonstrated varying degrees of ageing, such as senescence of different cell types, in both AD patients and animal models [8]. Ameliorating the hallmarks of ageing, such as removing senescent cells, decreases the Aβ- and tau-induced neuropathology and improves memory in AD mice [9–11], suggesting that ageing plays a crucial role in the pathophysiological process of AD. However, the mechanisms underlying ageing and its neuropathophysiological role in AD remain unknown [12].
In this narrative review, we performed literature search in databases PubMed, Web of Science and Embase by using keywords “ageing”, “Alzhermer's disease” and each of the factors such as “genomic instability”. To describe the concept of implementation, Medical Subject Heading (MeSH) terms were used in PubMed and Emtree terms were used in Embase. We summarize the roles of various ageing-related markers in AD to elucidate the impact of ageing on the development of AD and provide novel insights into ageing-related diseases. Moreover, we list novel techniques to study the mechanisms underlying the role of ageing in AD and potential therapies targeting ageing for prevention and treatment of AD.
Hallmarks of ageing in the course of AD
Ageing is a significant risk factor for neurodegenerative disorders [13]. In healthy individuals, the ageing-associated decline of homeostasis leads to increased cellular stress, including oxidative stress, DNA damage and mitochondrial stress [14]. Senescence may initially occur to maintain homeostasis; however, excessive accumulation of senescent cells results in persistent inflammatory responses and tissue deterioration. The resulting inflammation may cause damage to synapses and lead to cognitive impairment [15, 16]. Patients with AD exhibit tau protein aggregation and Aβ deposition, which lead to ageing of different types of brain cells, resulting in local inflammation [17]. The inflammation, accompanied by accumulation of toxic proteins, contributes to the increased accumulation of stressors within cells, promotes the ageing phenotype and leads to chronic ageing [18]. In this section, we describe the relationship between AD and ageing by summarizing the effects of ageing-related factors on AD.
Intracellular hallmarks
Genomic instability
External stressors such as chemical, physical or biological factors, and endogenous stressors such as DNA replication errors and chromosomal segregation defects, can impair the integrity and stability of the genome [21]. These molecular alterations and the consequent genomic chimerism may contribute to both healthy and pathological ageing [22]. DNA replication errors may result in long-term, irreversible alterations in the final RNA and/or protein output, whereas abnormalities in other biological components are often transient [23].
Unlike proliferating (non-neuronal) cells that experience these changes for a brief period before being replaced, neurons are preserved for life and hence require the ability to withstand long-term damage [24]. Pascarella et al. [25] reported that somatic recombination profiles are altered in Parkinson’s disease and AD. Genomic abnormalities occurring during brain development can greatly increase the risk of AD. Methylazoxymethanol, a major genotoxin found in cycad seeds, induces specific DNA damage and is associated with enhanced tau expression and altered transcription of AD-related genes in primary rat neurons [26]. In AD, genes of DNA repair-associated enzymes are dysregulated in neurons. For instance, histone deacetylase (HDAC) 1, which is involved in DNA repair initiation, is downregulated in neurons in AD [27]. In a recent study, single-cell sequencing of the whole genome revealed increased DNA damage in neurons during neurodegeneration [28]. Neurons are susceptible to DNA damage owing to their non-proliferative nature and high metabolic activity. Excessive DNA damage in neurons is concentrated in genes with differential expression among patients with AD, indicating that dysregulation of gene expression in neurons may be associated with defective DNA repair. Double-strand breaks (DSBs) are the most destructive and severe type of DNA damage that may lead to cell death if not repaired or improperly repaired [29]. Accumulation of DSBs alters the transcription of genes located near the break site, consequently altering neuronal and synaptic function. An imbalance between the accumulation and the repair of DSBs in the brain may lead to neuronal damage as well as learning and memory impairments in AD [30]. Asada et al. [31] found that DSBs and phosphorylated tau frequently co-exist in the cortex of patients with AD. DNA damage may also be involved in the cell state transition under metabolic stress. For instance, DSBs promote the aberrant accumulation of p-tau. Additionally, environmental factors affect the susceptibility of neurons to oxidative stress. Astrocytes, microglia and vascular cells form the surrounding environment of neurons, which release antioxidants or oxidants to block or enhance reactive oxygen species (ROS)-induced damage [32]. Therefore, environmental factors play an essential role in preserving the integrity of DNA and ensuring the survival of neurons.
Almost half of the human genome is composed of repetitive sequences from transposable elements (TEs). Under the action of transposases, TEs can move between genes without relying on the homology of any DNA sequence. Therefore, they are involved in shaping mammalian genomes throughout evolution [33]. Although most TEs have mutated during evolution and have lost the ability to mutate in humans, more than 100 long interspersed elements have retained their full-coding potential and are capable of retrotransposition [34]. Uncontrolled activation of TEs has been observed in various models of neurodegeneration and in brain tissues of patients with neurodegeneration [35]. The CCCTC-binding factor (CTCF), a zinc finger protein that primarily acts as a transcription factor, is involved in gene regulation. The age-associated decrease in CTCF level may affect the expression of Aβ and tau [36]. CTCF is located upstream of many Aβ regulatory proteins, such as PAX6 [37], which regulates GSK-3β and catalyzes Aβ-mediated tau phosphorylation [38]. Defects in CTCF may alter the genome-wide chromatin accessibility and severely impede translation [39]. Therefore, a reduction of CTCF level with ageing may be the first step in the pathophysiological process of AD. Guo et al. [40] sequenced the RNAs of 636 human brain tissues and found that differential expression of numerous retrotransposons was associated with the burden of NFTs and tau-associated active chromatin signatures at various genomic locations. To reduce the transposon-induced replication barriers, cells utilize epigenetic defence mechanisms to limit transposition, including inhibition of heterochromatin formation and production of piwi-interacting RNAs (piRNAs), small RNAs that help to clear transposition factor transcripts [41]. Sun et al. [42] found that the tau deposition-induced absence of piwi and piRNAs and subsequent TE dysregulation seriously hinder the treatment of neurodegenerative diseases. Neurons are postmitotic cells. The neurons will partially acquire the ability to re-enter the cell cycle in AD [43, 44]. Additionally, chromosome 21-specific aneuploidy has been found to be increased in AD brains [45], and functional alterations in cell cycle regulators can influence neuronal migration, axon elongation and pruning, dendrite morphogenesis and synaptic maturation and plasticity, thereby contributing to the development of AD [46].
Altogether, genomic instability remarkably affects the development of AD (Fig. 1) [47]. Understanding the specific mechanisms underlying genomic instability in AD may facilitate the development of preventive strategies for the disease. Although both oxidative DNA damage and deficiencies in repair contribute to genomic instability and are implicated in neurodegenerative processes in AD, the age-related increase in oxidative DNA damage appears to play a predominating role. However, it remains unclear whether the neuronal DNA damage is predominantly induced by autonomous or involuntary processes, and the mechanisms underlying the disturbance of neuronal redox equilibrium that results in cell death and AD-related morbidity, remain unknown. Studies employing single-cell analysis have shown that AD involves complex interactions among all major cell types in the brain. With the development of bioinformatics technology, such as genomics and spatial transcriptomics, the temporal and spatial variations of the entire genome during AD have been successfully mapped. However, the key factors regulating the course of AD remain to be identified in future studies.
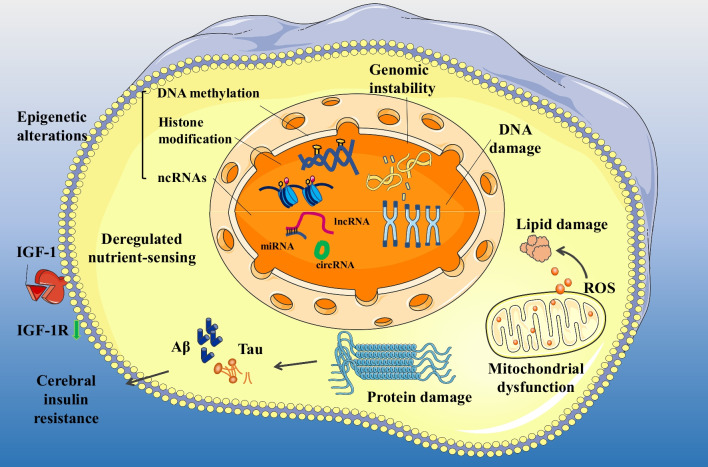
Fig. 1.
Intracellular hallmarks of ageing in AD. The intracellular hallmarks of ageing include genomic instability, macromolecular damage, epigenetic alterations, deregulated nutrient sensing and mitochondrial dysfunction. Additionally, protein damage in AD mainly manifests as the abnormal aggregation of Aβ and tau proteins, which is related to cerebral insulin resistance and affects nutrient sensing in nerve cells [19]. The green arrow indicates that IGF-1R is downregulated in the brain tissues of patients with AD [20]. AD Alzheimer’s disease, ncRNAs non-coding RNAs, lncRNA long non-coding RNA, miRNA microRNA, circRNA circular RNA
Macromolecular damage
DNA damage
DNA damage at the ends of chromosomes (telomeres) contributes to ageing and age-related disorders [48]. The reverse transcriptase activity of telomerase [49], an active ribonucleoprotein that maintains the sufficient length of telomeres, may prevent telomere loss. However, most somatic cells in mammals do not produce telomerase, resulting in the progressive erosion of telomere sequences from the ends of chromosomes throughout life [50, 51]. Mammals with extremely long telomeres live longer and have improved metabolic health [52]. Pharmacological activation of telomerase has been shown to delay normal ageing in mice.
As individuals continue to age, telomeres get shorter, and approximately 50 nucleotides are lost every cell cycle. Although neurons are post-mitotic cells whose telomeres do not shorten as a result of cell division, they may undergo irreversible DNA damage, leading to senescent cell types and even death [53]. Guan et al. [54] reported that the peripheral leukocytes of AD patients show a decreased proportion of the longest telomeres and a subtelomeric hypermethylation state specific for the shortest telomeres. In another study, Mendelian randomisation (MR) analysis [55] revealed that the genetically predicted longer telomere length is significantly associated with lower levels of Aβ in the cerebrospinal fluid (CSF). Telomerase reverse transcriptase (TERT) proteins, which maintain the length of telomeres, are found in the cytoplasm and mitochondria but not in the nucleus of hippocampal neurons [56]. Iannilli et al. [57] reported that TERT proteins can form complexes with RNA granules and the cell cycle inhibitor p15INK4b in the cytoplasm of hippocampal neurons. During oxidative stress, this complex is disrupted, and different components are released to promote cell senescence. In addition to maintaining telomere length, telomerase also functions to reduce oxidative stress and apoptosis and activate autophagy [58], playing an essential role in brain development and neuronal cells [59]. Both in vitro and in vivo studies have demonstrated that the inhibitory effects of rapamycin on oxidative stress and brain ageing depend on the presence of TERT proteins and its localization to mitochondria. In cells without TERT proteins, the inhibitory effects of rapamycin on the production of ROS are attenuated [60]. Defects in telomerase-rebinding enzymes, such as DNA-PKcs, increase the susceptibility of neurons to AD-associated pathological conditions [61]. Substances that can increase telomerase levels protect hippocampal neurons against Aβ toxicity by increasing the expression of neurotrophic factors and plasticity-related genes, indicating that telomere wear may have an important effect on the aetiology of AD [62]. Li et al. [63] reported that miR-340-5p increases telomere length, delays cell senescence and alleviates the symptoms of AD by reducing POT1 expression in mice.
Altogether, the ageing-induced telomere wear exacerbates DNA damage and contributes to the pathogenesis of AD. TERT proteins can not only increase telomere length, but also exert antioxidant and neuroprotective effects to alleviate the damage caused by telomere loss. Therefore, activating TERT proteins may represent a novel strategy for treating neurodegenerative diseases such as AD.
Protein damage
In healthy cells, proteostasis is maintained by a complex network of molecular chaperones, proteolytic processes and related regulatory factors [64]. These factors regulate protein synthesis, polypeptide folding, as well as the maintenance of protein structure and degradation. Multiple external and endogenous stressors that increase with age lead to protein damage. These stressors reduce the activity of the complex network that regulates proteostasis and the integrity of the proteome. Diseases such as AD, Parkinson’s disease and cataracts are caused by the misfolding and accumulation of aggregated proteins, which mostly affect postmitotic cell types such as neurons [65].
Accumulation of misfolded, oxidized, glycosylated or ubiquitinated proteins results in the production of intracellular inclusion bodies and extracellular Aβ, which play a key role in the progression of AD [66]. Errors in protein production become more common with increased age. Pro-adhesive proteins (PCDHs) are the largest subgroup of the calcium-dependent adhesion molecule (cadherin) family. PCDHα, PCDHβ and PCDHγ, three major protocadherin clusters, are abundantly expressed in the brain and play a role in the development of the central nervous system (CNS), cell differentiation and the formation of proper neural circuits [67]. Low expression of protocadherins has been associated with dysregulation of dendritic shape and branching. PCDHα is essential for learning and memory [68]. Consistently, Li et al. [69] reported that PCDHγC5 is upregulated in Aβ-treated hyperexcited neurons and transgenic APP/PS1 mice.
As a component of the network that regulates protein turnover, autophagy is closely related to the management of cell quality [70]. The inflammatory response and oxidative stress induced by Aβ may reduce macroautophagy. In addition, the decrease of autolysosome-driven acidification of neurons precedes the extracellular deposition of Aβ. Microglial autophagy maintains the α-synaptic nucleoprotein homeostasis, thereby regulating neuroinflammation and delaying the progression of AD [71]. Atg7 is a crucial regulator of autophagosome biogenesis and regulates lipid metabolism and neuroinflammation in microglia [72]. Deletion of the microglia-specific Atg7 results in the transformation of microglia to a pro-inflammatory phenotype in vivo and the activation of inflammasomes in vitro. Xu et al. [73] demonstrated that deficiency of Atg7 in microglia exacerbates tau pathology and its spreading in neurons. Chaperone-mediated autophagy (CMA) is a selective mode of autophagy that degrades neurodegeneration-related proteins [74]. Inhibition of CMA disrupts protein homeostasis and leads to changes in neuronal function. Suppression of CMA in a mouse model of AD has been shown to exert synergistic effects on proteins at risk of aggregation, thereby increasing the susceptibility to neurological disorders and accelerating disease progression. However, chemically enhancing CMA ameliorates characteristic pathology in two mouse models of AD [75]. Therefore, CMA plays an essential role in regulating protein homeostasis in neurons.
Recent studies analyzing whole-proteome changes during ageing have shown that protein homeostasis is involved in the entire pathological process of AD. In addition to classical Aβ and tau deposition, proteins such as cadherins greatly affect the development of AD. Changes in protein homeostasis are not limited to an increase or decrease in protein level. Conformational heterogeneity may considerably alter the functions of proteins such as chaperones. Pharmaceutical agents that improve protein homeostasis can be used to delay the onset of age-related diseases associated with proteome degradation [76].
Lipid damage
Lipids play an essential role in maintaining cell membrane integrity, energy production and signal transduction. Altered lipid metabolism has been observed in some ageing-related diseases. Impairment of lipid metabolism can induce AD by promoting Aβ deposition. APOE, a cholesterol/lipid transporter in the CNS, is the most influential risk factor for AD [77, 78]. The ε4 allele of the APOE gene (compared with the most common ε3 allele) is the strongest genetic risk factor and the relatively rare APOE ε2 allele is the strongest protective genetic factor against sporadic AD [78]. APOE and ABCA1 regulate cholesterol transfer into and out of brain cells, respectively. APOE/ABCA1 imbalance causes lipid accumulation in the brain [79]. Accordingly, deletion of the ABCA1 gene reduces APOE lipidation and increases Aβ deposition in the brain [80]. A rare mutation (R47H) in triggering receptor expressed on myeloid cells 2 (TREM2), a microglial surface receptor, has been associated with a substantially high risk of AD. TREM2 can activate microglia to phagocytose Aβ by sensing various anionic and zwitterionic lipids known to be associated with fibrous Aβ in lipid membranes [81]. Cholesterol metabolism in the brain is often impaired during ageing and AD [82]. Dysregulation of lipid metabolism is more pronounced in older individuals than in younger individuals. In a previous study, older mice were found to have a more persistent inflammatory response than younger mice after myelin injury. This phenomenon was attributed to the accumulation of excess myelin fragments in aged phagocytes, which resulted in the formation of cholesterol crystals that stimulate inflammasomes [83]. Wiley et al. demonstrated that senescent cells activate the biosynthesis of several oxidized lipids that promote the senescence-associated secretory phenotype (SASP) [84]. Quantitative analysis of these oxidized lipids may be an approach to assessing ageing. Several studies have shown that cerebral lipid peroxidation increases regionally in patients with AD. Notably, lipid metabolism disorder is frequently accompanied by neuroinflammation, and lipid damage is closely related to mitochondrial dysfunction during ageing [85]. The brain relies heavily on mitochondrial oxidative phosphorylation (OxPhos) to degrade fatty acids and maintain lipid homeostasis in astrocytes [86]. Abnormal OxPhos may induce the accumulation of lipid droplets in astrocytes. Moreover, when the accumulation of fatty acids exceeds the OxPhos capacity of astrocytes, the upregulated acetyl-CoA would induce astrocyte activation by enhancing the acetylation and activation of STAT3. Eventually, reactive astrocytes enriched with lipids induce neuroinflammation and oxidative stress [87]. Studies investigating the specific targets of lipid damage are limited. An in-depth understanding of the relationship between lipid damage and AD may help elucidate the pathogenesis of AD and develop more effective treatment methods.
Epigenetic alterations
Epigenetic changes that lead to ageing include altered DNA methylation patterns, abnormal histone post-translational modifications, abnormal chromatin remodelling and dysfunction of non-coding RNAs (ncRNAs) [88]. These regulatory, and often reversible, alterations affect gene expression and other cellular processes, leading to the development and progression of age-related diseases such as cancer, dementia, metabolic syndrome and bone disease [89].
DNA methylation
DNA methylation occurs when a hydrogen atom in a DNA strand is replaced by a methyl group. Methylation is catalyzed by DNA methyltransferases and typically occurs on the fifth carbon atom of the cytosine residue (5mC) of CpG and non-CpG (CpA, CpC and CpT) dinucleotides [90]. CpG dinucleotides are predominantly methylated in all organs of vertebrates, with approximately 80% of CpG sites possessing 5mC. The number of methylated CpH (mCpH) sites in the brain increases with age. Enhancers with hypermethylated CpH sites are associated with genes functionally enriched in immune responses, some of which are related to neuroinflammation and degeneration. A previous Whole Epigenome Association Study found that early-stage and severe AD patients have more genes with altered DNA methylation levels in the hippocampus, entorhinal cortex, dorsolateral prefrontal cortex (PFC) and cerebellum than control patients [91]. These genes have been associated with AD susceptibility and are involved in different pathological processes in neuronal or non-neuronal cells, such as Aβ pathology (APP, ABCA7), tau protein pathology, inflammation (IL-1β and IL-6) and abnormal protein metabolism (RPL13 and HOXA3) [92]. Han et al. [93] reported that the expression of the m6A methyltransferase METTL3 was increased and that of the m6A demethylase FTO was decreased in mice with AD. These findings suggest that m6A modification is enhanced during the development of AD.
Altogether, DNA methylation is implicated in ageing and AD (Fig. 1). AD-specific de novo methylation of numerous previously unmethylated sites plays a vital role in the development of AD [94]. Although the precise mechanisms underlying aberrant DNA methylation remain unclear, oxidative DNA damage has been reported to play a significant role. Given the close relationship between DNA methylation and damage responses, we hypothesize that AD-specific methylation patterns result from and reflect more oxidative damage, which necessitates substantial repair and eventually results in more errors. DNA methylation involves the coordination of different epigenetic markers, such as H3K18ac and H3K23ac (involved in the regulation of histone acetylation), which collectively affect gene transcription. Although the relationship between DNA methylation and histone modification remains elusive, the two mechanisms have been reported to involve shared regulatory pathways.
Histone modification
Histone modification is another essential epigenetic mechanism in which histones are covalently altered to modify the intrinsic chromatin structure and influence gene expression. In gene promoters and enhancers, methylation and acetylation of positively charged lysine (K) and arginine (R) residues are the most common histone modifications [95]. Histone modifications are dynamic and reversible and are regulated by enzymes known as writers (such as histone acetyltransferases or methyltransferases) and erasers (such as histone deacetylases or demethylases). An imbalance between writers and erasers results in the dysregulation of transcription and the alterations of epigenetic markers in many brain diseases. Dysregulation of histone methylation and acetylation has been associated with the pathogenesis of early-stage AD. HDACs are well-known enzymes that remove acetyl groups from lysine residues in the amino-terminal domain of histones [27]. Dysfunction of HDACs (HDAC1, HDAC2, HDAC3 and HDAC6) has been associated with cognitive impairment. The expression of HDAC1 and HDAC2 is decreased in the PFC and hippocampus in advanced AD [96]. The epigenome-wide H3K9 acetylation (H3K9ac) and H3K27ac levels are increased in AD [97]. In addition, upregulation of H3K9ac in the PFC and temporal lobe and its downregulation in the hippocampus may play a major role in the pathogenesis of AD, indicating that H3K9ac is a suitable therapeutic target for AD [98]. Recent studies have demonstrated that HDAC inhibitors improve memory and synaptic function in cellular and animal models of AD [99]. Alterations of many HDACs can affect ageing indicators in AD. As class III HDACs, sirtuins play an important role in regulating various physiological processes, including apoptosis, DNA repair, inflammatory responses and metabolism, and their function depends on nicotinamide adenine dinucleotides (NAD+) [100]. Zhao et al. [101] reported that the SIRT1–FOXO1/3–PINK1–Parkin pathway regulates mitochondrial autophagy to reverse mitochondrial dysfunction and exerts anti-AD effects.
Altogether, histone acetylation indicators, namely, H3K9ac and H3K27ac, have altered levels in AD, which may result in improper or excessive activation of implicated genes, leading to cell death. However, the levels of H3K9ac and H3K27ac in other regions of the brain in AD and the mechanisms underlying their aberrant levels remain unclear. Although histone H3 lysine 4 trimethylation (H3K4me3) and H3K9me2 (histone H3 lysine 9 dimethylation) are enriched in genes associated with cellular defense and memory development, in-depth information regarding the relationship between these modifications and genes is lacking [102]. Understanding the precise mechanisms underlying histone modification in response to DNA damage and changes in the levels of related markers at different disease stages may facilitate the development of methods for controlling histone modification in the treatment of AD.
ncRNAs
ncRNAs are a family of non-protein-coding transcripts that are subdivided into small ncRNAs (< 200 nucleotides) including microRNAs (miRNAs; approximately 22 nucleotides); long ncRNAs (lncRNAs; > 200 nucleotides); and circular RNAs (circRNAs) [103]. Approximately 80% of the human genome is transcribed as non-coding transcripts, whereas only 2% codes for proteins. ncRNAs are particularly prevalent in the CNS. Approximately 70% of miRNAs and 40% of lncRNAs are expressed in the brain. These non-coding transcripts are mostly found in the nucleus, indicating epigenetic control as their principal function [104]. Most ncRNAs are expressed with precise temporal and spatial patterns in the CNS. Dysregulation of complex multitasking ncRNAs (particularly miRNAs and lncRNAs) is related to the fundamental pathogenic phenotype of AD. The lncRNAs BACE1-AS, BC200 and NEAT1 have been associated with the regulation of Aβ aggregation, whereas the lncRNAs repressor element 1-silencing transcription factor (REST), RPPH1 (Ribonuclease P RNA Component H1), MALAH1, MEG3, miR-125-b, miR-361-3 and miR-122 have been associated with cellular apoptosis [105]. REST is an epigenetic master regulatory gene that serves as a marker of ageing in human cortical and hippocampal neurons, and its level is strongly associated with AD and life expectancy. REST binds to hundreds of genomic sites and controls numerous neuron-specific coding and non-coding genes. It forms complexes with histone-modifying enzymes and other proteins involved in chromatin remodelling [106]. These complexes may form a big complex with HOX antisense intergenic RNA (HOTAIR) and polycomb repressive complexes 2 (PRC2) [107]. PRC2 is present in almost all eukaryotic cells and is responsible for the epigenetic control of > 2000 genes on 10 chromosomes. Additionally, it is responsible for the alterations of 5%–10% of histones to the H3K27me3 form. REST increases the local H3K27me3 levels through PRC2. Given that H3K27me3 is important for DNA damage response and is associated with AD, HOTAIR may play a role in DNA damage response and AD pathogenesis by interacting with REST and PRC2 to regulate the levels of epigenetic markers, including H3K27ac, H3K27me3 and H3K4me3.
ncRNAs are involved in the formation of Aβ plaques, tau phosphorylation and inflammation, three major pathophysiological processes in AD (Fig. 1) [108]. However, the interactions among various ncRNAs remains unclear. Relatively comprehensive lncRNA-related competing endogenous RNA networks have been constructed based on brain tissue samples from APP/PS1 mice [109]. In future studies, these networks can be combined with multiple ncRNAs to gain novel insights into the diagnosis and treatment of AD.
Mitochondrial dysfunction
In addition to serving as the powerhouse of cells, mitochondria can potentially trigger inflammatory responses [110]. Mitochondrial function deteriorates with ageing due to various inter-related mechanisms, including accumulation of mitochondrial DNA mutation, dysregulation of the respiratory chain complex owing to the loss of protein homeostasis, reduced organelle turnover and alterations of mitochondrial dynamics. These alterations decrease the productive efficiency of mitochondria in cells, increase the production of ROS and may lead to abrupt mitochondrial membrane perforation, resulting in inflammation and cell death [111].
Although mitochondrial dysfunction is involved in each step of disease progression, the dysfunction can be observed before the occurrence of pathophysiological changes and targeted for early therapeutic intervention [112]. Localized hypometabolism in patients with AD can reveal initial signs of mitochondrial failure [113]. Changes in glucose metabolism in the brain can reflect alterations in energy metabolism in patients with AD [114]. Mitochondrial function can be affected by the interactions between AD-related neuropathological markers (APP, Aβ and tau) and genetic risk factors (APOE, etc.) [115–117]. A previous study showed that a low intracellular NAD+/NADH ratio is involved in the mitochondrial dysfunction-related senescence, and prevents the IL-1-mediated SASP through AMPK-mediated activation of p53 [118]. Swerdlow et al. have proposed the mitochondrial cascade hypothesis in AD [119]. In particular, addition of Aβ to mDNA-free neuronal cells does not induce cell death, indicating that the mitochondrial cascade reaction is important for triggering Aβ toxicity [120]. Mitochondria respond to changes in energy through continuous fission and fusion during AD [121]. Mitochondrial complex I has been shown to directly affect pTau deposition and energy homeostasis in mice [122]. As an important part of the mitochondrial cascade hypothesis, mitochondrial calcium overload is prevalent in AD, and the absence of the mitochondrial sodium/calcium exchanger can directly induce AD-like pathological characteristics [123]. Mitochondrial dysfunction may be secondary to abnormal deposition of neuropathological markers (APP, Aβ and tau), or a primary mitochondrial cascade may directly disturb vital brain functions [119].
The energy produced by mitochondria is required by astrocytes to perform neuroprotective functions. Interfering with mitochondrial homeostasis in astrocytes and the impaired ability of mitochondria to produce ATP can negatively affect neural function. In ageing or other pathological conditions, alterations in mitochondrial function in astrocytes may precede or accompany neuronal injury [124]. Mitochondria are the primary source of ROS, and the ROS generated by dysfunctional mitochondria may cause damage to DNA, lipids and proteins [125]. Park et al. reported that an increase in NADPH oxidase-4 level aggravates oxidative stress in human astrocytes through the production of mitochondrial ROS, fragmentation of mitochondria and suppression of cellular antioxidant mechanisms, thereby enhancing the ferroptosis of astrocytes [126].
The mitochondrial unfolded protein response (UPRmt) maintains protein homeostasis in mitochondria by initiating the transcriptional activation of mitochondrial chaperone proteins and proteases [127]. Inhibition of UPRmt is involved in several human disorders, including age-related diseases such as AD, Huntington’s disease and Parkinson’s disease [128]. Stimulation of UPRmt and high expression of UPRmt-related components have been associated with an extended lifespan. Shen et al. [129] reported that inhibition of UPRmt enhanced the toxic effects of Aβ25-35 on SHSY5Y cells. Sirtuin (SIRT) 3 is a deacetylase that is localized in mitochondria and regulates acetylation levels in mitochondria. SIRT3 expression and activity are significantly decreased in the hippocampal mitochondria in APP/PS1 mice [130]. The decreased expression is closely related to mitochondrial dysfunction and UPRmt [131]. Hou et al. [132] demonstrated that Honokiol, an anti-AD component derived from the bark of Magnolia officinalis, ameliorates the Aβ-induced mitochondrial dysfunction in a SIRT3-dependent manner. In addition, Sorrentino et al. [133] found that enhancement of mitochondrial proteostasis significantly delays the Aβ-associated symptoms in AD.
Given that mitochondria are important sites of cellular energy production, mitochondrial failure is common in neurodegenerative diseases, especially AD [134] (Fig. 1). Therefore, mitochondrial function plays an essential role in maintaining health, and progressive degradation of mitochondria can lead to ageing phenotypes. Treatment strategies targeting different elements of mitochondrial dysfunction involve the inhibition of mitochondrial processes associated with oxidative stress and apoptosis [135]. Early oxidative stress has been observed in the brains of AD patients and animal models. Therefore, antioxidant treatment may be beneficial [136]. A study demonstrated that the mitochondria-targeted antioxidant catalase (MCAT) transgenic AD mice (AD-MCAT) have longer survival and lower expression of neuropathological markers of AD (APP, oligo-Aβ) than AD mice [137]. These findings suggest that directing antioxidants to mitochondria is a viable strategy for effective treatment of ageing and AD. MitoQ, an antioxidant that targets mitochondria, reduces Aβ-induced neuronal cell death and oxidative stress in the cortical neurons of mice and alleviates AD-like symptoms [138, 139]. Altogether, mitochondrial oxidative stress plays an important role in the development of several pathological characteristics of AD, and an early intervention may be the key to successful therapies [140].
Deregulated nutrient sensing
Nutrient-sensing networks are highly evolutionarily conserved. Extracellular ligands, such as insulin and insulin-like growth factors, interact with receptor tyrosine kinases and intracellular signal cascades [141] to regulate several cellular processes, including autophagy, mRNA and ribosome biogenesis, protein synthesis, glucose and lipid metabolism and mitochondrial biogenesis [142]. Regulating the expression of genes involved in nutrient-sensing networks has been shown to extend survival in different animal models.
Insulin resistance is common in patients with early-onset AD. It impairs vascular function by affecting the clearance of Aβ peptides, phosphorylation of tau proteins, vascular reactivity, lipid metabolism and inflammation. Therefore, restoring insulin function in the brain may benefit patients with AD [143, 144].
Glucagon-like peptide 1 (GLP-1) is an incretin hormone released from enteroendocrine L-cells upon nutrient ingestion and also released by proglucagon-expressing neurons in the nucleus of the solitary tract (NTS) of the hindbrain. A recent study showed that GLP-1 limits glucose uptake and enhances beta-oxidation in cultured astrocytes, while deletion of GLP-1 receptor results in an adaptive stress response that improves systemic glucose homeostasis and memory development [145].
The Ras–Raf–Mek–Erk pathway is another important nutrition-related pathway involved in the development of AD. Activation of this pathway leads to the activation of transcription factors that stimulate the transcription of many cell cycle regulators and are associated with apoptosis. Suppression of the Ras/Mek/Erk signalling pathway may alleviate the AD-related cognitive impairment. Mai et al. [146] reported that deletion of DHCR24 resulted in hyperphosphorylation of tau in astrocytes through activation of the lipid raft-dependent Ras/Mek/Erk signalling pathway, which is involved in the aetiology of AD. Oxygen homeostasis is essential for maintaining cell function. 2-Oxoglutarate and ferrous iron-dependent oxygenases (2OGDDs) are hypoxia sensors that play an essential role in regulating oxygen homeostasis [147]. Several 2OGDD-related cellular processes are altered in the brains of AD patients. Therefore, 2OGDDs may act as key regulators of the transition from normal brain ageing to AD.
Altogether, deregulated nutrient sensing, with altered insulin signalling as its core, is a crucial component involved in the pathogenesis of AD (Fig. 1). The hippocampus, which plays a crucial role in memory development and consolidation, has wide distribution of insulin receptors and is a target of insulin resistance. Insulin signalling pathways promote neuronal survival and synaptic plasticity and contribute to advanced brain functions, such as cognition [148]. Disturbance of insulin signalling pathway increases the risk of AD. Given that insulin sensitivity is strongly influenced by environmental factors, the integrated role of biological, social and lifestyle factors in the progression of AD highlights the potential of psychological and behavioural interventions to prevent or delay AD [143].
Cellular hallmarks
Cellular senescence
Cellular senescence, which includes replicative senescence and stress-induced premature senescence, is the permanent cell cycle arrest [149]. The primary hallmarks of senescent cells include loss of the proliferative or regenerative capability, altered metabolic function, resistance to apoptosis and secretion of various disease-causing active molecules known as SASP factors [150]. In most cases, SASP is considered harmful and would lead to abnormalities in body function and age-related diseases. Studies in humans and animals have indicated a crucial role of cellular senescence in the onset of several age-related diseases [151]. Pre-clinical and clinical studies have indicated that cellular senescence plays a crucial role in the onset of several age-related diseases, including AD [10] (Fig. 2).
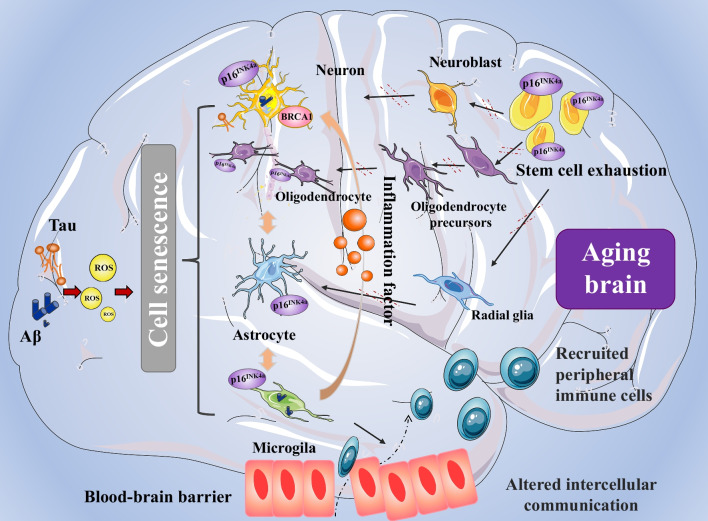
Fig. 2.
Cellular hallmarks of ageing in AD, including cellular senescence, disabled macroautophagy, stem cell exhaustion and altered intercellular communication. ROS activated by Aβ and tau can cause stress-induced cellular senescence [10, 152]. The senescent cells exhibit significant dysfunction and abnormal intercellular communication. Ageing microglia release more pro-inflammatory factors and have impaired phagocytic function [153]. Simultaneously, stem cell exhaustion inhibits the transformation of stem cells into neurons, astrocytes and oligodendrocytes [154]. AD Alzheimer’s disease, ROS reactive oxygen species, P16INK4a a marker of cellular senescence
Neuronal senescence
Age is the basic biological factor affecting subcortical and hippocampal symmetry [155]. As brain function constantly changes with age, alleviating the pathological damage caused by brain ageing is a promising strategy for improving cognitive function [156]. Mertens et al. reported that age-dependent cellular changes impair the functions of neurons in AD [157]. In another study, single-cell transcriptomic analysis revealed that neurons derived from patients with AD exhibited ageing-like features, including metabolic dysfunction and elevated levels of pro-inflammatory markers [158]. In AD, senescence of neurons may initially result from abnormal stimulation of proteins, such as Aβ and tau oligomers [159]. Wei et al. [160] reported that the level of the neuronal ageing-related marker p16 was significantly higher in 5 × FAD mice, indicating an evident ageing phenotype. In vitro experiments demonstrated that Aβ1-42 induced the production of p16 and aggravated cell ageing. Accumulation of tau-containing NFTs has been associated with brain ageing and cognitive decline. Musi et al. [10] and Dehkordi et al. [161] performed transcriptomic analysis on NFT-containing neurons from autopsied brain tissues of patients with AD and found that the expression profiles were consistent with those observed in cellular senescence. Metabolic abnormalities, changes in cholinergic receptors and neuroinflammation, which are risk factors for cell senescence, may occur in the brains at early stage of AD [162]. Senescent neurons may further suffer increased deposition of Aβ, creating a vicious feedback loop. Interleukin-like EMT inducer (ILEI, also known as the family with sequence similarity 3C) binds to the γ-secretase complex to suppress Aβ production without blocking γ-secretase activity. ILEI is widely expressed in normal neurons and ependymal cells, and its expression level peaks after birth and decreases with age. In a previous study, the number of ILEI-immunoreactive neurons was found to be lower in patients with AD than in age-matched control individuals [163]. The decreased expression of ILEI in ageing neurons may further induce the accumulation of Aβ in the brain and aggravate AD.
Brain ageing in AD appears to behave differently from normal ageing. Neurons lose the ability to reproduce during normal ageing, whereas numerous neurons re-enter the cell cycle during pathological ageing in AD, indicating the recovery of their reproductive potential [164]. However, these neurons often lose their normal function, coexist with cells characterised by ageing and are co-involved in the dysfunction of the ageing brain. Raina et al. [165] reported increased expression of MORF4 (a transcription-activating protein) in many neurons found in vulnerable brain regions in AD, indicating the re-entry of these neurons into the cell cycle. BRCA1, a known cell cycle regulator, is strongly expressed near NFTs in the brains of patients with AD. However, its expression is significantly reduced in normal-ageing brain tissues in clinical settings [166]. This difference in BRCA1 expression may explain the absence of neuronal re-entry into the cell cycle in the normal ageing brain and the abundance of neurons entering the cell cycle in AD. Therefore, these neurons may be studied to reveal the differences between normal ageing and pathological ageing in AD. However, to date, no studies have identified the mechanisms underlying the re-entry of neurons into the cell cycle in AD.
Astrocyte senescence
The burden of p16INK4a (a senescence biomarker)-positive astrocytes in the frontal cortex is substantially greater in patients with AD than in healthy individuals of the same age [167]. On the one hand, abnormal protein deposition, such as tau accumulation, induces the ageing of astrocytes; on the other hand, ageing astrocytes produce neurotoxic factors to induce inflammation and oxidative stress, further aggravating the development of AD [168]. The age-dependent increase in the expression of GFAP and astrocyte hypertrophy may reflect the potential toxicity of astrocytes [169]. Limbab et al. [170] reported that the X-irradiation-induced senescence of human astrocytes led to down-regulation of glutamate and potassium transporter genes in vitro. This downregulation caused neuronal cell death when the astrocytes were co-cultured with normal neurons. Aged astrocytes develop a neuroinflammatory A1-like reactive phenotype, and aged brains have more A1 reactive astrocytes in response to neuroinflammatory inducers, such as lipopolysaccharides. When the A1-like reactive astrocytes lose their normal function, they produce complement components and release a toxic factor that kills neurons and oligodendrocytes, leading to cognitive decline in vulnerable regions of the brain during normal ageing [171]. Turnquist et al. demonstrated a high abundance of senescent astrocytes in the brain tissues of patients with AD. These astrocytes exhibit the same SASP as senescent astrocytes in vitro [172]. Furthermore, Bussian et al. reported that the MAPTP301SPS19 mice with tau-dependent neurodegenerative disease have a high abundance of P16INK4A-positive senescent astrocytes, and clearance of these astrocytes significantly reduces the formation of NFTs [173].
Therefore, astrocyte senescence may play an important role in the progression of AD, and effective prevention of astrocyte senescence may represent an important therapeutic strategy for AD.
Microglial senescence
The continuous proliferation of microglia is a hallmark of AD. Microglial proliferation is significantly different between healthy and ageing brains [174]. A recent study showed that microglia undergo replicative senescence in the APP/PS1 model, which is dependent on early and sustained proliferation of microglia and characterized by increased senescence-associated β-galactosidase activity, age-related transcription signature and telomere shortening [153]. Microglia in patients with AD also exhibit an ageing phenotype [175]. As SASP factors are composed of various pro-inflammatory factors including cytokines, growth factors, angiogenic factors and soluble proteins, as well as extracellular vesicles [176], it is difficult to distinguish between the inflammatory activation state and the ageing state of inflammatory cell types such as microglia. The phagocytic function of microglia is usually enhanced at an inflammatory activation state [177] while substantially reduced at the ageing state. Hu et al. [178] reported that Aβ1-40 induced microglial senescence in vitro. Increased expression of CD38 in ageing microglia is associated with energy metabolism disorder and neuroinflammation. Moreover, Aβ substantially reduces the mRNA expression and protein level of SIRT1 (a major regulator of ageing) as well as the mRNA expression and translocation of NRF2, a critical transcription factor in inflammatory responses, resulting in impairment of the phagocytic function of microglia [179]. Notably, microglia tend to become proinflammatory and chemotactic during ageing. The aged microglia promote T-cell infiltration and exacerbate neuroinflammation in the brain by releasing chemokines [180]. In addition, the persistent inflammatory activation state can induce ageing, resulting in decreased phagocytic function of microglia [181]. In some cases, inflammation co-exists with the aging state. Additionally, aged microglia have abnormal metabolic activities [182]. The receptor TREM2 on microglia acts as a sensor for various lipids, whereas defects in TREM2 affect the Akt signalling pathway for lipid metabolism [183]. Microglia require prompt remodelling of the plasma membrane to monitor local changes in brain function and control neuronal activity. Yoo et al. found that replacing mutant microglia with circulation-derived myeloid cells following haematopoietic cell transplantation restores the function of Trem2 and improves cognitive function in a Trem2 mutant mouse model of AD [184]. This finding indicates that microglia may be targeted for alleviating the symptoms of AD.
Senescence of other cells
Decreased white matter volume and function is an important sign of brain ageing. Senescence of oligodendrocytes, a critical component of white matter, has been associated with decreased oligodendrocyte status and total oligodendrocyte density. By single-cell RNA sequencing, Kaya et al. [185] observed a lymphocyte-dependent, IFN-responsive microglial subpopulation localized near CD8+ T cells in the ageing white matter. CD8+ T cells can inhibit glial cell loss; however, the underlying mechanisms remain elusive. Peripheral immune cells play a crucial role in age-related neurodegenerative diseases [186]. Enhanced lymphocyte migration is involved in the amplified response of the ageing brain to acute exogenous inflammatory stimuli. However, the molecular regulation of blood–brain barrier (BBB) and the interaction between peripheral immune cells and the CNS during ageing warrant further investigations [187]. The age-related phenotypic changes of cerebrovascular endothelial cells lead to abnormal cerebral blood flow and disruption of the BBB, contributing to vascular cognitive impairment. Kiss et al. [188] used single-cell sequencing and found that the number of ageing endothelial cells increases by ~ 10% with advanced ageing. Bryant et al. reported that the expression of the SASP-related genes SERPINE1 and CXCL8 in microvascular endothelial cells of the frontal cortex was 2 times higher in patients with AD than in healthy individuals of the same age [189].
In summary, AD is closely associated with cellular senescence [164]. Exposure to toxic forms of Aβ or aggregated tau proteins can lead to senescence of several types of brain cells. Selective elimination of senescent cells can inhibit Aβ deposition and NFT formation in the brains of mice, thereby improving memory and learning [164, 190]. However, different types of cells have unique forms of ageing and may play different roles in ageing-related diseases. In future studies, single-cell RNA sequencing may be used to examine the effects of ageing on different types of brain cells and the efficacy of various anti-ageing therapies in distinct tissues.
Stem cell exhaustion
Adult stem cells are crucial for tissue homeostasis and regeneration. Stem cell exhaustion defined as the quantitative and qualitative reduction in stem cell activity during life, is considered one of the causes of ageing [191]. Unlike the adaptability of resident stem cells under normal homeostasis, the plasticity during injury diminishes with ageing [192].
Neural stem cells (NSCs) play an important role in physiological homeostasis and pathological repair of the CNS [193]. Because stem cells are highly delicate, their homeostasis may be disrupted under several circumstances, directly leading to decreased proliferation, which is one of the most prominent features of senescent stem cells. NSCs are usually deficient in differentiation and DNA-repair abilities in neurodegenerative disorders. Increased levels of p16INK4a, a marker of cell senescence and cell cycle arrest, and accumulation of damaged DNA, are closely associated with a decrease of stem cells during ageing [194]. The normal use of human stem cells (such as NSCs) requires maintenance of their nuclear structure and chromatin homeostasis. Nuclear reprogramming to pluripotency can revert both the age and the identity of any cell to that of an embryonic cell [195]. The H3K4me3 domain has been demonstrated to enhance the self-renewal and differentiation capabilities of mouse NSCs [196]. Although epigenetic dysregulation is associated with changes in stem cell populations throughout life, the mechanisms through which particular epigenetic markers and their regulators participate in stem cell senescence remain unknown and warrant further investigation. Protein homeostasis plays a crucial role in maintaining stem cell function. The transmembrane protein Ttyh1 is necessary for the survival of NSCs [197]. Based on an integrative bioinformatic analysis, Cao et al. [198] found that Ttyh1 regulates the resting and activation states of NSCs through Ca2+/NFATc3. Single-cell RNA sequencing of young and aged neurogenic niches revealed a decline in the number of activated NSCs in the ageing brain [199]. Lee et al. [200] reported that Aβ oligomers regulate the proliferation, differentiation and migration of human NSCs through glycogen synthase kinase-3β. The SASPs of other cells can induce the senescence of stem and progenitor cells, leading to poor tissue maintenance and reduced regenerative potential of tissues, eventually resulting in inflammation [201].
Oligodendrocyte progenitor cells (OPCs) are an important class of brain stem cells. In the brains of patients with AD, Aβ-associated OPCs expressing Olig2 and ng2 show increased expression of p21/CDKN1A and p16/INK4/CDKN2A and increased age-related β-galactosidase activity, exhibiting an ageing-like phenotype [154]. Direct exposure to Aβ induces senescence of OPCs in vitro. In mice with AD, senolytic treatment selectively removes senescent OPCs from the plaque environment, which reduces neuroinflammation and Aβ load and improves cognition. As an early event of AD, myelin fragmentation is closely related to the normal function of OPCs. Myelin-coated axons are maintained by a dynamic demyelinating–remyelinating equilibrium, which involves the coordinated action of OPCs and microglia [202]. OPCs develop into oligodendrocytes, which produce myelin. Microglia eliminate myelin debris and produce signalling molecules that stimulate the generation of oligodendrocytes from OPCs. However, as OPCs age, their differentiation rate decreases, diminishing their regenerative capacity. A previous study showed that the staining intensity of myelin basic protein and the density of OPCs in the hippocampus decrease with age in 3 × Tg AD mice. In addition, OPCs were found to undergo complicated age-related remodelling [203]. Degradation of OPCs is an early pathological indication of AD and represents a potential mechanism that drives myelin loss and cognitive impairment (Fig. 2).
Adult stem cells are essential for maintaining optimal tissue function. Many factors, including genomic instability, telomere wear, epigenetic alterations, cellular ageing, mitochondrial malfunction, protein homeostasis and altered intercellular communication, contribute to the age-related reduction in stem cell function. Therefore, stem cell regeneration may reverse the ageing phenotype in vivo, and understanding the underlying mechanisms may help to identify novel therapeutic targets for ameliorating age-related phenotypes and prolonging survival in humans. Some recent studies have shown that metabolites and their associated epigenetic regulators may reverse the ageing phenotype of adult stem cells. Regenerative stem cell ageing directly affects epigenetics and gene expression. Resveratrol protects adult stem cells from premature ageing and considerably extends the survival of mice by enhancing the interaction between SIRT1 and p53 in mice [204]. Exogenous stem cell therapies aim to restore cognitive function by introducing stem cells to repair the degraded neural networks. Based on the paracrine ‘bystander’ mechanism, these stem cells can be used as delivery systems through production or induced production of neuroprotective growth factors. Alternatively, functional recovery can be achieved by inducing the differentiation of stem cells to compensate for the degenerative neuronal circuits. Exogenous stem cell therapy has been shown to alleviate the cognitive impairment in APP/PS1 transgenic mice, Aβ1-42 brain perfusion mice and 3 × Tg-AD transgenic mice. However, clinical studies (NCT01297218, NCT01696591) have not demonstrated the beneficial effects of exogenous stem cell therapy in AD [205, 206].
Altered intercellular communication
Ageing is related to gradual changes in cell–cell communication, such as defects in neural, neuroendocrine and hormonal signalling pathways, which impair homeostasis and hormone regulation [207].
Alterations in neurotransmitters are closely related to synaptic alterations and neuronal loss in AD. Studies employing single-cell sequencing (snRNA-Seq) have revealed molecular pathways that regulate neuronal dysfunction [208] and demonstrated that excitatory neurons from AD patients show dysregulated expression of genes that are involved in neurotransmitter release, synaptic vesicular circulation and glutamate metabolism. Several differentially expressed genes are involved in postsynaptic scaffold formation, glutamate receptor trafficking and calmodulin signalling [209]. AD is associated with a decreased number of excitatory neurons and downregulation of NTNG1, a gene that regulates neurite development [210]. As secretory cells of the CNS, astrocytes release neurotransmitters (e.g. glutamate or GABA), neuromodulators (e.g. renal acid) and trophic factors. Some studies employing snRNA-Seq have indicated that genes related to glutamate receptor subunits (e.g., GRIA2, GRM3 and GRID2) are altered in astrocytes of AD patients [168, 211]. The metabolic reprograming of astrocytes in AD may affect their capacity to maintain nervous system homeostasis. Astrocytes may degrade harmful fatty acids (FAs) generated by hyperactive neurons. APOE4, a gene associated with the risk of AD, impairs lipid balance and energy transmission in the brain. It affects neuronal function by decreasing the separation of FAs from lipid droplets, the efficiency of FA transport and the capacity of astrocytes to degrade FAs, thereby impairing the metabolic and synaptic support for neurons [212]. Neurons and astrocytes closely interact with each other throughout the neurotransmitter cycle, also known as the glutamate/GABA-glutamine cycle. The metabolic abnormalities in astrocytes during the development of AD lead to defective metabolic support for neurons, resulting in synaptic dysfunction and neurodegeneration [213].
In addition, impaired abilities of microglia to detect and regulate neuronal activity may contribute to neuronal dysfunction in patients with AD. The ability of microglia to regulate neuronal activity may be compromised by changes in their metabolic state, which are partly associated with cellular stress and glycolysis. Ageing is often associated with an increased amount of inflammatory cytokines in the body; however, whether there are age-related alterations in cytokine signalling pathways and intercellular communication remains controversial. Xu et al. [214] reported that intracerebroventricular injection of tumor necrosis factor (TNF) α or interferon-γ increases the number of transcripts of CXCL9 and ICAM-1 (intercellular adhesion molecule-1) in both young and old mice. Additionally, the proportions of CD3+, CD4+ and CD8+ T lymphocytes in the brain parenchyma and choroid plexus increase with advancing age. These results suggest that the exposure of the brain to inflammation can lead to age-related lesions and the responses to inflammation become more severe with ageing.
The macrophage populations activated in response to brain ageing include parenchymal microglia, boundary-associated macrophages and mononuclear cells. Silvin et al. demonstrated that the embryonically derived TREM2-dependent disease-associated microglia (DAM) exert neuroprotective effects, whereas the monocyte-derived TREM2-expressing disease inflammatory macrophages (DIM) play a pro-inflammatory role. These two cell types accumulate in the brain during ageing [215]. Fahrenhold et al. [216] performed immunostaining on post-mortem brain tissues and found that TREM2 was not expressed in microglia but appeared to be a marker of monocyte recruitment in the brain. This finding suggests that TREM2 is a marker of recruited peripheral immune cells in the brain. Additionally, single-cell RNA sequencing revealed that in addition to neuronal ageing phenotypes, transcriptome changes in endothelial cells and microglia were prevalent in the ageing brain, whereas T-cell infiltration was prevalent in old neurogenic niches [199]. T cells may suppress the proliferation of NSCs by secreting interferon-γ both in vitro (co-culture) and in vivo. Therefore, T cells and NSCs can interact in the ageing brain and serve as potential targets for counteracting age-related impairments in brain function.
The BBB controls the homeostasis of the brain microenvironment by regulating the exchange of molecules and cells between blood and the brain [217]. The effect of vascular status on the BBB is a significant risk factor for AD [218]. Vascular disruption occurs in the early stage of AD and may affect cognitive impairment. Disruption of the BBB is related to endothelial and pericellular degeneration as well as changes in the basement membrane and astrocyte end-feet. BBB destruction allows the infiltration of blood-derived cells and circulatory factors into the brain and prevents Aβ clearance [219]. Microglia associated with capillaries control blood flow through purinergic actions. In AD, microglia may release factors that impair the integrity of endothelial tight junctions. Chemokines released by microglia may affect the inflamed condition of the endothelium membrane, which may, in turn, lead to neutrophil adhesion and reduced blood flow owing to capillary stalling [220]. CD19 is expressed in brain mural cells surrounding the endothelium, which are necessary for maintaining the integrity of the BBB. Parker et al. [221] evaluated CD19 expression in brain mural cells and verified perivascular presence of CD19 protein in human brain. Experiments in mice showed that although mice had less abundant CD19+ mural cells in the brain, CD19-directed therapies for tumors led to BBB leakiness, which was indicative of neurotoxicity. These findings suggest that CD19 may be an effective strategic target for improving the integrity of the BBB.
Similarly, impaired meningeal lymphatic drainage has been found to exacerbate the inflammatory response of microglia in AD [222]. Meningeal lymphatics are channels in the brain and transport large molecules, including Aβ, from cerebrospinal and interstitial fluids, whereas other metabolic wastes are cleared through the vascular bypass [223]. Under healthy conditions, immune cells usually cannot enter the meninges of the brain; therefore, meningeal lymphatic vessels transport macromolecular metabolites to the lymph nodes of the neck, where they are cleared by immune cells. However, the metabolic wastes will rapidly accumulate again [224]. Wu et al. [225] demonstrated that borneol accelerated the lymphatic clearance of Aβ by improving meningeal lymphatic drainage and alleviated cognitive impairment in Aβ-injected rats. This finding suggests that the cognitive ability in AD is related to the ability of meningeal lymphatic vessels to clear macromolecular metabolic wastes. Therefore, repairing and increasing the function of meningeal lymphatic vessels may be an effective strategy for AD prevention and treatment.
In conclusion, some researchers have attempted to identify cell–cell communication networks that may delay ageing and prolong survival [226]. Identifying commonly altered pathways may facilitate the development of novel therapeutic approaches involving numerous cell types [227]. In AD, almost all cell types including astrocytes, microglia, and neurons have immunological responses, including transcriptional responses involving cytokines, chemokines and MHC signalling pathways. Synaptic plasticity and unfolded protein response may be associated with the MHC signalling pathway [228]. Consequently, regulating the communication networks between different cell types is a promising strategy for treating neurodegenerative diseases such as AD (Fig. 2).
Systemic hallmarks
Chronic inflammation
Many studies have demonstrated that patients with AD have a chronic neuroinflammatory response. On the one hand, the neuroinflammatory response stimulates microglia to phagocytose Aβ, thereby decreasing Aβ accumulation. On the other hand, severe inflammation may cause irreparable nerve tissue damage [105]. Uyar et al. [232] conducted a large-scale integrated study based on single-cell analysis and found that the expression of genes related to cellular inflammation is usually upregulated with ageing. Although Aβ deposition is a primary cause of AD, several genetic variations in the inflammatory pathway may synergistically influence the risk of AD [233]. Dysregulation of inflammation during ageing may be an important cause of the progression of AD. In the CNS, microglia are activated after they detect ‘danger’ signals (e.g., Aβ). Upon activation, they produce pro-inflammatory factors and recruit monocytes and dendritic cells to the brain via disrupted BBB or the lymphatic system of the brain [234]. Sustained activation of microglia may lead to persistent inflammation and underlie the central neuropathophysiology of age-related neurodegeneration and cognitive decline. [235]. Cole et al. [236] found that APOBEC1-induced RNA editing was key to maintaining the resting state of microglia. Similar as bone marrow-derived macrophages, RNA editing in microglia alters the abundance of edited proteins that coordinate multiple cellular pathways. In contrast, mice lacking APOBEC1 in microglia showed abnormal regulation, manifesting as aggregation of activated microglia, abnormal myelination, elevated inflammation and lysosomal abnormalities, which led to behavioural and psychological deficits. Another study revealed that compared with brain tissues of young mice, the brain tissues of old mice showed over-recruitment of peripheral CCR2+ macrophages and augmented inflammatory responses after traumatic brain injury [237]. Baik et al. [238] found that chronic Aβ treatment induces innate immune tolerance in microglia, due to the defects in cellular metabolism. They also demonstrated that recombinant interferon-γ rescues the glycolytic metabolism and immune functions of microglia and alleviates the symptoms of AD in transgenic mice.
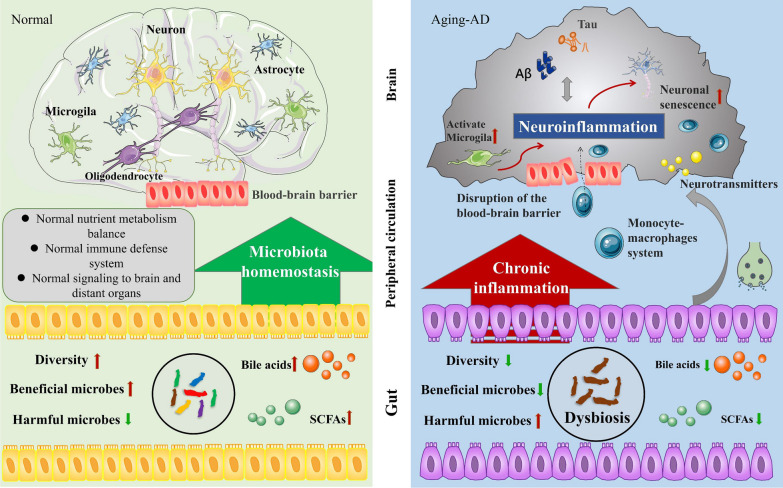
In conclusion, in AD, neuroinflammation is caused by aggregation of pathogenic tau proteins through activation of microglia and astrocytes, and the chronic inflammatory state is responsible for the subsequent neuronal loss (Fig. 3). However, anti-inflammatory drugs do not mitigate or prevent the development of AD [239]. Chronic inflammation may be a result of persistent pathophysiology in AD, which may in turn worsen the symptoms. Neuroinflammation, primarily induced by microglia and astrocytes, usually leads to dysfunction and degeneration of adjacent neurons, as the activated glial cells have reduced ability to maintain and support neurons while having increased expression of pro-inflammatory cytokines. This phenomenon is similar to ageing, in which the accumulation of senescent cells increases and initiates primary senescence, disrupting the ability of cells to maintain homeostasis and increasing their susceptibility to diseases. With disease onset, a second episode of ageing is triggered, resulting in a vicious feedback loop. Inflammation and ageing may worsen this feedback loop. Therefore, regulating the development and progression of chronic inflammation is a feasible preventive strategy for age-related diseases.
Fig. 3.
Changes in systemic ageing markers between normal and ageing (in AD) brains. Microbiota homeostasis maintains normal nutrient metabolism, immune defense and signaling transduction to the brain and other organs [229]. Dysbiosis, including decreased diversity of microbiota, decreased abundance of beneficial microbes, increased abundance of harmful microbes and decreased levels of bile acids and SCFAs, can cause a persistent inflammatory reaction [230]. Moreover, disruption of the BBB allows macrophages to enter the brain and aggravate neuroinflammation [231]. AD Alzheimer’s disease, SCFAs short-chain fatty acids
Dysbiosis
Disruption of the bidirectional bacteria–host relationship results in ecological disequilibrium. The microbiome pattern of healthy ageing in a majority of individuals is defined by the loss of key groups such as Bacteroides. Alistipes putredinis may minimize the risk of pathogenic infections and promote intestinal homeostasis, thereby decreasing the susceptibility to age-related chronic illnesses [240].
The human microbiome comprises bacteria found in the intestinal tract, oral cavity, nasal cavity and other organs interacting with the external environment. An imbalance of the microbiome in any organ may cause systemic abnormalities, with the intestinal microbiome being the most influential. The composition of intestinal microbes can be influenced by the increased intestinal barrier permeability and immune cell activation [241]. Enhanced secretion of lipopolysaccharides and bacterial amyloid proteins caused by gut dysbiosis may trigger activation of brain-resident immune cells, leading to impairments of intestinal permeability and BBB function, neuroinflammation, neuronal loss and eventually AD [242]. By cleaving Aβ precursor protein and tau proteins in the brain, the CCAAT/enhancer-binding protein/asparagine endopeptidase (C/EPP/AEP) signalling pathway contributes to the AD pathologies. Chen et al. [243] found that the gut dysbiosis in AD mice increases with age and is related to the C/EBP-β/AEP pathway. Compared with the microbiota of aged wild-type mice, the microbiota of aged AD mice accelerate the symptoms of AD in young AD mice, through the active C/EBP- β/AEP signalling. Antibiotic treatment and microbiome transplantation [244] can reduce the activity of this signalling pathway and improve cognitive function. Wang et al. [245] found that in AD mice, with the progression of AD, alterations in the gut microbiota composition result in the peripheral accumulation of phenylalanine and isoleucine, thereby promoting the differentiation and proliferation of pro-inflammatory T helper 1 (Th1) cells. These changes were also found in two cohorts of patients with mild cognitive impairment due to AD. These results suggest that changes in the gut microbiota composition play a role in early stages of AD.
In addition to gut microbiota, oral and nasal microbiota have also been found to be involved in the development of AD [246]. Microbes shared by intestinal, oral and nasal microbiota, particularly Porphyromonas gingivalis, may be associated with AD through a common pathway in the innate immune system [247]. Dominy et al. [248] found that oral P. gingivalis infection in mice led to bacterial colonisation in the brain. Furthermore, increased levels of Aβ1-42 and gingival protease (a toxic protease) are observed in the brains of patients with AD, indicating that these two factors are associated with tau- and ubiquitin-associated pathological changes. AD seems to involve microbiome in the brain [249]. The dominant microorganisms consistently detected in brain tissues from AD patients or animal models are Spirochaeta, herpes simplex virus, Chlamydia pneumoniae and Porphyria gingivalis [250]. These microorganisms are capable of altering the opsonophagocytosis activity of microglia and exacerbating AD disease [251].
In conclusion, dysbiosis can lead to enhanced secretion of lipopolysaccharides and amyloid protein, which may disrupt intestinal and BBB permeability. In patients with cognitive impairment, inflammatory microbes in the gut microbiota are associated with peripheral inflammation and Aβ deposition in the brain. Oral microbiome may influence the risk of AD through circulatory or neural pathways in the brain. Combined antibiotic therapy has been demonstrated to be effective in animal models of AD, highlighting the important role of dysbiosis in AD [252]. Remodelling the microbiota homeostasis may be a novel therapeutic strategy for AD.
Novel techniques to study the mechanisms underlying ageing in AD
As ageing is an inevitable process, elucidating the mechanisms underlying ageing is of great significance to the field of life sciences. With the continuous development of bioinformatic techniques, several novel methods have been used to understand these mechanisms [253].
Mendelian randomization (MR)
Given the complexity of factors affecting ageing, assessing the relationship between these factors and age-associated diseases is necessary for developing effective therapeutic strategies. Mediation analysis is a traditional approach to elucidating the effects of exposure on an outcome. However, traditional mediation analysis with non-instrumental variables is limited by several methodological difficulties, including bias due to the confounding between an exposure, mediator and outcome, and measurement errors. MR is a causal inference method that examines the influence of biological factors on diseases using genetic variants associated with the factors as instrumental variables [254]. MR uses the published genetic data to explore the causal relationship between exposure and outcome. Similar to randomised controlled trials (RCTs), MR ‘randomises’ the participating genes based on one or more alleles that influence risk factors to determine whether carriers of these genetic variants have a different risk of developing the disease compared with non-carriers. On the contrary, traditional observational studies examine the effects of exposure through questionnaires, biochemical markers or imaging approaches. Genetic variants are present at birth and remain stable throughout life. To date, numerous genetic variants strongly associated with specific traits have been identified, and many large-sample genome-wide association studies (GWAS) have published pooled data on several exposures and disease-related genetic variants. These aggregated data enable researchers to estimate genetic associations in large-sample studies, thereby facilitating the development of MR. As MR can avoid the influence of residual confounding factors on the accuracy of the results, the associations identified via MR are more reliable than those reported in observational studies or RCTs. MR can be used to improve the causal inference in mediation analysis using alleles that follow random assignment without being affected by confounding factors and not subject to reverse causation (which is observed in traditional epidemiological studies) [254]. For example, telomere shortening is difficult to detect in a population; however, MR translates it into a detectable mutation [255]. A MR study by Rodríguez et al. showed that a lower telomere length is causally related to an increased risk of AD [256]. To date, studies have neither reported a proven direct cause of AD nor revealed any risk factors that are easily modifiable, resulting in the lack of effective therapeutic strategies. MR method may remarkably improve the identification of risk factors for AD and facilitate the development of effective therapeutic strategies.
Omics analysis
The omics technology has revolutionized the detection of genes (genome), mRNAs (transcriptome), proteins (proteome) and metabolites (metabolomics) in cells.
Single-cell sequencing
Traditional studies usually focus on animal (in vivo) or cell (in vitro) models without consideration of the heterogeneity and the interactions among different cell types. Single-cell sequencing, an emerging bioinformatic technology, allows the analysis of heterogeneity among cells and cell–cell interactions [28, 257]. At present, a complete set of single-cell and spatial multiomics technologies is available, including single-cell transcriptome sequencing (sc-seq), single-cell ATAC sequencing (sc-ATAC-seq), single-cell immune library sequencing (scTCR/BCR-seq) and spatial transcriptomic sequencing. Compared with conventional omics techniques, single-cell sequencing allows independent analysis at the cellular level to assess heterogeneity among different cell types. The subsequent development of spatial transcriptomic sequencing allows direct mapping of the functions of cells in different parts of the body [258]. In studies of CNS diseases, single-cell sequencing has been primarily used to examine changes in the gene expression profiles in neurons, glia, microglia and immune cells to elucidate the pathogenesis and explore new therapeutic targets. To date, in studies of AD, single-cell sequencing has been utilized mainly for the following purposes: constructing a brain atlas; examining cells in the hippocampus, cortex and organoids; assessing the risks of diseases and finding novel treatment modalities (Table 1). In a previous study, transcriptomics analysis of different cell subsets in the PFC of 48 AD patients revealed AD pathology-related cell subsets characterized by regulators of myelination, inflammation and neuronal survival, revealing the molecular characteristics and pathogenesis of AD [259]. In another study, single-cell sequencing in blood and cerebrospinal fluid samples from AD patients revealed changes in peripheral and central acquired immune responses in the patients, suggesting changes in the immune microenvironment of AD [260]. Similarly, ncRNA sequencing may help identify AD-specific regulatory ncRNAs, thus providing a theoretical basis for considering ncRNAs as drug targets [261]. In addition, single-cell transcriptomic sequencing studies have demonstrated that microglia, interneurons and endothelial cells have differentially expressed genes in AD [259, 262]. Disruption of signalling pathways directly associated with these marker genes, such as inhibition of fractal and purine signalling pathways in microglia, and inhibition of neuropeptide signalling pathways in interneurons, may affect neural circuits. The loss of marker genes indicates the loss of transcription programs that control the identity of different cell types in AD, which may lead to cell senescence. Miller et al. [28] analyzed the single-cell sequencing data of neurons isolated from the PFC and the hippocampus of patients with AD and healthy individuals. They found that patients with AD had more somatic DNA changes and molecular patterns that differed from the age-related patterns of mutation observed in normal neurons. Additionally, AD was found with increased nucleotide oxidation associated with abnormal protein homeostasis. These findings provide valuable insights into the sequence of molecular and cellular processes that occur throughout the progression of AD [263].
Table 1.
Summary of recent studies on AD utilizing single-cell RNA sequencing
| Study and year | Platform | Region | Data accessibility | Main findings |
|---|---|---|---|---|
| Keren-Shaul et al. 2017 [264] | Illumina NextSeq 500 sequencer | Whole brains of 5xFAD mice and C57/BL6 mice | GEO: GSE98969 (single-cell RNA-seq) and GEO: GSE98970 (iChIP) | A novel microglial type associated with neurodegenerative diseases was described. The markers, spatial localisation and pathways associated with this cell type were identified |
| Mathys et al. 2017 [265] | Illumina HiSeq 2000 platform | Hippocampus of AD mice and control mice | GEO: GSE103334 | Two molecularly distinct phenotypes of reactive microglia were identified, characterized by modules of co-regulated type I and type II interferon response genes, respectively. The study also identified heterogeneity in microglial responses to neurodegeneration, disease stage-specific microglial states, cell reprogramming trajectory of microglial response to neurodegeneration and the underlying transcriptional pathways |
| Mathys et al. 2019 [259] | 10× Genomics platform | Prefrontal cortex of patients with AD and healthy individuals | https://www.radc.rush.edu/docs/omics.htm (snRNA-seq PFC) | The study identified different transcriptomic subsets, including those associated with pathology, characterised by regulators of myelination, inflammation and neuronal survival. The strongest disease-related changes occur early in the progression of AD and are highly cell type-specific, whereas in the later stages of AD, different cell types show similar upregulation of genes, mainly those involved in stress responses |
| Cosacak et al. 2019 [266] | 10× Genomics platform | Zebrafish brain | GEO: GSE118577 | The study provided extensive data on the molecular basis of NSC plasticity in the brains of adult zebrafish models of AD |
| Gate et al. 2020 [260] | Illumina HiSeq 4000 platform | Peripheral blood mononuclear cells of 97 healthy individuals, 31 patients with MCI, 28 patients with AD and 8 patients with PD | GEO: GSE134578 | The immune-related features of AD included an increase in the number of CD8+ T effector memory CD45RA+ (TEMRA) cells, and the proportion of CD8+ TEMRA cells was negatively associated with cognitive function. In addition, single-cell RNA sequencing showed that T cell receptor signalling was enhanced in these cells. The findings revealed adaptive immune responses in the blood and cerebrospinal fluid of patients with AD and provided evidence that cloned, antigen-experienced T cells patrol the intracranial space of the brain affected by age-related neurodegenerative diseases |
| Zhong et al. 2020 [267] | Illumina Hiseq-PE150 platform | Hippocampus of APP23 mice | GEO: GSE141044 | Comparative transcription analysis revealed various changes in different subtypes of hippocampal neurons in APP23 mice compared with control mice, and validated transcriptional changes in these neurons during disease progression |
| Xu et al. 2020 [268] | Illumina NovaSeq 6000 platform | Peripheral blood mononuclear cells of amyloid-positive AD patients and amyloid-negative healthy individuals | GEO: GSE181279 | Five immune cell subsets were revealed: CD4+ T cells, CD8+ T cells, B cells, natural killer cells and mononuclear macrophages. The characteristic changes in the proportions of these cell subsets and their gene expression patterns in AD were revealed. Protein–protein interaction network and pathway enrichment analyses revealed 31 cell type-specific key genes, including abundant human leukocyte antigen genes and multiple immune-related pathways. The study also revealed high-frequency amplification clones of T and B cells and decreased T cell diversity in AD. As clonal amplification suggests the activation of adaptive immune responses to specific antigens, the finding suggests that peripheral adaptive immune responses, especially those mediated by T cells, may play a role in the pathogenesis of AD |
| Leng et al. 2020 [269] | 10× Genomics platform | Post-mortem brain tissues | GEO: GSE147528 | The study identified a subpopulation of reactive astrocytes characterized by reduced expression of genes involved in homeostasis |
| Walgrave et al. 2021 [261] | 10× Genomics platform | Human hippocampal and serum samples | GEO: GSE172402 | The study revealed that miR-132 is one of the most consistently down-regulated miRNAs in AD and an effective regulator of adult hippocampal neurogenesis (AHN), and plays a cell-autonomic neurogenic role in adult neural stem cells and their progeny. AHN was shown to be directly affected by AD pathology. miR-132 replacement in the hippocampus of adult AD mice restored AHN and alleviated associated memory deficits |
| Lee et al. 2021 [270] | Illumina HiSeq4000 platform | Hippocampus of AD mice model | Cohort I (GSE160512), cohort II (GSE181786) and cohort III (GSE153895) | The spatial distribution of two types of oligodendrocytes with distinct transcriptional states was revealed. TREM2-deficient animals exhibited drastically delayed microglial responses to tau and Aβ pathology, whereas non-microglial (oligodendrocytes, astrocytes and T cells) responses remained unaltered |
| Freitag et al. 2022 [271] | 10× Genomics platform | Cerebral hemisphere of APP/PS1 mice | GEO: GSE206202 | The study identified a population of microglia characterized by elevated AXL levels and expression of phagocytosis- and cell-migration-related genes. Subsequent proteomic analysis of microglia isolated from APP/PS1 mice validated the anti-inflammatory and cytoskeletal effects of spermidine. Autophagy induced by spermidine altered the TLR3- and TLR4-mediated inflammatory processes, Aβ phagocytosis and motility in primary microglia and astrocytes |
| Lampinen et al. 2022 [272] | Illumina NovaSeq S1 platform | Olefin mucosa cells extracted from three cognitively healthy individuals (mean age, 71.7 years) and five patients with AD (mean age, 67.2 years) | European Genome-phenome Archive (EGA, https://ega-archive.org/, 10 February 2022) under the accession ID EGAS00001006019 | Single-cell RNA sequencing revealed altered expression of mitochondrial localization-related genes in olefin mucosa cells in AD. This finding was corroborated by functional assays, which revealed altered mitochondrial respiration and decreased ATP generation |
| Wood et al. 2022 [273] | Illumina NextSeq 2000 platform | Cerebral hemisphere of APPNL−F/NL−F knockin mice | All data reported in this study will be shared by the corresponding author upon request | The TREM2-dependent genes are all involved in phagocytosis and degradation. The decrease in phagocytosis markers is associated with an increase of tiny plaques in mice with TREM2 mutations. Furthermore, in the presence of R47H mutation that prevents the increase in TREM2 expression, there were still small increases in TREM2 protein and microglial density on plaques. The results indicate that the interaction between microglia and plaques and the activity of TREM2 are both required for microglia to respond appropriately to amyloid-related diseases |
Single-cell sequencing has advanced our understanding of diverse cell types in the brain, including oligodendrocytes, microglia and neurons. Comparing the sequencing data between humans and mice or non-human vertebrates can reveal markers of conserved or specific cell types, including the proportions of different cell types in tissues and species-specific gene expression patterns. Single-cell sequencing can be further improved by developing methods for long-term storage of tissues and cells without damage to genes, more standardized data quality control methods, dimensionality reduction in data analysis, and increasing the reliability of statistical analysis. At present, studies employing single-cell sequencing for examining brain diseases are lacking. It is necessary to understand the interactions between various types of cells during disease development. Additionally, AD-specific transcriptional abnormalities may not represent biological differences, as the changes in gene transcripts may not transmit into protein level changes. In addition, non-genomic processes that may not be observed via single-cell profiling, are also involved in the dysfunction in AD, including post-translational modifications and mRNA regulatory processes involved in local protein synthesis in various cell compartments and types. Altogether, single-cell sequencing enables comprehensive understanding of the pathophysiology of AD from perspectives of different cell types and multi-omics features, and would facilitate the development of novel strategies for preventing and treating AD.
Spatial transcriptomics
Molecular mapping techniques such as genomics and proteomics involve tissue separation, which results in the loss of morphological and spatial information. Recent advances in spatial molecular mapping methods have facilitated thorough molecular characterisation of cells while preserving their spatial and morphological integrity [274]. As compartmentalization is a fundamental feature of the brain, understanding the integrative functioning of different parts (in brain tissue) is crucial. Single-cell analysis helps understand this coordinated functioning, and spatial transcriptomics analysis provides insights into the whole-brain transcriptomic pattern associated with the pathological features of AD. In particular, spatial transcriptomic analysis is advantageous in ageing-related studies. Single-cell RNA sequencing requires the generation of single-cell suspensions, which are difficult to produce in older mice. Visium Spatial Gene Expression, a spatial transcriptomics technique, uses tissue slices as the input, overcoming the aforementioned limitation [275]. Studies employing pathological and immunohistochemical analyses have demonstrated the presence of complex inflammation-like changes around aggregated Aβ in patients with AD; however, the molecular changes and cellular interactions that characterize this response were not clear. Chen et al. [276] used the spatial transcriptomics technique and discovered transcriptional changes in tissue domains within a 100-μm diameter surrounding aggregated Aβ. They also demonstrated early changes in the co-expression network of myelin-related genes and oligodendrocyte genes. With technological advancements, the obstacles to spatial transcriptomics technique, including resolution and sensitivity restrictions, and feasibility of different tissues, are gradually improved. The spatial transcriptomics technique is compatible with paraffin-embedded tissues and allows retrospective analysis of samples collected over decades. Future advancements may facilitate the systematic assessment of larger tissues to generate 3D organ or organism-level maps and observe changes in gene expression throughout the transcriptome over time [277]. In addition to overcoming these technological obstacles, innovative computer tools and analytical methods should be developed in the future. These innovations may improve data analysis to elucidate anatomical patterns (essential characteristics of spatial transcriptomic datasets) and the underlying molecular mechanisms of genes.
Spatial proteomics
The function of a protein varies across different intracellular locations. Therefore, understanding the subcellular localization of a protein is important for determining its function. Upon synthesis, proteins function effectively only after being transported to the correct organelles. Spatial proteomics refers to the mapping of proteins at the single-cell or the tissue level. This technique allows detection of changes in the spatial expression profiles of proteins in diseases, providing a novel strategy for identifying biomarkers and developing effective diagnostic and therapeutic methods [278].
Prokop et al. used NanoString digital spatial profiling (DSP) to analyze the protein expression profiles of microglia in different brain regions and showed differences in immune response patterns across the examined brain regions [279]. DSP is an emerging technique that allows spatial analysis of proteins across multiple regions of interest in formalin-fixed paraffin-embedded tissue sections [280]. Walker et al. used DPS to analyze the protein expression profiles of NFT-bearing neurons, non-NFT-bearing neurons, and their neuronal microenvironment in the hippocampus. The results showed that low energetic and oxidative stress levels are important for the maintenance of neurons and their synaptic connections [281]. Vijayaragavan et al. developed a nanoscale framework integrating spatial proteomics and multiplexed ion beam imaging. This framework was used to examine neuropathological features, identify cell types and protein lesions in the hippocampus during different stages of AD, and assess the direct relationship between microglia and tau-related pathological changes in the CA1 hippocampal region in patients with AD [282]. In another study, the quantitative multiplex immunohistochemistry and visual colourimetric staining to enhance regional protein localisation (QUIVER) technique was developed to overcome the problem of unclear postmortem tissue immunostaining. Five molecular phenotypes of microglia/macrophage were identified in patients with AD using QUIVER in conjunction with digital pathological tools. The reactive and homeostatic microglial/macrophage phenotypes exhibit spatial polarization toward and away from Aβ, respectively. These findings suggest that QUIVER is a valuable tool for examining pathological changes in the brains of older adults [283]. Spatial proteomics is of great significance in clinical diagnosis and treatment. DISCO-MS, a technique that combines ultra-sensitive mass spectrometry (MS) with whole-organ/whole-organism clearance and imaging, allows unbiased proteomic analysis of preclinical and clinical tissues to identify diagnostic and therapeutic opportunities for complex diseases [284].
The development of single-cell proteomics is slower than that of genomic technology partly because that the proteomes cannot be amplified like nucleic acids and hence require extremely sensitive detection instruments. The current spatial proteomics methods used for characterizing protein expression have limitations. For example, the multi-immunofluorescence imaging coverage is usually limited to 20–100 proteins, and methods such as MS are not sensitive enough to capture the proteome at high spatial resolution [285]. The high resolution of modern microscopes and the increasing sensitivity of MS have increased the accuracy of proteomic analysis in natural subcellular settings; however, using images to measure protein abundance at the single-cell level remains a key challenge. Therefore, future studies on spatial proteomics should integrate AI-driven image analysis with automated single-cell or single-core laser microdissection with ultra-sensitive MS [286].
Spatial metabolomics
Spatial metabolomics that combines imaging mass spectrometry with metabolomic techniques examines the spatial molecular profiles in tissues in an unlabelled and untargeted manner. In the field of medicine, the spatial metabolomic technology can be used to localize molecular changes in tissue sections. Understanding the spatial localisation of metabolites is particularly important for addressing the complexity and heterogeneity of neurodegenerative diseases and their microenvironments. A spatial metabolomics study by Wang et al. [287] revealed effects of changes in gut microbiota composition on dopamine in the striatum of mice. Disturbance of microbial homeostasis is an important factor in AD. The spatial organization of metabolic processes of the microbial community, the interactions among microbes, and the exchange of metabolites between cells in various locations, can influence the overall metabolic activity of the community. In a recent review, Dal et al. [288] have discussed the mechanisms that drive the spatial arrangement of metabolic processes from the perspective of spatial metabolome and emphasized the influence of spatial organization of metabolic processes on the ecology and evolution of microbial communities. Although the spatial metabolomic technology holds great promise in studies on disease mechanisms, tissue classification, biomarker discovery and drug development, further development is required to improve the annotation of metabolites and the accuracy of spatial algorithms [289].
Multiomics analysis
AD is a complex multifactorial disease with changes in the multilayered biological networks, including protein imbalance (Aβ and tau aggregation), neuroinflammation and abnormal metabolism. Omics such as genomics, transcriptomics, proteomics and metabolomics are embedded within the theoretical and computational framework and can generate interpretable readings that describe the entire biological continuum of diseases from a systemic view [290, 291]. The combined use of multiple omics analyses can facilitate the identification of reliable biomarkers and improve clinical management of AD [292]. Extracellular vesicles (EVs), which are lipid bilayer particles released by most cells, play a crucial role in intercellular communication and systemic diseases. A multi-omics study conducted by Cohn et al. [293] was the first to report that many genetic risk factors of AD are associated with microglia-specific intercellular communications. The study revealed that approximately 1000 AD-specific proteins, 600 lipids and 100 miRNAs are present in microglia-derived EVs. In addition, the protein and lipid transports were found to be abnormal in AD, accompanied by a proinflammatory lipid profile, dysfunctional endolysosomes and upregulation of four miRNAs related to immune and cellular senescence signaling pathways in AD. Therefore, the analysis of microglia-derived EVs allows for development of new EV-related biomarkers and provides a framework for future larger-scale multi-omics studies on patient-derived cell type-specific EVs. Integration of multi-omics data into a synthetic neural network may help detect and map upstream mechanisms underlying the pathological changes in AD and downstream molecular effects in preclinical settings [294].
Potential therapeutic targets
Given that suppressing ageing can extend life expectancy and delay the development of age-related disorders, anti-ageing strategies developed based on biological, chemical, nanotechnological and immunological principles have attracted much attention. As of January 2022, 143 anti-AD drugs were under investigation in trials in the US. Of them, 119 (83.2%) drugs account for disease-modifying therapies, whereas only 24 (16.8%) drugs account for symptomatic treatment [295].
Anti-ageing efficacy is an important focus of studies on anti-AD drugs (Table 2). Among the mechanisms of action, proteostasis has been extensively studied [296]. A reason for the increased focus on proteostasis is that AD is characterized by abnormal protein deposition long before its association with ageing [297]. Immunotherapies offer the possibility of targeted elimination of abnormal proteins. A total of 12 monoclonal antibodies (mAbs) against Aβ have been developed for AD treatment, most of which are undergoing clinical trials. A new direction of mAb research is to target more-specific Aβ types and improve therapeutic effects while reducing side effects. Lecanemab, a newly developed mAb against Aβ [298], has a high affinity for large, soluble Aβ protofibrils and is currently undergoing investigation in a phase III trial [299]. Additionally, TRx0237 has entered a phase III clinical trial as a tau-aggregation inhibitor [300]. Liu et al. isolated homologous prostrong mycin from the marine bacterium Streptomyces tendae MCCC 1A01534. This compound inhibited tau aggregation to protect HT22 cells and exhibited low cytotoxicity, demonstrating its therapeutic potential for AD [301]. Furthermore, regulation of nutrient sensing can alleviate the symptoms of AD. The insulin sensitizer metformin can significantly decrease the risk of AD [302] and has demonstrated therapeutic efficacy in animal models of AD [303]. Metformin is currently undergoing investigation in a phase III clinical trial [304].
Table 2.
Anti-AD drugs with anti-ageing properties in trials
| Candidate drugs | Relevant AD hallmark of target | Mechanism of action | Outcome | Current clinical trial |
|---|---|---|---|---|
| Lecanemab | Loss of proteostasis | Monoclonal antibody directed at Aβ plaques and oligomers | Reduces Aβ deposition |
Phase 3 |
| Aducanumab | Loss of proteostasis | Monoclonal antibody directed at Aβ plaques and oligomers | Reduces Aβ deposition and controls inflammation |
Phase 3 |
| Donanemab | Loss of proteostasis | Monoclonal antibody specific for the pyroglutamate form of Aβ | Reduces Aβ deposition |
Phase 3 |
| Donanemab & Aducanumab | Loss of proteostasis | Combination of two monoclonal antibodies | Reduces Aβ deposition |
Phase 3 |
| Simufilam (PTI-125) | Loss of proteostasis | Filamin A protein inhibitor | Stabilizes the interaction between amyloid-alpha-7 and nicotinic receptor |
Phase 3 |
| Gantenerumab | Loss of proteostasis | Monoclonal antibody directed at Aβ plaques and oligomers | Reduces Aβ deposition |
Phase 3 |
| TRx0237 | Loss of proteostasis | Inhibitor of tau protein aggregation | Reduces tau protein aggregation |
Phase 3 |
| Valiltramiprosate (ALZ-801) | Loss of proteostasis | Prodrug of tramiprosate | Inhibits the aggregation of Aβ into toxic oligomers |
Phase 3 |
| ACI-35 | Loss of proteostasis | Active immunotherapy targeting tau | Reduces tau protein aggregation |
Phase 2 |
| Nilotinib BE | Disabled macroautophagy | Tyrosine kinase inhibitor; autophagy enhancer | Increases clearance of Aβ and tau |
Phase 3 |
| Losartan and Amlodipine and Atorvastatin + exercise | Deregulated nutrient sensing | Angiotensin II receptor blocker (losartan), calcium channel blocker (amlodipine) and cholesterol agent (atorvastatin) | Regulates vascular energy metabolism |
Phase 3 |
| Metformin | Deregulated nutrient sensing | Insulin sensitizer | Improves glucose metabolism in the CNS |
Phase 3 |
| Semaglutide | Deregulated nutrient sensing | GLP-1 agonist | Reduces neuroinflammation and improves insulin signalling in the brain |
Phase 3 |
| Tricaprilin | Mitochondrial dysfunction | Caprylic triglyceride | Induces ketosis and improves mitochondrial and neuronal function |
Phase 3 |
| MitoQ | Mitochondrial dysfunction | Mitochondria‐targeting antioxidant | Reduces systemic oxidative stress and increases cerebral oxygenation |
Phase 1 |
| AGB101 (low-dose levetiracetam) | Cellular senescence | Synaptic plasticity/neuroprotection | Reduces Aβ-induced neuronal overactivity | Phase 3 (NCT03486938) |
| Atuzaginstat (COR388) | Cellular senescence | Synaptic plasticity/neuroprotection | Reduces Aβ-induced neuronal overactivity | Phase 3 (NCT03823404) |
|
Dasatinib + Quercetin |
Cellular senescence | Tyrosine kinase inhibitor (dasatinib) and flavonoid (quercetin) | Decreases the number of senescent cells and tau aggregation |
Phase 1 (NCT04063124 and NCT04785300) Phase 2 |
| Deferiprone | Cellular senescence | Iron-chelating agent | Reduces the amount of reactive oxygen species |
Phase 2 |
| AVP-786 | Altered intercellular communication | Sigma 1 receptor agonist and NMDA receptor antagonist | Controls neuropsychiatric symptoms |
Phase 3 |
| AXS-05 | Altered intercellular communication | NMDA receptor antagonist | Controls neuropsychiatric symptoms |
Phase 3 |
| Donepezil | Altered intercellular communication | Acetylcholinesterase inhibitor | Improves cognitive impairment |
Phase 3 |
| Caffeine | Altered intercellular communication | Adenosine antagonist; non-specific phosphodiesterase inhibitor | Improves cognitive impairment |
Phase 3 |
| Blarcamesine (ANAVEX2-73) | Chronic inflammation | M2 autoreceptor antagonist | Improves oxidative stress, protein misfolding, mitochondrial dysfunction and inflammation |
Phase 3 |
| Hydralazine | Chronic inflammation | Free radical scavenger | Controls inflammatory response caused by oxidative stress |
Phase 3 |
| Icosapent ethyl (IPE) | Chronic inflammation | Purified form of the omega-3 fatty acid EPA | Improves synaptic function and reduces inflammation |
Phase 3 |
| NE3107 | Chronic inflammation | MAPK-1/3 inhibitor | Reduces activation of proinflammatory NFκB |
Phase 3 |
| Canakinumab | Chronic inflammation | Anti-IL-1β monoclonal antibody | Reduces neuroinflammation |
Phase 2 |
| Baricitinib | Chronic inflammation | Janus kinase inhibitor | Reduces neuroinflammation |
Phase 2 |
| GV-971 | Dysbiosis | Algae-derived acidic oligosaccharides | Regulates bacterial imbalance and reduces peripheral and central inflammation |
Phase 3 |
Because cell death is inevitable during ageing, inhibiting the death of various functional cells is also a focus of anti-ageing strategy. Upregulating different anti-apoptotic pathways may serve as an effective strategy for inhibiting ageing. Several anti-apoptotic mechanisms and their essential components have been identified as therapeutic targets for ageing. For example, SIRT6, an NAD+-dependent histone deacetylase, plays a vital role in several biochemical processes associated with DNA repair, nutrient metabolism and neurodegeneration, and is a promising therapeutic target for several disorders, including diabetes and ageing. Natural products such as isoquercetin can act as agonists of SIRT6 in the treatment of major human diseases such as AD and can be used to develop selective and potent scaffolds for SIRT6 [305]. Alternatively, targeted removal of senescent cells is considered an important strategy for inhibiting ageing [306]. Senolytics are a class of drugs that can selectively remove senescent cells. The most harmful senescent cells are resistant to apoptosis with upregulation of anti-apoptotic pathways that protect them from autoinflammatory SASPs and allow them to survive while killing neighbouring cells [307]. Senolytics can inactivate these anti-apoptotic pathways, resulting in the apoptosis of the senescent cells through tissue-destructive SASP factors [308]. Tau accumulation has been associated with cellular senescence [10]. In a study, intermittent administration of senolytics via gavage alleviated physical dysfunction and increased survival of old mice [309]. In addition, the combination of senolytics dasatinib and quercetin has demonstrated acceptable safety in the treatment of age-related diseases [310]. However, in-depth investigations are required before senolytics can be safely used in clinical settings.
Additionally, other therapeutic strategies are also under investigations, such as altering intercellular communication, inhibiting chronic inflammation and adjusting dysbiosis (Table 2). Altogether, in-depth research into ageing can help improve the treatment of AD.
Conclusions and perspectives
Mechanisms underlying ageing and AD are closely related and are a major focus of research at present. Ageing is a multifactorial process that involves the accumulation of molecular and cellular damage over time, resulting in declined biological functions and increased risk of age-related diseases. AD is a progressive and irreversible neurodegenerative disease that primarily affects memory and cognitive function.
Ageing is the most significant risk factor for AD; however, the relationship between ageing and AD, that is, whether ageing is a cause or an effect of AD, remains unclear. Some hallmarks of ageing that contribute to the development and progression of AD have been identified in recent studies [311].
In this review, we systematically summarize the potential molecular mechanisms underlying ageing in AD. AD and ageing accelerate the pathology of each other through a feedback loop. The use of cutting-edge techniques or methods such as MR, multi-omics analysis and single-cell sequencing has enabled researchers to examine the molecular and cellular changes occurring during ageing and AD. Based on the understanding of the mechanisms and shared pathways involved in ageing and AD, novel strategies for preventing and treating age-related diseases such as AD can be developed. Some potential avenues of research include identifying biomarkers of ageing and AD and developing novel drugs such as dasatinib plus quercetin that target cell senescence (NCT04063124 [312], NCT04785300 [18]). In addition, drugs aimed at improving proteostasis and mitochondrial function may also be used for AD treatment.
Acknowledgements
None.
Abbreviations
- Aβ
Amyloid beta
- AD
Alzheimer’s disease
- CMA
Chaperone-mediated autophagy
- CSF
Cerebrospinal fluid
- DSB
Double-strand breaks
- EV
Extracellular vesicle
- GLP-1
Glucagon-like peptide-1
- MR
Mendelian randomization
- NFT
Neurofibrillary tangles
- NSC
Neural stem cells
- OPC
Oligodendrocyte progenitor cell
- PCDH
Pro-adhesive proteins
- ROS
Reactive oxygen species
- SASP
Senescence-associated secretory phenotype
- SIRT1
Sirtuin-1
- TE
Transposable element
- TERT
Telomerase reverse transcriptase
- UPRmt
Mitochondrial unfolded protein response
Author contributions
YL and WP conceptualised, designed and wrote the primary draft of the manuscript. YL, YT, ZZ, MY, LZ and WP revised the final version of the manuscript. All authors contributed to discussion and revision of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81873169, 82104967), the Science and Technology Innovation Program of Hunan Province (2022RC1220), Hunan Provincial Natural Science Foundation of China (2022JJ40723, 2022JJ40728), and Hunan Flagship Department of Integrated Traditional Chinese and Western Medicine.
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Goikolea J, Gerenu G, Daniilidou M, Mangialasche F, Mecocci P, Ngandu T, et al. Serum Thioredoxin-80 is associated with age, ApoE4, and neuropathological biomarkers in Alzheimer's disease: a potential early sign of AD. Alzheimers Res Ther. 2022;14(1):37. doi: 10.1186/s13195-022-00979-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luo J, Thomassen JQ, Bellenguez C, Grenier-Boley B, de Rojas I, Castillo A, et al. Genetic associations between modifiable risk factors and Alzheimer disease. JAMA Netw Open. 2023;6(5):e2313734. doi: 10.1001/jamanetworkopen.2023.13734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hou Y, Dan X, Babbar M, Wei Y, Hasselbalch SG, Croteau DL, et al. Ageing as a risk factor for neurodegenerative disease. Nat Rev Neurol. 2019;15(10):565–581. doi: 10.1038/s41582-019-0244-7. [DOI] [PubMed] [Google Scholar]
- 4.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. The hallmarks of aging. Cell. 2013;153(6):1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: an expanding universe. Cell. 2023;186(2):243–278. doi: 10.1016/j.cell.2022.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Gorgoulis V, Adams PD, Alimonti A, Bennett DC, Bischof O, Bishop C, et al. Cellular senescence: defining a path forward. Cell. 2019;179(4):813–827. doi: 10.1016/j.cell.2019.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Xia X, Jiang Q, McDermott J, Han JJ. Aging and Alzheimer's disease: comparison and associations from molecular to system level. Aging Cell. 2018;17(5):e12802. doi: 10.1111/acel.12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stern Y. Cognitive reserve in ageing and Alzheimer's disease. Lancet Neurol. 2012;11(11):1006–1012. doi: 10.1016/S1474-4422(12)70191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ovadya Y, Krizhanovsky V. Senescent cells: SASPected drivers of age-related pathologies. Biogerontology. 2014;15(6):627–642. doi: 10.1007/s10522-014-9529-9. [DOI] [PubMed] [Google Scholar]
- 10.Musi N, Valentine JM, Sickora KR, Baeuerle E, Thompson CS, Shen Q, et al. Tau protein aggregation is associated with cellular senescence in the brain. Aging Cell. 2018;17(6):e12840. doi: 10.1111/acel.12840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu RM. Aging, cellular senescence, and Alzheimer's disease. Int J Mol Sci. 2022;23(4):1989. doi: 10.3390/ijms23041989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saez-Atienzar S, Masliah E. Cellular senescence and Alzheimer disease: the egg and the chicken scenario. Nat Rev Neurosci. 2020;21(8):433–444. doi: 10.1038/s41583-020-0325-z. [DOI] [PubMed] [Google Scholar]
- 13.Swaab DF. Brain aging and Alzheimer's disease, "wear and tear" versus "use it or lose it". Neurobiol Aging. 1991;12(4):317–324. doi: 10.1016/0197-4580(91)90008-8. [DOI] [PubMed] [Google Scholar]
- 14.Santos RX, Correia SC, Zhu X, Smith MA, Moreira PI, Castellani RJ, et al. Mitochondrial DNA oxidative damage and repair in aging and Alzheimer's disease. Antioxid Redox Signal. 2013;18(18):2444–2457. doi: 10.1089/ars.2012.5039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Newcombe EA, Camats-Perna J, Silva ML, Valmas N, Huat TJ, Medeiros R. Inflammation: the link between comorbidities, genetics, and Alzheimer's disease. J Neuroinflammation. 2018;15(1):276. doi: 10.1186/s12974-018-1313-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salminen A, Kaarniranta K, Kauppinen A. ER stress activates immunosuppressive network: implications for aging and Alzheimer's disease. J Mol Med. 2020;98(5):633–650. doi: 10.1007/s00109-020-01904-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Morawe T, Hiebel C, Kern A, Behl C. Protein homeostasis, aging and Alzheimer's disease. Mol Neurobiol. 2012;46(1):41–54. doi: 10.1007/s12035-012-8246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guerrero A, De Strooper B, Arancibia-Cárcamo IL. Cellular senescence at the crossroads of inflammation and Alzheimer's disease. Trends Neurosci. 2021;44(9):714–727. doi: 10.1016/j.tins.2021.06.007. [DOI] [PubMed] [Google Scholar]
- 19.Chen W, Huang Q, Lazdon EK, Gomes A, Wong M, Stephens E, et al. Loss of insulin signaling in astrocytes exacerbates Alzheimer-like phenotypes in a 5xFAD mouse model. Proc Natl Acad Sci USA. 2023;120(21):e2220684120. doi: 10.1073/pnas.2220684120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talbot K, Wang HY, Kazi H, Han LY, Bakshi KP, Stucky A, et al. Demonstrated brain insulin resistance in Alzheimer's disease patients is associated with IGF-1 resistance, IRS-1 dysregulation, and cognitive decline. J Clin Invest. 2012;122(4):1316–1338. doi: 10.1172/JCI59903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Briu LM, Maric C, Cadoret JC. Replication stress, genomic instability, and replication timing: a complex relationship. Int J Mol Sci. 2021;22(9):4764. doi: 10.3390/ijms22094764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Laffon B, Bonassi S, Costa S, Valdiglesias V. Genomic instability as a main driving factor of unsuccessful ageing: potential for translating the use of micronuclei into clinical practice. Mutat Res Rev Mutat Res. 2021;787:108359. doi: 10.1016/j.mrrev.2020.108359. [DOI] [PubMed] [Google Scholar]
- 23.Ferragut Cardoso AP, Banerjee M, Nail AN, Lykoudi A, States JC. miRNA dysregulation is an emerging modulator of genomic instability. Semin Cancer Biol. 2021;76:120–131. doi: 10.1016/j.semcancer.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scheijen EEM, Wilson DM., III Genome integrity and neurological disease. Int J Mol Sci. 2022;23(8):4142. doi: 10.3390/ijms23084142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pascarella G, Hon CC, Hashimoto K, Busch A, Luginbühl J, Parr C, et al. Recombination of repeat elements generates somatic complexity in human genomes. Cell. 2022;185(16):3025–3040.e3026. doi: 10.1016/j.cell.2022.06.032. [DOI] [PubMed] [Google Scholar]
- 26.Kisby GE, Spencer PS. Genotoxic damage during brain development presages prototypical neurodegenerative disease. Front Neurosci. 2021;15:752153. doi: 10.3389/fnins.2021.752153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pao PC, Patnaik D, Watson LA, Gao F, Pan L, Wang J, et al. HDAC1 modulates OGG1-initiated oxidative DNA damage repair in the aging brain and Alzheimer's disease. Nat Commun. 2020;11(1):2484. doi: 10.1038/s41467-020-16361-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller MB, Huang AY, Kim J, Zhou Z, Kirkham SL, Maury EA, et al. Somatic genomic changes in single Alzheimer's disease neurons. Nature. 2022;604(7907):714–722. doi: 10.1038/s41586-022-04640-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thadathil N, Hori R, Xiao J, Khan MM. DNA double-strand breaks: a potential therapeutic target for neurodegenerative diseases. Chromosome Res. 2019;27(4):345–364. doi: 10.1007/s10577-019-09617-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shanbhag NM, Evans MD, Mao W, Nana AL, Seeley WW, Adame A, et al. Early neuronal accumulation of DNA double strand breaks in Alzheimer's disease. Acta Neuropathol Commun. 2019;7(1):77. doi: 10.1186/s40478-019-0723-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Asada-Utsugi M, Uemura K, Ayaki T, Uemura M, Minamiyama S, Hikiami R, et al. Failure of DNA double-strand break repair by tau mediates Alzheimer's disease pathology in vitro. Commun Biol. 2022;5(1):358. doi: 10.1038/s42003-022-03312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cobley JN, Fiorello ML, Bailey DM. 13 reasons why the brain is susceptible to oxidative stress. Redox Biol. 2018;15:490–503. doi: 10.1016/j.redox.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chuong EB, Elde NC, Feschotte C. Regulatory activities of transposable elements: from conflicts to benefits. Nat Rev Genet. 2017;18(2):71–86. doi: 10.1038/nrg.2016.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elbarbary RA, Lucas BA, Maquat LE. Retrotransposons as regulators of gene expression. Science. 2016;351(6274):aac7247. doi: 10.1126/science.aac7247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Peze-Heidsieck E, Bonnifet T, Znaidi R, Ravel-Godreuil C, Massiani-Beaudoin O, Joshi RL, et al. Retrotransposons as a source of DNA damage in neurodegeneration. Front Aging Neurosci. 2021;13:786897. doi: 10.3389/fnagi.2021.786897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Burton T, Liang B, Dibrov A, Amara F. Transforming growth factor-beta-induced transcription of the Alzheimer beta-amyloid precursor protein gene involves interaction between the CTCF-complex and Smads. Biochem Biophys Res Commun. 2002;295(3):713–723. doi: 10.1016/S0006-291X(02)00725-8. [DOI] [PubMed] [Google Scholar]
- 37.Wu D, Li T, Lu Z, Dai W, Xu M, Lu L. Effect of CTCF-binding motif on regulation of PAX6 transcription. Investig Ophthalmol Vis Sci. 2006;47(6):2422–2429. doi: 10.1167/iovs.05-0536. [DOI] [PubMed] [Google Scholar]
- 38.Zhang Y, Zhang Y, Aman Y, Ng CT, Chau WH, Zhang Z, et al. Amyloid-β toxicity modulates tau phosphorylation through the PAX6 signalling pathway. Brain. 2021;144(9):2759–2770. doi: 10.1093/brain/awab134. [DOI] [PubMed] [Google Scholar]
- 39.Hilmi K, Jangal M, Marques M, Zhao T, Saad A, Zhang C, et al. CTCF facilitates DNA double-strand break repair by enhancing homologous recombination repair. Sci Adv. 2017;3(5):e1601898. doi: 10.1126/sciadv.1601898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo C, Jeong HH, Hsieh YC, Klein HU, Bennett DA, De Jager PL, et al. Tau activates transposable elements in Alzheimer's disease. Cell Rep. 2018;23(10):2874–2880. doi: 10.1016/j.celrep.2018.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang X, Ramat A, Simonelig M, Liu MF. Emerging roles and functional mechanisms of PIWI-interacting RNAs. Nat Rev Mol Cell Biol. 2023;24(2):123–141. doi: 10.1038/s41580-022-00528-0. [DOI] [PubMed] [Google Scholar]
- 42.Sun W, Samimi H, Gamez M, Zare H, Frost B. Pathogenic tau-induced piRNA depletion promotes neuronal death through transposable element dysregulation in neurodegenerative tauopathies. Nat Neurosci. 2018;21(8):1038–1048. doi: 10.1038/s41593-018-0194-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bonda DJ, Lee HP, Kudo W, Zhu X, Smith MA, Lee HG. Pathological implications of cell cycle re-entry in Alzheimer disease. Expert Rev Mol Med. 2010;12:e19. doi: 10.1017/S146239941000150X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhao F, Xu Y, Gao S, Qin L, Austria Q, Siedlak SL, et al. METTL3-dependent RNA m(6)A dysregulation contributes to neurodegeneration in Alzheimer's disease through aberrant cell cycle events. Mol Neurodegener. 2021;16(1):70. doi: 10.1186/s13024-021-00484-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iourov IY, Vorsanova SG, Yurov YB. Genomic landscape of the Alzheimer's disease brain: chromosome instability—aneuploidy, but not tetraploidy—mediates neurodegeneration. Neurodegener Dis. 2011;8(1–2):35–37. doi: 10.1159/000315398. [DOI] [PubMed] [Google Scholar]
- 46.Bajic V, Spremo-Potparevic B, Zivkovic L, Isenovic ER, Arendt T. Cohesion and the aneuploid phenotype in Alzheimer's disease: a tale of genome instability. Neurosci Biobehav Rev. 2015;55:365–374. doi: 10.1016/j.neubiorev.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 47.Rao CV, Yamada HY. How would preclinical Alzheimer's disease (AD pathology) occur? An insight from a genomic instability mouse model. Neural Regen Res. 2021;16(10):2012–2014. doi: 10.4103/1673-5374.308096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chakravarti D, LaBella KA, DePinho RA. Telomeres: history, health, and hallmarks of aging. Cell. 2021;184(2):306–322. doi: 10.1016/j.cell.2020.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu B, He Y, Wang Y, Song H, Zhou ZH, Feigon J. Structure of active human telomerase with telomere shelterin protein TPP1. Nature. 2022;604(7906):578–583. doi: 10.1038/s41586-022-04582-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aubert G, Lansdorp PM. Telomeres and aging. Physiol Rev. 2008;88(2):557–579. doi: 10.1152/physrev.00026.2007. [DOI] [PubMed] [Google Scholar]
- 51.Collins K. Mammalian telomeres and telomerase. Curr Opin Cell Biol. 2000;12(3):378–383. doi: 10.1016/S0955-0674(00)00103-4. [DOI] [PubMed] [Google Scholar]
- 52.Haussmann MF, Winkler DW, O'Reilly KM, Huntington CE, Nisbet IC, Vleck CM. Telomeres shorten more slowly in long-lived birds and mammals than in short-lived ones. Proc Biol Sci. 2003;270(1522):1387–1392. doi: 10.1098/rspb.2003.2385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jurk D, Wang C, Miwa S, Maddick M, Korolchuk V, Tsolou A, et al. Postmitotic neurons develop a p21-dependent senescence-like phenotype driven by a DNA damage response. Aging Cell. 2012;11(6):996–1004. doi: 10.1111/j.1474-9726.2012.00870.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guan JZ, Guan WP, Maeda T, Makino N. Analysis of telomere length and subtelomeric methylation of circulating leukocytes in women with Alzheimer's disease. Aging Clin Exp Res. 2013;25(1):17–23. doi: 10.1007/s40520-013-0006-0. [DOI] [PubMed] [Google Scholar]
- 55.Rodríguez-Fernández B, Vilor-Tejedor N, Arenaza-Urquijo EM, Sánchez-Benavides G, Suárez-Calvet M, Operto G, et al. Genetically predicted telomere length and Alzheimer's disease endophenotypes: a Mendelian randomization study. Alzheimers Res Ther. 2022;14(1):167. doi: 10.1186/s13195-022-01101-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fu W, Lu C, Mattson MP. Telomerase mediates the cell survival-promoting actions of brain-derived neurotrophic factor and secreted amyloid precursor protein in developing hippocampal neurons. J Neurosci. 2002;22(24):10710–10719. doi: 10.1523/JNEUROSCI.22-24-10710.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iannilli F, Zalfa F, Gartner A, Bagni C, Dotti CG. Cytoplasmic TERT associates to RNA granules in fully mature neurons: role in the translational control of the cell cycle inhibitor p15INK4B. PLoS ONE. 2013;8(6):e66602. doi: 10.1371/journal.pone.0066602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jaiswal RK, Kumar P, Yadava PK. Telomerase and its extracurricular activities. Cell Mol Biol Lett. 2013;18(4):538–554. doi: 10.2478/s11658-013-0105-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saretzki G. Telomerase and neurons: an unusual relationship. Neural Regen Res. 2022;17(11):2364–2367. doi: 10.4103/1673-5374.336133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Miwa S, Czapiewski R, Wan T, Bell A, Hill KN, von Zglinicki T, et al. Decreased mTOR signalling reduces mitochondrial ROS in brain via accumulation of the telomerase protein TERT within mitochondria. Aging (Albany NY). 2016;8(10):2551–2567. doi: 10.18632/aging.101089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kanungo J. DNA-dependent protein kinase and DNA repair: relevance to Alzheimer's disease. Alzheimers Res Ther. 2013;5(2):13. doi: 10.1186/alzrt167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boccardi V, Arosio B, Cari L, Bastiani P, Scamosci M, Casati M, et al. Beta-carotene, telomerase activity and Alzheimer's disease in old age subjects. Eur J Nutr. 2020;59(1):119–126. doi: 10.1007/s00394-019-01892-y. [DOI] [PubMed] [Google Scholar]
- 63.Li X, Zhang J, Yang Y, Wu Q, Ning H. MicroRNA-340-5p increases telomere length by targeting telomere protein POT1 to improve Alzheimer's disease in mice. Cell Biol Int. 2021;45(6):1306–1315. doi: 10.1002/cbin.11576. [DOI] [PubMed] [Google Scholar]
- 64.Hipp MS, Kasturi P, Hartl FU. The proteostasis network and its decline in ageing. Nat Rev Mol Cell Biol. 2019;20(7):421–435. doi: 10.1038/s41580-019-0101-y. [DOI] [PubMed] [Google Scholar]
- 65.Boland B, Yu WH, Corti O, Mollereau B, Henriques A, Bezard E, et al. Promoting the clearance of neurotoxic proteins in neurodegenerative disorders of ageing. Nat Rev Drug Discov. 2018;17(9):660–688. doi: 10.1038/nrd.2018.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Peng C, Trojanowski JQ, Lee VM. Protein transmission in neurodegenerative disease. Nat Rev Neurol. 2020;16(4):199–212. doi: 10.1038/s41582-020-0333-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Peek SL, Mah KM, Weiner JA. Regulation of neural circuit formation by protocadherins. Cell Mol Life Sci. 2017;74(22):4133–4157. doi: 10.1007/s00018-017-2572-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yamagishi T, Yoshitake K, Kamatani D, Watanabe K, Tsukano H, Hishida R, et al. Molecular diversity of clustered protocadherin-α required for sensory integration and short-term memory in mice. Sci Rep. 2018;8(1):9616. doi: 10.1038/s41598-018-28034-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li Y, Chen Z, Gao Y, Pan G, Zheng H, Zhang Y, et al. Synaptic adhesion molecule Pcdh-γC5 mediates synaptic dysfunction in Alzheimer's disease. J Neurosci. 2017;37(38):9259–9268. doi: 10.1523/JNEUROSCI.1051-17.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Griffey CJ, Yamamoto A. Macroautophagy in CNS health and disease. Nat Rev Neurosci. 2022;23(7):411–427. doi: 10.1038/s41583-022-00588-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Choi I, Heaton GR, Lee YK, Yue Z. Regulation of α-synuclein homeostasis and inflammasome activation by microglial autophagy. Sci Adv. 2022;8(43):eabn1298. doi: 10.1126/sciadv.abn1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Wang X, Wu R, Liu Y, Zhao Y, Bi Z, Yao Y, et al. m(6)A mRNA methylation controls autophagy and adipogenesis by targeting Atg5 and Atg7. Autophagy. 2020;16(7):1221–1235. doi: 10.1080/15548627.2019.1659617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Xu Y, Propson NE, Du S, Xiong W, Zheng H. Autophagy deficiency modulates microglial lipid homeostasis and aggravates tau pathology and spreading. Proc Natl Acad Sci USA. 2021;118(27):e2023418118. doi: 10.1073/pnas.2023418118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Kim HJ, Koh HC. Chaperon-mediated autophagy can regulate diquat-induced apoptosis by inhibiting α-synuclein accumulation cooperatively with macroautophagy. Food Chem Toxicol. 2021;158:112706. doi: 10.1016/j.fct.2021.112706. [DOI] [PubMed] [Google Scholar]
- 75.Bourdenx M, Martín-Segura A, Scrivo A, Rodriguez-Navarro JA, Kaushik S, Tasset I, et al. Chaperone-mediated autophagy prevents collapse of the neuronal metastable proteome. Cell. 2021;184(10):2696–2714.e2625. doi: 10.1016/j.cell.2021.03.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kumar B, Thakur A, Dwivedi AR, Kumar R, Kumar V. Multi-target-directed ligands as an effective strategy for the treatment of Alzheimer's disease. Curr Med Chem. 2022;29(10):1757–1803. doi: 10.2174/0929867328666210512005508. [DOI] [PubMed] [Google Scholar]
- 77.Chen Y, Strickland MR, Soranno A, Holtzman DM. Apolipoprotein E: structural insights and links to Alzheimer disease pathogenesis. Neuron. 2021;109(2):205–221. doi: 10.1016/j.neuron.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Serrano-Pozo A, Das S, Hyman BT. APOE and Alzheimer's disease: advances in genetics, pathophysiology, and therapeutic approaches. Lancet Neurol. 2021;20(1):68–80. doi: 10.1016/S1474-4422(20)30412-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Fan J, Donkin J, Wellington C. Greasing the wheels of Abeta clearance in Alzheimer's disease: the role of lipids and apolipoprotein E. BioFactors. 2009;35(3):239–248. doi: 10.1002/biof.37. [DOI] [PubMed] [Google Scholar]
- 80.Wahrle SE, Jiang H, Parsadanian M, Hartman RE, Bales KR, Paul SM, et al. Deletion of Abca1 increases Abeta deposition in the PDAPP transgenic mouse model of Alzheimer disease. J Biol Chem. 2005;280(52):43236–43242. doi: 10.1074/jbc.M508780200. [DOI] [PubMed] [Google Scholar]
- 81.Wang Y, Cella M, Mallinson K, Ulrich JD, Young KL, Robinette ML, et al. TREM2 lipid sensing sustains the microglial response in an Alzheimer's disease model. Cell. 2015;160(6):1061–1071. doi: 10.1016/j.cell.2015.01.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bonfili L, Cuccioloni M, Gong C, Cecarini V, Spina M, Zheng Y, et al. Gut microbiota modulation in Alzheimer's disease: Focus on lipid metabolism. Clin Nutr. 2022;41(3):698–708. doi: 10.1016/j.clnu.2022.01.025. [DOI] [PubMed] [Google Scholar]
- 83.Cantuti-Castelvetri L, Fitzner D, Bosch-Queralt M, Weil MT, Su M, Sen P, et al. Defective cholesterol clearance limits remyelination in the aged central nervous system. Science. 2018;359(6376):684–688. doi: 10.1126/science.aan4183. [DOI] [PubMed] [Google Scholar]
- 84.Wiley CD, Sharma R, Davis SS, Lopez-Dominguez JA, Mitchell KP, Wiley S, et al. Oxylipin biosynthesis reinforces cellular senescence and allows detection of senolysis. Cell Metab. 2021;33(6):1124–1136.e1125. doi: 10.1016/j.cmet.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Panov AV, Dikalov SI. Cardiolipin, perhydroxyl radicals, and lipid peroxidation in mitochondrial dysfunctions and aging. Oxid Med Cell Longev. 2020;2020:1323028. doi: 10.1155/2020/1323028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Rubio-Atonal LF, Ioannou MS. Astrocytic OxPhos: more than just energy production. Nat Metab. 2023;5(3):362–363. doi: 10.1038/s42255-023-00755-5. [DOI] [PubMed] [Google Scholar]
- 87.Mi Y, Qi G, Vitali F, Shang Y, Raikes AC, Wang T, et al. Loss of fatty acid degradation by astrocytic mitochondria triggers neuroinflammation and neurodegeneration. Nat Metab. 2023;5(3):445–465. doi: 10.1038/s42255-023-00756-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Zhang W, Qu J, Liu GH, Belmonte JCI. The ageing epigenome and its rejuvenation. Nat Rev Mol Cell Biol. 2020;21(3):137–150. doi: 10.1038/s41580-019-0204-5. [DOI] [PubMed] [Google Scholar]
- 89.Sen P, Shah PP, Nativio R, Berger SL. Epigenetic mechanisms of longevity and aging. Cell. 2016;166(4):822–839. doi: 10.1016/j.cell.2016.07.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Mattei AL, Bailly N, Meissner A. DNA methylation: a historical perspective. Trends Genet. 2022;38(7):676–707. doi: 10.1016/j.tig.2022.03.010. [DOI] [PubMed] [Google Scholar]
- 91.De Jager PL, Srivastava G, Lunnon K, Burgess J, Schalkwyk LC, Yu L, et al. Alzheimer's disease: early alterations in brain DNA methylation at ANK1, BIN1, RHBDF2 and other loci. Nat Neurosci. 2014;17(9):1156–1163. doi: 10.1038/nn.3786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Poon CH, Tse LSR, Lim LW. DNA methylation in the pathology of Alzheimer's disease: from gene to cognition. Ann NY Acad Sci. 2020;1475(1):15–33. doi: 10.1111/nyas.14373. [DOI] [PubMed] [Google Scholar]
- 93.Han M, Liu Z, Xu Y, Liu X, Wang D, Li F, et al. Abnormality of m6A mRNA methylation is involved in Alzheimer's disease. Front Neurosci. 2020;14:98. doi: 10.3389/fnins.2020.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Horvath S, Raj K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nat Rev Genet. 2018;19(6):371–384. doi: 10.1038/s41576-018-0004-3. [DOI] [PubMed] [Google Scholar]
- 95.Lawrence M, Daujat S, Schneider R. Lateral thinking: how histone modifications regulate gene expression. Trends Genet. 2016;32(1):42–56. doi: 10.1016/j.tig.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 96.Kumar V, Kundu S, Singh A, Singh S. Understanding the role of histone deacetylase and their inhibitors in neurodegenerative disorders: current targets and future perspective. Curr Neuropharmacol. 2022;20(1):158–178. doi: 10.2174/1570159X19666210609160017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Nativio R, Lan Y, Donahue G, Sidoli S, Berson A, Srinivasan AR, et al. An integrated multi-omics approach identifies epigenetic alterations associated with Alzheimer's disease. Nat Genet. 2020;52(10):1024–1035. doi: 10.1038/s41588-020-0696-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.De Jager PL, Ma Y, McCabe C, Xu J, Vardarajan BN, Felsky D, et al. A multi-omic atlas of the human frontal cortex for aging and Alzheimer's disease research. Sci Data. 2018;5:180142. doi: 10.1038/sdata.2018.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lu X, Wang L, Yu C, Yu D, Yu G. Histone acetylation modifiers in the pathogenesis of Alzheimer's disease. Front Cell Neurosci. 2015;9:226. doi: 10.3389/fncel.2015.00226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jiao F, Gong Z. The beneficial roles of SIRT1 in neuroinflammation-related diseases. Oxid Med Cell Longev. 2020;2020:6782872. doi: 10.1155/2020/6782872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Zhao N, Xia J, Xu B. Physical exercise may exert its therapeutic influence on Alzheimer's disease through the reversal of mitochondrial dysfunction via SIRT1-FOXO1/3-PINK1-Parkin-mediated mitophagy. J Sport Health Sci. 2021;10(1):1–3. doi: 10.1016/j.jshs.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Klein HU, McCabe C, Gjoneska E, Sullivan SE, Kaskow BJ, Tang A, et al. Epigenome-wide study uncovers large-scale changes in histone acetylation driven by tau pathology in aging and Alzheimer's human brains. Nat Neurosci. 2019;22(1):37–46. doi: 10.1038/s41593-018-0291-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Akbari Dilmaghnai N, Shoorei H, Sharifi G, Mohaqiq M, Majidpoor J, Dinger ME, et al. Non-coding RNAs modulate function of extracellular matrix proteins. Biomed Pharmacother. 2021;136:111240. doi: 10.1016/j.biopha.2021.111240. [DOI] [PubMed] [Google Scholar]
- 104.Panni S, Lovering RC, Porras P, Orchard S. Non-coding RNA regulatory networks. Biochim Biophys Acta Gene Regul Mech. 2020;1863(6):194417. doi: 10.1016/j.bbagrm.2019.194417. [DOI] [PubMed] [Google Scholar]
- 105.Liu Y, Cheng X, Li H, Hui S, Zhang Z, Xiao Y, et al. Non-Coding RNAs as novel regulators of neuroinflammation in Alzheimer's disease. Front Immunol. 2022;13:908076. doi: 10.3389/fimmu.2022.908076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Lu T, Aron L, Zullo J, Pan Y, Kim H, Chen Y, et al. REST and stress resistance in ageing and Alzheimer's disease. Nature. 2014;507(7493):448–454. doi: 10.1038/nature13163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Tsai MC, Manor O, Wan Y, Mosammaparast N, Wang JK, Lan F, et al. Long noncoding RNA as modular scaffold of histone modification complexes. Science. 2010;329(5992):689–693. doi: 10.1126/science.1192002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Idda ML, Munk R, Abdelmohsen K, Gorospe M. Noncoding RNAs in Alzheimer's disease. Wiley Interdiscip Rev RNA. 2018;9(2):e1463. doi: 10.1002/wrna.1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ma N, Tie C, Yu B, Zhang W, Wan J. Identifying lncRNA-miRNA-mRNA networks to investigate Alzheimer's disease pathogenesis and therapy strategy. Aging (Albany NY). 2020;12(3):2897–2920. doi: 10.18632/aging.102785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Iwata R, Casimir P, Erkol E, Boubakar L, Planque M, Gallego López IM, et al. Mitochondria metabolism sets the species-specific tempo of neuronal development. Science. 2023;379(6632):eabn4705. doi: 10.1126/science.abn4705. [DOI] [PubMed] [Google Scholar]
- 111.Abate M, Festa A, Falco M, Lombardi A, Luce A, Grimaldi A, et al. Mitochondria as playmakers of apoptosis, autophagy and senescence. Semin Cell Dev Biol. 2020;98:139–153. doi: 10.1016/j.semcdb.2019.05.022. [DOI] [PubMed] [Google Scholar]
- 112.Wan W, Zhang L, Lin Y, Rao X, Wang X, Hua F, et al. Mitochondria-derived peptide MOTS-c: effects and mechanisms related to stress, metabolism and aging. J Transl Med. 2023;21(1):36. doi: 10.1186/s12967-023-03885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Butterfield DA, Halliwell B. Oxidative stress, dysfunctional glucose metabolism and Alzheimer disease. Nat Rev Neurosci. 2019;20(3):148–160. doi: 10.1038/s41583-019-0132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Hipkiss AR. Aging, Alzheimer's disease and dysfunctional glycolysis; similar effects of too much and too little. Aging Dis. 2019;10(6):1328–1331. doi: 10.14336/AD.2019.0611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Anandatheerthavarada HK, Devi L. Amyloid precursor protein and mitochondrial dysfunction in Alzheimer's disease. Neuroscientist. 2007;13(6):626–638. doi: 10.1177/1073858407303536. [DOI] [PubMed] [Google Scholar]
- 116.Kim DK, Jeong H, Bae J, Cha MY, Kang M, Shin D, et al. Aβ-induced mitochondrial dysfunction in neural progenitors controls KDM5A to influence neuronal differentiation. Exp Mol Med. 2022;54(9):1461–1471. doi: 10.1038/s12276-022-00841-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Qin L, Zhu X, Friedland RP. ApoE and mitochondrial dysfunction. Neurology. 2020;94(23):1009–1010. doi: 10.1212/WNL.0000000000009569. [DOI] [PubMed] [Google Scholar]
- 118.Wiley CD, Velarde MC, Lecot P, Liu S, Sarnoski EA, Freund A, et al. Mitochondrial dysfunction induces senescence with a distinct secretory phenotype. Cell Metab. 2016;23(2):303–314. doi: 10.1016/j.cmet.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Swerdlow RH. Mitochondria and mitochondrial cascades in Alzheimer's disease. J Alzheimers Dis. 2018;62(3):1403–1416. doi: 10.3233/JAD-170585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Cardoso SM, Santos S, Swerdlow RH, Oliveira CR. Functional mitochondria are required for amyloid beta-mediated neurotoxicity. Faseb J. 2001;15(8):1439–1441. doi: 10.1096/fj.00-0561fje. [DOI] [PubMed] [Google Scholar]
- 121.Zhang L, Trushin S, Christensen TA, Bachmeier BV, Gateno B, Schroeder A, et al. Altered brain energetics induces mitochondrial fission arrest in Alzheimer's Disease. Sci Rep. 2016;6:18725. doi: 10.1038/srep18725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Stojakovic A, Chang SY, Nesbitt J, Pichurin NP, Ostroot MA, Aikawa T, et al. Partial inhibition of mitochondrial complex i reduces tau pathology and improves energy homeostasis and synaptic function in 3xTg-AD mice. J Alzheimers Dis. 2021;79(1):335–353. doi: 10.3233/JAD-201015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jadiya P, Kolmetzky DW, Tomar D, Di Meco A, Lombardi AA, Lambert JP, et al. Impaired mitochondrial calcium efflux contributes to disease progression in models of Alzheimer's disease. Nat Commun. 2019;10(1):3885. doi: 10.1038/s41467-019-11813-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kubik LL, Philbert MA. The role of astrocyte mitochondria in differential regional susceptibility to environmental neurotoxicants: tools for understanding neurodegeneration. Toxicol Sci. 2015;144(1):7–16. doi: 10.1093/toxsci/kfu254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Dan Dunn J, Alvarez LA, Zhang X, Soldati T. Reactive oxygen species and mitochondria: a nexus of cellular homeostasis. Redox Biol. 2015;6:472–485. doi: 10.1016/j.redox.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Park MW, Cha HW, Kim J, Kim JH, Yang H, Yoon S, et al. NOX4 promotes ferroptosis of astrocytes by oxidative stress-induced lipid peroxidation via the impairment of mitochondrial metabolism in Alzheimer's diseases. Redox Biol. 2021;41:101947. doi: 10.1016/j.redox.2021.101947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Zhu L, Luo X, Fu N, Chen L. Mitochondrial unfolded protein response: a novel pathway in metabolism and immunity. Pharmacol Res. 2021;168:105603. doi: 10.1016/j.phrs.2021.105603. [DOI] [PubMed] [Google Scholar]
- 128.Zhu L, Zhou Q, He L, Chen L. Mitochondrial unfolded protein response: an emerging pathway in human diseases. Free Radic Biol Med. 2021;163:125–134. doi: 10.1016/j.freeradbiomed.2020.12.013. [DOI] [PubMed] [Google Scholar]
- 129.Shen Y, Ding M, Xie Z, Liu X, Yang H, Jin S, et al. Activation of mitochondrial unfolded protein response in SHSY5Y expressing APP cells and APP/PS1 mice. Front Cell Neurosci. 2019;13:568. doi: 10.3389/fncel.2019.00568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Yang W, Zou Y, Zhang M, Zhao N, Tian Q, Gu M, et al. Mitochondrial Sirt3 expression is decreased in APP/PS1 double transgenic mouse model of Alzheimer's disease. Neurochem Res. 2015;40(8):1576–1582. doi: 10.1007/s11064-015-1630-1. [DOI] [PubMed] [Google Scholar]
- 131.Papa L, Germain D. SirT3 regulates the mitochondrial unfolded protein response. Mol Cell Biol. 2014;34(4):699–710. doi: 10.1128/MCB.01337-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Hou M, Bao W, Gao Y, Chen J, Song G. Honokiol improves cognitive impairment in APP/PS1 mice through activating mitophagy and mitochondrial unfolded protein response. Chem Biol Interact. 2022;351:109741. doi: 10.1016/j.cbi.2021.109741. [DOI] [PubMed] [Google Scholar]
- 133.Sorrentino V, Romani M, Mouchiroud L, Beck JS, Zhang H, D'Amico D, et al. Enhancing mitochondrial proteostasis reduces amyloid-β proteotoxicity. Nature. 2017;552(7684):187–193. doi: 10.1038/nature25143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Han S, Zhang M, Jeong YY, Margolis DJ, Cai Q. The role of mitophagy in the regulation of mitochondrial energetic status in neurons. Autophagy. 2021;17(12):4182–4201. doi: 10.1080/15548627.2021.1907167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Yan MH, Wang X, Zhu X. Mitochondrial defects and oxidative stress in Alzheimer disease and Parkinson disease. Free Radic Biol Med. 2013;62:90–101. doi: 10.1016/j.freeradbiomed.2012.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Veurink G, Perry G, Singh SK. Role of antioxidants and a nutrient rich diet in Alzheimer's disease. Open Biol. 2020;10(6):200084. doi: 10.1098/rsob.200084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mao P, Manczak M, Calkins MJ, Truong Q, Reddy TP, Reddy AP, et al. Mitochondria-targeted catalase reduces abnormal APP processing, amyloid β production and BACE1 in a mouse model of Alzheimer's disease: implications for neuroprotection and lifespan extension. Hum Mol Genet. 2012;21(13):2973–2990. doi: 10.1093/hmg/dds128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ng LF, Gruber J, Cheah IK, Goo CK, Cheong WF, Shui G, et al. The mitochondria-targeted antioxidant MitoQ extends lifespan and improves healthspan of a transgenic Caenorhabditis elegans model of Alzheimer disease. Free Radic Biol Med. 2014;71:390–401. doi: 10.1016/j.freeradbiomed.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 139.McManus MJ, Murphy MP, Franklin JL. The mitochondria-targeted antioxidant MitoQ prevents loss of spatial memory retention and early neuropathology in a transgenic mouse model of Alzheimer's disease. J Neurosci. 2011;31(44):15703–15715. doi: 10.1523/JNEUROSCI.0552-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rai SN, Singh C, Singh A, Singh MP, Singh BK. Mitochondrial dysfunction: a potential therapeutic target to treat Alzheimer's disease. Mol Neurobiol. 2020;57(7):3075–3088. doi: 10.1007/s12035-020-01945-y. [DOI] [PubMed] [Google Scholar]
- 141.Li X, Wenes M, Romero P, Huang SC, Fendt SM, Ho PC. Navigating metabolic pathways to enhance antitumour immunity and immunotherapy. Nat Rev Clin Oncol. 2019;16(7):425–441. doi: 10.1038/s41571-019-0203-7. [DOI] [PubMed] [Google Scholar]
- 142.Smith RL, Soeters MR, Wüst RCI, Houtkooper RH. Metabolic flexibility as an adaptation to energy resources and requirements in health and disease. Endocr Rev. 2018;39(4):489–517. doi: 10.1210/er.2017-00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.De Felice FG, Gonçalves RA, Ferreira ST. Impaired insulin signalling and allostatic load in Alzheimer disease. Nat Rev Neurosci. 2022;23(4):215–230. doi: 10.1038/s41583-022-00558-9. [DOI] [PubMed] [Google Scholar]
- 144.Aghanoori MR, Agarwal P, Gauvin E, Nagalingam RS, Bonomo R, Yathindranath V, et al. CEBPβ regulation of endogenous IGF-1 in adult sensory neurons can be mobilized to overcome diabetes-induced deficits in bioenergetics and axonal outgrowth. Cell Mol Life Sci. 2022;79(4):193. doi: 10.1007/s00018-022-04201-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Timper K, Del Río-Martín A, Cremer AL, Bremser S, Alber J, Giavalisco P, et al. GLP-1 receptor signaling in astrocytes regulates fatty acid oxidation, mitochondrial integrity, and function. Cell Metab. 2020;31(6):1189–1205.e1113. doi: 10.1016/j.cmet.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Mai M, Guo X, Huang Y, Zhang W, Xu Y, Zhang Y, et al. DHCR24 knockdown induces tau hyperphosphorylation at Thr181, Ser199, Ser262, and Ser396 sites via activation of the lipid raft-dependent Ras/MEK/ERK signaling pathway in C8D1A astrocytes. Mol Neurobiol. 2022;59(9):5856–5873. doi: 10.1007/s12035-022-02945-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Liu H, Xie Y, Wang X, Abboud MI, Ma C, Ge W, et al. Exploring links between 2-oxoglutarate-dependent oxygenases and Alzheimer's disease. Alzheimers Dement. 2022;18(12):2637–2668. doi: 10.1002/alz.12733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Sędzikowska A, Szablewski L. Insulin and insulin resistance in Alzheimer's disease. Int J Mol Sci. 2021;22(18):9987. doi: 10.3390/ijms22189987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Salama R, Sadaie M, Hoare M, Narita M. Cellular senescence and its effector programs. Genes Dev. 2014;28(2):99–114. doi: 10.1101/gad.235184.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ogrodnik M. Cellular aging beyond cellular senescence: markers of senescence prior to cell cycle arrest in vitro and in vivo. Aging Cell. 2021;20(4):e13338. doi: 10.1111/acel.13338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Hernandez-Segura A, Nehme J, Demaria M. Hallmarks of cellular senescence. Trends Cell Biol. 2018;28(6):436–453. doi: 10.1016/j.tcb.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 152.Wang J, Zheng B, Yang S, Zhou D, Wang J. Olmesartan prevents oligomerized amyloid β (Aβ)-induced cellular senescence in neuronal cells. ACS Chem Neurosci. 2021;12(7):1162–1169. doi: 10.1021/acschemneuro.0c00775. [DOI] [PubMed] [Google Scholar]
- 153.Hu Y, Fryatt GL, Ghorbani M, Obst J, Menassa DA, Martin-Estebane M, et al. Replicative senescence dictates the emergence of disease-associated microglia and contributes to Aβ pathology. Cell Rep. 2021;35(10):109228. doi: 10.1016/j.celrep.2021.109228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Zhang P, Kishimoto Y, Grammatikakis I, Gottimukkala K, Cutler RG, Zhang S, et al. Senolytic therapy alleviates Aβ-associated oligodendrocyte progenitor cell senescence and cognitive deficits in an Alzheimer's disease model. Nat Neurosci. 2019;22(5):719–728. doi: 10.1038/s41593-019-0372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Guadalupe T, Mathias SR, vanErp TGM, Whelan CD, Zwiers MP, Abe Y, et al. Human subcortical brain asymmetries in 15,847 people worldwide reveal effects of age and sex. Brain Imaging Behav. 2017;11(5):1497–1514. doi: 10.1007/s11682-016-9629-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kraig E, Linehan LA, Liang H, Romo TQ, Liu Q, Wu Y, et al. A randomized control trial to establish the feasibility and safety of rapamycin treatment in an older human cohort: immunological, physical performance, and cognitive effects. Exp Gerontol. 2018;105:53–69. doi: 10.1016/j.exger.2017.12.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Mertens J, Herdy JR, Traxler L, Schafer ST, Schlachetzki JCM, Böhnke L, et al. Age-dependent instability of mature neuronal fate in induced neurons from Alzheimer's patients. Cell Stem Cell. 2021;28(9):1533–1548.e1536. doi: 10.1016/j.stem.2021.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Herdy JR, Traxler L, Agarwal RK, Karbacher L, Schlachetzki JCM, Boehnke L, et al. Increased post-mitotic senescence in aged human neurons is a pathological feature of Alzheimer's disease. Cell Stem Cell. 2022;29(12):1637–1652.e1636. doi: 10.1016/j.stem.2022.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Gaikwad S, Puangmalai N, Bittar A, Montalbano M, Garcia S, McAllen S, et al. Tau oligomer induced HMGB1 release contributes to cellular senescence and neuropathology linked to Alzheimer's disease and frontotemporal dementia. Cell Rep. 2021;36(3):109419. doi: 10.1016/j.celrep.2021.109419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Wei Z, Chen XC, Song Y, Pan XD, Dai XM, Zhang J, et al. Amyloid β protein aggravates neuronal senescence and cognitive deficits in 5XFAD mouse model of Alzheimer's disease. Chin Med J (Engl) 2016;129(15):1835–1844. doi: 10.4103/0366-6999.186646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Dehkordi SK, Walker J, Sah E, Bennett E, Atrian F, Frost B, et al. Profiling senescent cells in human brains reveals neurons with CDKN2D/p19 and tau neuropathology. Nat Aging. 2021;1(12):1107–1116. doi: 10.1038/s43587-021-00142-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Chaney AM, Lopez-Picon FR, Serrière S, Wang R, Bochicchio D, Webb SD, et al. Prodromal neuroinflammatory, cholinergic and metabolite dysfunction detected by PET and MRS in the TgF344-AD transgenic rat model of AD: a collaborative multi-modal study. Theranostics. 2021;11(14):6644–6667. doi: 10.7150/thno.56059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Liu L, Watanabe N, Akatsu H, Nishimura M. Neuronal expression of ILEI/FAM3C and its reduction in Alzheimer's disease. Neuroscience. 2016;330:236–246. doi: 10.1016/j.neuroscience.2016.05.050. [DOI] [PubMed] [Google Scholar]
- 164.Varvel NH, Bhaskar K, Patil AR, Pimplikar SW, Herrup K, Lamb BT. Abeta oligomers induce neuronal cell cycle events in Alzheimer's disease. J Neurosci. 2008;28(43):10786–10793. doi: 10.1523/JNEUROSCI.2441-08.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Raina AK, Pardo P, Rottkamp CA, Zhu X, Pereira-Smith OM, Smith MA. Neurons in Alzheimer disease emerge from senescence. Mech Ageing Dev. 2001;123(1):3–9. doi: 10.1016/S0047-6374(01)00333-5. [DOI] [PubMed] [Google Scholar]
- 166.Evans TA, Raina AK, Delacourte A, Aprelikova O, Lee HG, Zhu X, et al. BRCA1 may modulate neuronal cell cycle re-entry in Alzheimer disease. Int J Med Sci. 2007;4(3):140–145. doi: 10.7150/ijms.4.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Bhat R, Crowe EP, Bitto A, Moh M, Katsetos CD, Garcia FU, et al. Astrocyte senescence as a component of Alzheimer's disease. PLoS ONE. 2012;7(9):e45069. doi: 10.1371/journal.pone.0045069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Ungerleider K, Beck J, Lissa D, Turnquist C, Horikawa I, Harris BT, et al. Astrocyte senescence and SASP in neurodegeneration: tau joins the loop. Cell Cycle. 2021;20(8):752–764. doi: 10.1080/15384101.2021.1909260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Middeldorp J, Hol EM. GFAP in health and disease. Prog Neurobiol. 2011;93(3):421–443. doi: 10.1016/j.pneurobio.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 170.Limbad C, Oron TR, Alimirah F, Davalos AR, Tracy TE, Gan L, et al. Astrocyte senescence promotes glutamate toxicity in cortical neurons. PLoS ONE. 2020;15(1):e0227887. doi: 10.1371/journal.pone.0227887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Csipo T, Lipecz A, Ashpole NM, Balasubramanian P, Tarantini S. Astrocyte senescence contributes to cognitive decline. Geroscience. 2020;42(1):51–55. doi: 10.1007/s11357-019-00140-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Turnquist C, Horikawa I, Foran E, Major EO, Vojtesek B, Lane DP, et al. p53 isoforms regulate astrocyte-mediated neuroprotection and neurodegeneration. Cell Death Differ. 2016;23(9):1515–1528. doi: 10.1038/cdd.2016.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Bussian TJ, Aziz A, Meyer CF, Swenson BL, van Deursen JM, Baker DJ. Clearance of senescent glial cells prevents tau-dependent pathology and cognitive decline. Nature. 2018;562(7728):578–582. doi: 10.1038/s41586-018-0543-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Boche D, Gordon MN. Diversity of transcriptomic microglial phenotypes in aging and Alzheimer's disease. Alzheimers Dement. 2022;18(2):360–376. doi: 10.1002/alz.12389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Srinivasan K, Friedman BA, Etxeberria A, Huntley MA, van der Brug MP, Foreman O, et al. Alzheimer's patient microglia exhibit enhanced aging and unique transcriptional activation. Cell Rep. 2020;31(13):107843. doi: 10.1016/j.celrep.2020.107843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Baker DJ, Narita M, Muñoz-Cánoves P. Cellular senescence: beneficial, harmful, and highly complex. FEBS J. 2023;290(5):1156–1160. doi: 10.1111/febs.16735. [DOI] [PubMed] [Google Scholar]
- 177.Rustenhoven J, Aalderink M, Scotter EL, Oldfield RL, Bergin PS, Mee EW, et al. TGF-beta1 regulates human brain pericyte inflammatory processes involved in neurovasculature function. J Neuroinflammation. 2016;13:37. doi: 10.1186/s12974-016-0503-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hu Y, Huang Y, Xing S, Chen C, Shen D, Chen J. Aβ promotes CD38 expression in senescent microglia in Alzheimer's disease. Biol Res. 2022;55(1):10. doi: 10.1186/s40659-022-00379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.An Y, Li Y, Hou Y, Huang S, Pei G. Alzheimer's amyloid-β accelerates cell senescence and suppresses the SIRT1/NRF2 pathway in human microglial cells. Oxid Med Cell Longev. 2022;2022:3086010. doi: 10.1155/2022/3086010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Zhang X, Wang R, Chen H, Jin C, Jin Z, Lu J, et al. Aged microglia promote peripheral T cell infiltration by reprogramming the microenvironment of neurogenic niches. Immun Ageing. 2022;19(1):34. doi: 10.1186/s12979-022-00289-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.He GL, Liu Y, Li M, Chen CH, Gao P, Yu ZP, et al. The amelioration of phagocytic ability in microglial cells by curcumin through the inhibition of EMF-induced pro-inflammatory responses. J Neuroinflammation. 2014;11:49. doi: 10.1186/1742-2094-11-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Luo G, Wang X, Cui Y, Cao Y, Zhao Z, Zhang J. Metabolic reprogramming mediates hippocampal microglial M1 polarization in response to surgical trauma causing perioperative neurocognitive disorders. J Neuroinflammation. 2021;18(1):267. doi: 10.1186/s12974-021-02318-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Ulland TK, Song WM, Huang SC, Ulrich JD, Sergushichev A, Beatty WL, et al. TREM2 maintains microglial metabolic fitness in Alzheimer's disease. Cell. 2017;170(4):649–663.e613. doi: 10.1016/j.cell.2017.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Yoo Y, Neumayer G, Shibuya Y, Mader MM, Wernig M. A cell therapy approach to restore microglial Trem2 function in a mouse model of Alzheimer's disease. Cell Stem Cell. 2023;30(8):1043–1053.e1046. doi: 10.1016/j.stem.2023.07.006. [DOI] [PubMed] [Google Scholar]
- 185.Kaya T, Mattugini N, Liu L, Ji H, Cantuti-Castelvetri L, Wu J, et al. CD8(+) T cells induce interferon-responsive oligodendrocytes and microglia in white matter aging. Nat Neurosci. 2022;25(11):1446–1457. doi: 10.1038/s41593-022-01183-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Rodrigues LP, Teixeira VR, Alencar-Silva T, Simonassi-Paiva B, Pereira RW, Pogue R, et al. Hallmarks of aging and immunosenescence: connecting the dots. Cytokine Growth Factor Rev. 2021;59:9–21. doi: 10.1016/j.cytogfr.2021.01.006. [DOI] [PubMed] [Google Scholar]
- 187.Gemechu JM, Bentivoglio M. T cell recruitment in the brain during normal aging. Front Cell Neurosci. 2012;6:38. doi: 10.3389/fncel.2012.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Kiss T, Nyúl-Tóth Á, Balasubramanian P, Tarantini S, Ahire C, DelFavero J, et al. Single-cell RNA sequencing identifies senescent cerebromicrovascular endothelial cells in the aged mouse brain. Geroscience. 2020;42(2):429–444. doi: 10.1007/s11357-020-00177-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Bryant AG, Hu M, Carlyle BC, Arnold SE, Frosch MP, Das S, et al. Cerebrovascular senescence is associated with tau pathology in Alzheimer's disease. Front Neurol. 2020;11:575953. doi: 10.3389/fneur.2020.575953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Li Y, Lu J, Hou Y, Huang S, Pei G. Alzheimer's amyloid-β accelerates human neuronal cell senescence which could be rescued by Sirtuin-1 and Aspirin. Front Cell Neurosci. 2022;16:906270. doi: 10.3389/fncel.2022.906270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Blanpain C, Fuchs E. Stem cell plasticity. Plasticity of epithelial stem cells in tissue regeneration. Science. 2014;344(6189):1242281. doi: 10.1126/science.1242281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Oh J, Lee YD, Wagers AJ. Stem cell aging: mechanisms, regulators and therapeutic opportunities. Nat Med. 2014;20(8):870–880. doi: 10.1038/nm.3651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kalamakis G, Brüne D, Ravichandran S, Bolz J, Fan W, Ziebell F, et al. Quiescence modulates stem cell maintenance and regenerative capacity in the aging brain. Cell. 2019;176(6):1407–1419.e1414. doi: 10.1016/j.cell.2019.01.040. [DOI] [PubMed] [Google Scholar]
- 194.Xiao YZ, Yang M, Xiao Y, Guo Q, Huang Y, Li CJ, et al. Reducing hypothalamic stem cell senescence protects against aging-associated physiological decline. Cell Metab. 2020;31(3):534–548.e535. doi: 10.1016/j.cmet.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 195.Sarkar TJ, Quarta M, Mukherjee S, Colville A, Paine P, Doan L, et al. Transient non-integrative expression of nuclear reprogramming factors promotes multifaceted amelioration of aging in human cells. Nat Commun. 2020;11(1):1545. doi: 10.1038/s41467-020-15174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Haag D, Mack N, Benites Goncalves da Silva P, Statz B, Clark J, Tanabe K, et al. H3.3–K27M drives neural stem cell-specific gliomagenesis in a human iPSC-derived model. Cancer Cell. 2021;39(3):407–422. doi: 10.1016/j.ccell.2021.01.005. [DOI] [PubMed] [Google Scholar]
- 197.Kim J, Han D, Byun SH, Kwon M, Cho JY, Pleasure SJ, et al. Ttyh1 regulates embryonic neural stem cell properties by enhancing the Notch signaling pathway. EMBO Rep. 2018;19(11):e45472. doi: 10.15252/embr.201745472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Cao Y, Wu HN, Cao XL, Yue KY, Han WJ, Cao ZP, et al. Transmembrane protein Ttyh1 maintains the quiescence of neural stem cells through Ca(2+)/NFATc3 signaling. Front Cell Dev Biol. 2021;9:779373. doi: 10.3389/fcell.2021.779373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Dulken BW, Buckley MT, Navarro Negredo P, Saligrama N, Cayrol R, Leeman DS, et al. Single-cell analysis reveals T cell infiltration in old neurogenic niches. Nature. 2019;571(7764):205–210. doi: 10.1038/s41586-019-1362-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lee IS, Jung K, Kim IS, Park KI. Amyloid-β oligomers regulate the properties of human neural stem cells through GSK-3β signaling. Exp Mol Med. 2013;45(11):e60. doi: 10.1038/emm.2013.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Kirkland JL, Tchkonia T. Cellular senescence: a translational perspective. EBioMedicine. 2017;21:21–28. doi: 10.1016/j.ebiom.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Srivastava T, Diba P, Dean JM, Banine F, Shaver D, Hagen M, et al. A TLR/AKT/FoxO3 immune tolerance-like pathway disrupts the repair capacity of oligodendrocyte progenitors. J Clin Investig. 2018;128(5):2025–2041. doi: 10.1172/JCI94158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Vanzulli I, Papanikolaou M, De-La-Rocha IC, Pieropan F, Rivera AD, Gomez-Nicola D, et al. Disruption of oligodendrocyte progenitor cells is an early sign of pathology in the triple transgenic mouse model of Alzheimer's disease. Neurobiol Aging. 2020;94:130–139. doi: 10.1016/j.neurobiolaging.2020.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Liu B, Ghosh S, Yang X, Zheng H, Liu X, Wang Z, et al. Resveratrol rescues SIRT1-dependent adult stem cell decline and alleviates progeroid features in laminopathy-based progeria. Cell Metab. 2012;16(6):738–750. doi: 10.1016/j.cmet.2012.11.007. [DOI] [PubMed] [Google Scholar]
- 205.Zhou Z, Shi B, Xu Y, Zhang J, Liu X, Zhou X, et al. Neural stem/progenitor cell therapy for Alzheimer disease in preclinical rodent models: a systematic review and meta-analysis. Stem Cell Res Ther. 2023;14(1):3. doi: 10.1186/s13287-022-03231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Duncan T, Valenzuela M. Alzheimer's disease, dementia, and stem cell therapy. Stem Cell Res Ther. 2017;8(1):111. doi: 10.1186/s13287-017-0567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Yin Y, Chen H, Wang Y, Zhang L, Wang X. Roles of extracellular vesicles in the aging microenvironment and age-related diseases. J Extracell Vesicles. 2021;10(12):e12154. doi: 10.1002/jev2.12154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Phillips RA, 3rd, Tuscher JJ, Black SL, Andraka E, Fitzgerald ND, Ianov L, et al. An atlas of transcriptionally defined cell populations in the rat ventral tegmental area. Cell Rep. 2022;39(1):110616. doi: 10.1016/j.celrep.2022.110616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Rudy CC, Hunsberger HC, Weitzner DS, Reed MN. The role of the tripartite glutamatergic synapse in the pathophysiology of Alzheimer's disease. Aging Dis. 2015;6(2):131–148. doi: 10.14336/AD.2014.0423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Shao F, Wang M, Guo Q, Zhang B, Wang X. Characterization of Alzheimer's disease-associated excitatory neurons via single-cell RNA sequencing analysis. Front Aging Neurosci. 2021;13:742176. doi: 10.3389/fnagi.2021.742176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Habib N, McCabe C, Medina S, Varshavsky M, Kitsberg D, Dvir-Szternfeld R, et al. Disease-associated astrocytes in Alzheimer's disease and aging. Nat Neurosci. 2020;23(6):701–706. doi: 10.1038/s41593-020-0624-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Qi G, Mi Y, Shi X, Gu H, Brinton RD, Yin F. ApoE4 impairs neuron-astrocyte coupling of fatty acid metabolism. Cell Rep. 2021;34(1):108572. doi: 10.1016/j.celrep.2020.108572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Andersen JV, Schousboe A, Verkhratsky A. Astrocyte energy and neurotransmitter metabolism in Alzheimer's disease: integration of the glutamate/GABA-glutamine cycle. Prog Neurobiol. 2022;217:102331. doi: 10.1016/j.pneurobio.2022.102331. [DOI] [PubMed] [Google Scholar]
- 214.Xu YZ, Nygård M, Kristensson K, Bentivoglio M. Regulation of cytokine signaling and T-cell recruitment in the aging mouse brain in response to central inflammatory challenge. Brain Behav Immun. 2010;24(1):138–152. doi: 10.1016/j.bbi.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 215.Silvin A, Uderhardt S, Piot C, Da Mesquita S, Yang K, Geirsdottir L, et al. Dual ontogeny of disease-associated microglia and disease inflammatory macrophages in aging and neurodegeneration. Immunity. 2022;55(8):1448–1465.e1446. doi: 10.1016/j.immuni.2022.07.004. [DOI] [PubMed] [Google Scholar]
- 216.Fahrenhold M, Rakic S, Classey J, Brayne C, Ince PG, Nicoll JAR, et al. TREM2 expression in the human brain: a marker of monocyte recruitment? Brain Pathol. 2018;28(5):595–602. doi: 10.1111/bpa.12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Bowman GL, Dayon L, Kirkland R, Wojcik J, Peyratout G, Severin IC, et al. Blood-brain barrier breakdown, neuroinflammation, and cognitive decline in older adults. Alzheimers Dement. 2018;14(12):1640–1650. doi: 10.1016/j.jalz.2018.06.2857. [DOI] [PubMed] [Google Scholar]
- 218.Yang AC, Vest RT, Kern F, Lee DP, Agam M, Maat CA, et al. A human brain vascular atlas reveals diverse mediators of Alzheimer's risk. Nature. 2022;603(7903):885–892. doi: 10.1038/s41586-021-04369-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Ishii M, Iadecola C. Risk factor for Alzheimer's disease breaks the blood-brain barrier. Nature. 2020;581(7806):31–32. doi: 10.1038/d41586-020-01152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Varatharaj A, Galea I. The blood-brain barrier in systemic inflammation. Brain Behav Immun. 2017;60:1–12. doi: 10.1016/j.bbi.2016.03.010. [DOI] [PubMed] [Google Scholar]
- 221.Parker KR, Migliorini D, Perkey E, Yost KE, Bhaduri A, Bagga P, et al. Single-cell analyses identify brain mural cells expressing CD19 as potential off-tumor targets for CAR-T immunotherapies. Cell. 2020;183(1):126–142.e117. doi: 10.1016/j.cell.2020.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Da Mesquita S, Papadopoulos Z, Dykstra T, Brase L, Farias FG, Wall M, et al. Meningeal lymphatics affect microglia responses and anti-Aβ immunotherapy. Nature. 2021;593(7858):255–260. doi: 10.1038/s41586-021-03489-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Frederick N, Louveau A. Meningeal lymphatics, immunity and neuroinflammation. Curr Opin Neurobiol. 2020;62:41–47. doi: 10.1016/j.conb.2019.11.010. [DOI] [PubMed] [Google Scholar]
- 224.Louveau A, Plog BA, Antila S, Alitalo K, Nedergaard M, Kipnis J. Understanding the functions and relationships of the glymphatic system and meningeal lymphatics. J Clin Investig. 2017;127(9):3210–3219. doi: 10.1172/JCI90603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Wu Y, Zhang T, Li X, Wei Y, Li X, Wang S, et al. Borneol-driven meningeal lymphatic drainage clears amyloid-β peptide to attenuate Alzheimer-like phenotype in mice. Theranostics. 2023;13(1):106–124. doi: 10.7150/thno.76133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Petkovic M, O'Brien CE, Jan YN. Interorganelle communication, aging, and neurodegeneration. Genes Dev. 2021;35(7–8):449–469. doi: 10.1101/gad.346759.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Gu W, Ni Z, Tan YQ, Deng J, Zhang SJ, Lv ZC, et al. Adventitial cell atlas of wt (wild type) and ApoE (Apolipoprotein E)-deficient mice defined by single-cell RNA sequencing. Arterioscler Thromb Vasc Biol. 2019;39(6):1055–1071. doi: 10.1161/ATVBAHA.119.312399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Das R, Chinnathambi S. Microglial priming of antigen presentation and adaptive stimulation in Alzheimer's disease. Cell Mol Life Sci. 2019;76(19):3681–3694. doi: 10.1007/s00018-019-03132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Erny D, Dokalis N, Mezö C, Castoldi A, Mossad O, Staszewski O, et al. Microbiota-derived acetate enables the metabolic fitness of the brain innate immune system during health and disease. Cell Metab. 2021;33(11):2260–2276.e2267. doi: 10.1016/j.cmet.2021.10.010. [DOI] [PubMed] [Google Scholar]
- 230.Sun Y, Zhang H, Zhang X, Wang W, Chen Y, Cai Z, et al. Promotion of astrocyte-neuron glutamate-glutamine shuttle by SCFA contributes to the alleviation of Alzheimer's disease. Redox Biol. 2023;62:102690. doi: 10.1016/j.redox.2023.102690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Leng F, Edison P. Neuroinflammation and microglial activation in Alzheimer disease: where do we go from here? Nat Rev Neurol. 2021;17(3):157–172. doi: 10.1038/s41582-020-00435-y. [DOI] [PubMed] [Google Scholar]
- 232.Uyar B, Palmer D, Kowald A, Murua Escobar H, Barrantes I, Möller S, et al. Single-cell analyses of aging, inflammation and senescence. Ageing Res Rev. 2020;64:101156. doi: 10.1016/j.arr.2020.101156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Neumann A, Küçükali F, Bos I, Vos SJB, Engelborghs S, De Pooter T, et al. Rare variants in IFFO1, DTNB, NLRC3 and SLC22A10 associate with Alzheimer's disease CSF profile of neuronal injury and inflammation. Mol Psychiatry. 2022;27(4):1990–1999. doi: 10.1038/s41380-022-01437-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Da Mesquita S, Louveau A, Vaccari A, Smirnov I, Cornelison RC, Kingsmore KM, et al. Functional aspects of meningeal lymphatics in ageing and Alzheimer's disease. Nature. 2018;560(7717):185–191. doi: 10.1038/s41586-018-0368-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Rayon-Estrada V, Harjanto D, Hamilton CE, Berchiche YA, Gantman EC, Sakmar TP, et al. Epitranscriptomic profiling across cell types reveals associations between APOBEC1-mediated RNA editing, gene expression outcomes, and cellular function. Proc Natl Acad Sci USA. 2017;114(50):13296–13301. doi: 10.1073/pnas.1714227114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Cole DC, Chung Y, Gagnidze K, Hajdarovic KH, Rayon-Estrada V, Harjanto D, et al. Loss of APOBEC1 RNA-editing function in microglia exacerbates age-related CNS pathophysiology. Proc Natl Acad Sci USA. 2017;114(50):13272–13277. doi: 10.1073/pnas.1710493114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Morganti JM, Riparip LK, Chou A, Liu S, Gupta N, Rosi S. Age exacerbates the CCR2/5-mediated neuroinflammatory response to traumatic brain injury. J Neuroinflammation. 2016;13(1):80. doi: 10.1186/s12974-016-0547-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Baik SH, Kang S, Lee W, Choi H, Chung S, Kim JI, et al. A breakdown in metabolic reprogramming causes microglia dysfunction in Alzheimer's disease. Cell Metab. 2019;30(3):493–507.e496. doi: 10.1016/j.cmet.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 239.Jaturapatporn D, Isaac MG, McCleery J, Tabet N. Aspirin, steroidal and non-steroidal anti-inflammatory drugs for the treatment of Alzheimer's disease. Cochrane Database Syst Rev. 2012;2:Cd006378. doi: 10.1002/14651858.CD006378.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.MahmoudianDehkordi S, Arnold M, Nho K, Ahmad S, Jia W, Xie G, et al. Altered bile acid profile associates with cognitive impairment in Alzheimer's disease: an emerging role for gut microbiome. Alzheimers Dement. 2019;15(1):76–92. doi: 10.1016/j.jalz.2018.07.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Megur A, Baltriukienė D, Bukelskienė V, Burokas A. The microbiota-gut-brain axis and Alzheimer's disease: neuroinflammation is to blame? Nutrients. 2020;13(1):37. doi: 10.3390/nu13010037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Shabbir U, Arshad MS, Sameen A, Oh DH. Crosstalk between gut and brain in Alzheimer's disease: the role of gut microbiota modulation strategies. Nutrients. 2021;13(2):690. doi: 10.3390/nu13020690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Chen C, Ahn EH, Kang SS, Liu X, Alam A, Ye K. Gut dysbiosis contributes to amyloid pathology, associated with C/EBPβ/AEP signaling activation in Alzheimer's disease mouse model. Sci Adv. 2020;6(31):eaba0466. doi: 10.1126/sciadv.aba0466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Chen C, Liao J, Xia Y, Liu X, Jones R, Haran J, et al. Gut microbiota regulate Alzheimer's disease pathologies and cognitive disorders via PUFA-associated neuroinflammation. Gut. 2022;71(11):2233–2252. doi: 10.1136/gutjnl-2021-326269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Wang X, Sun G, Feng T, Zhang J, Huang X, Wang T, et al. Sodium oligomannate therapeutically remodels gut microbiota and suppresses gut bacterial amino acids-shaped neuroinflammation to inhibit Alzheimer's disease progression. Cell Res. 2019;29(10):787–803. doi: 10.1038/s41422-019-0216-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Chen L, Cao H, Wu X, Xu X, Ji X, Wang B, et al. Effects of oral health intervention strategies on cognition and microbiota alterations in patients with mild Alzheimer's disease: a randomized controlled trial. Geriatr Nurs. 2022;48:103–110. doi: 10.1016/j.gerinurse.2022.09.005. [DOI] [PubMed] [Google Scholar]
- 247.Olsen I, Taubman MA, Singhrao SK. Porphyromonas gingivalis suppresses adaptive immunity in periodontitis, atherosclerosis, and Alzheimer's disease. J Oral Microbiol. 2016;8:33029. doi: 10.3402/jom.v8.33029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Dominy SS, Lynch C, Ermini F, Benedyk M, Marczyk A, Konradi A, et al. Porphyromonas gingivalis in Alzheimer's disease brains: evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019;5(1):eaau3333. doi: 10.1126/sciadv.aau3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Itzhaki RF, Golde TE, Heneka MT, Readhead B. Do infections have a role in the pathogenesis of Alzheimer disease? Nat Rev Neurol. 2020;16(4):193–197. doi: 10.1038/s41582-020-0323-9. [DOI] [PubMed] [Google Scholar]
- 250.Nemergut M, Batkova T, Vigasova D, Bartos M, Hlozankova M, Schenkmayerova A, et al. Increased occurrence of Treponema spp. and double-species infections in patients with Alzheimer's disease. Sci Total Environ. 2022;844:157114. doi: 10.1016/j.scitotenv.2022.157114. [DOI] [PubMed] [Google Scholar]
- 251.Sochocka M, Zwolińska K, Leszek J. The infectious etiology of Alzheimer's disease. Curr Neuropharmacol. 2017;15(7):996–1009. doi: 10.2174/1570159X15666170313122937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Panza F, Lozupone M, Solfrizzi V, Watling M, Imbimbo BP. Time to test antibacterial therapy in Alzheimer's disease. Brain. 2019;142(10):2905–2929. doi: 10.1093/brain/awz244. [DOI] [PubMed] [Google Scholar]
- 253.Qiu S, Joshi PS, Miller MI, Xue C, Zhou X, Karjadi C, et al. Development and validation of an interpretable deep learning framework for Alzheimer's disease classification. Brain. 2020;143(6):1920–1933. doi: 10.1093/brain/awaa137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Sekula P, Del Greco MF, Pattaro C, Köttgen A. Mendelian randomization as an approach to assess causality using observational data. J Am Soc Nephrol. 2016;27(11):3253–3265. doi: 10.1681/ASN.2016010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Gao K, Wei C, Zhu J, Wang X, Chen G, Luo Y, et al. Exploring the causal pathway from telomere length to Alzheimer's disease: an update mendelian randomization study. Front Psychiatry. 2019;10:843. doi: 10.3389/fpsyt.2019.00843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Rodríguez-Fernández B, Gispert JD, Guigo R, Navarro A, Vilor-Tejedor N, Crous-Bou M. Genetically predicted telomere length and its relationship with neurodegenerative diseases and life expectancy. Comput Struct Biotechnol J. 2022;20:4251–4256. doi: 10.1016/j.csbj.2022.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Johnson MB, Wang PP, Atabay KD, Murphy EA, Doan RN, Hecht JL, et al. Single-cell analysis reveals transcriptional heterogeneity of neural progenitors in human cortex. Nat Neurosci. 2015;18(5):637–646. doi: 10.1038/nn.3980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.Sadick JS, O'Dea MR, Hasel P, Dykstra T, Faustin A, Liddelow SA. Astrocytes and oligodendrocytes undergo subtype-specific transcriptional changes in Alzheimer's disease. Neuron. 2022;110(11):1788–1805.e1710. doi: 10.1016/j.neuron.2022.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Mathys H, Davila-Velderrain J, Peng Z, Gao F, Mohammadi S, Young JZ, et al. Single-cell transcriptomic analysis of Alzheimer's disease. Nature. 2019;570(7761):332–337. doi: 10.1038/s41586-019-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Gate D, Saligrama N, Leventhal O, Yang AC, Unger MS, Middeldorp J, et al. Clonally expanded CD8 T cells patrol the cerebrospinal fluid in Alzheimer's disease. Nature. 2020;577(7790):399–404. doi: 10.1038/s41586-019-1895-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Walgrave H, Balusu S, Snoeck S, Vanden Eynden E, Craessaerts K, Thrupp N, et al. Restoring miR-132 expression rescues adult hippocampal neurogenesis and memory deficits in Alzheimer's disease. Cell Stem Cell. 2021;28(10):1805–1821.e1808. doi: 10.1016/j.stem.2021.05.001. [DOI] [PubMed] [Google Scholar]
- 262.Morabito S, Miyoshi E, Michael N, Shahin S, Martini AC, Head E, et al. Single-nucleus chromatin accessibility and transcriptomic characterization of Alzheimer's disease. Nat Genet. 2021;53(8):1143–1155. doi: 10.1038/s41588-021-00894-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Wang M, Song WM, Ming C, Wang Q, Zhou X, Xu P, et al. Guidelines for bioinformatics of single-cell sequencing data analysis in Alzheimer's disease: review, recommendation, implementation and application. Mol Neurodegener. 2022;17(1):17. doi: 10.1186/s13024-022-00517-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Keren-Shaul H, Spinrad A, Weiner A, Matcovitch-Natan O, Dvir-Szternfeld R, Ulland TK, et al. A Unique microglia type associated with restricting development of Alzheimer's disease. Cell. 2017;169(7):1276–1290.e1217. doi: 10.1016/j.cell.2017.05.018. [DOI] [PubMed] [Google Scholar]
- 265.Mathys H, Adaikkan C, Gao F, Young JZ, Manet E, Hemberg M, et al. Temporal tracking of microglia activation in neurodegeneration at single-cell resolution. Cell Rep. 2017;21(2):366–380. doi: 10.1016/j.celrep.2017.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Cosacak MI, Bhattarai P, Reinhardt S, Petzold A, Dahl A, Zhang Y, et al. Single-cell transcriptomics analyses of neural stem cell heterogeneity and contextual plasticity in a zebrafish brain model of amyloid toxicity. Cell Rep. 2019;27(4):1307–1318.e1303. doi: 10.1016/j.celrep.2019.03.090. [DOI] [PubMed] [Google Scholar]
- 267.Zhong S, Wang M, Zhan Y, Zhang J, Yang X, Fu S, et al. Single-nucleus RNA sequencing reveals transcriptional changes of hippocampal neurons in APP23 mouse model of Alzheimer's disease. Biosci Biotechnol Biochem. 2020;84(5):919–926. doi: 10.1080/09168451.2020.1714420. [DOI] [PubMed] [Google Scholar]
- 268.Xu H, Jia J. Single-cell RNA sequencing of peripheral blood reveals immune cell signatures in Alzheimer's disease. Front Immunol. 2021;12:645666. doi: 10.3389/fimmu.2021.645666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Leng K, Li E, Eser R, Piergies A, Sit R, Tan M, et al. Molecular characterization of selectively vulnerable neurons in Alzheimer's disease. Nat Neurosci. 2021;24(2):276–287. doi: 10.1038/s41593-020-00764-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Lee SH, Rezzonico MG, Friedman BA, Huntley MH, Meilandt WJ, Pandey S, et al. TREM2-independent oligodendrocyte, astrocyte, and T cell responses to tau and amyloid pathology in mouse models of Alzheimer disease. Cell Rep. 2021;37(13):110158. doi: 10.1016/j.celrep.2021.110158. [DOI] [PubMed] [Google Scholar]
- 271.Freitag K, Sterczyk N, Wendlinger S, Obermayer B, Schulz J, Farztdinov V, et al. Spermidine reduces neuroinflammation and soluble amyloid beta in an Alzheimer's disease mouse model. J Neuroinflammation. 2022;19(1):172. doi: 10.1186/s12974-022-02534-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Lampinen R, Fazaludeen MF, Avesani S, Örd T, Penttilä E, Lehtola JM, et al. Single-cell RNA-Seq analysis of olfactory mucosal cells of Alzheimer's disease patients. Cells. 2022;11(4):676. doi: 10.3390/cells11040676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Wood JI, Wong E, Joghee R, Balbaa A, Vitanova KS, Stringer KM, et al. Plaque contact and unimpaired Trem2 is required for the microglial response to amyloid pathology. Cell Rep. 2022;41(8):111686. doi: 10.1016/j.celrep.2022.111686. [DOI] [PubMed] [Google Scholar]
- 274.Rao A, Barkley D, França GS, Yanai I. Exploring tissue architecture using spatial transcriptomics. Nature. 2021;596(7871):211–220. doi: 10.1038/s41586-021-03634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Allen WE, Blosser TR, Sullivan ZA, Dulac C, Zhuang X. Molecular and spatial signatures of mouse brain aging at single-cell resolution. Cell. 2023;186(1):194–208.e118. doi: 10.1016/j.cell.2022.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Chen WT, Lu A, Craessaerts K, Pavie B, Sala Frigerio C, Corthout N, et al. Spatial transcriptomics and in situ sequencing to study Alzheimer's disease. Cell. 2020;182(4):976–991.e919. doi: 10.1016/j.cell.2020.06.038. [DOI] [PubMed] [Google Scholar]
- 277.Fan Z, Luo Y, Lu H, Wang T, Feng Y, Zhao W, et al. SPASCER: spatial transcriptomics annotation at single-cell resolution. Nucleic Acids Res. 2023;51(D1):D1138–d1149. doi: 10.1093/nar/gkac889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Lundberg E, Borner GHH. Spatial proteomics: a powerful discovery tool for cell biology. Nat Rev Mol Cell Biol. 2019;20(5):285–302. doi: 10.1038/s41580-018-0094-y. [DOI] [PubMed] [Google Scholar]
- 279.Prokop S, Miller KR, Labra SR, Pitkin RM, Hoxha K, Narasimhan S, et al. Impact of TREM2 risk variants on brain region-specific immune activation and plaque microenvironment in Alzheimer's disease patient brain samples. Acta Neuropathol. 2019;138(4):613–630. doi: 10.1007/s00401-019-02048-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Mund A, Coscia F, Kriston A, Hollandi R, Kovács F, Brunner AD, et al. Deep Visual Proteomics defines single-cell identity and heterogeneity. Nat Biotechnol. 2022;40(8):1231–1240. doi: 10.1038/s41587-022-01302-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Walker JM, Kazempour Dehkordi S, Fracassi A, Vanschoiack A, Pavenko A, Taglialatela G, et al. Differential protein expression in the hippocampi of resilient individuals identified by digital spatial profiling. Acta Neuropathol Commun. 2022;10(1):23. doi: 10.1186/s40478-022-01324-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Vijayaragavan K, Cannon BJ, Tebaykin D, Bossé M, Baranski A, Oliveria JP, et al. Single-cell spatial proteomic imaging for human neuropathology. Acta Neuropathol Commun. 2022;10(1):158. doi: 10.1186/s40478-022-01465-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Shahidehpour RK, Nelson AS, Sanders LG, Embry CR, Nelson PT, Bachstetter AD. The localization of molecularly distinct microglia populations to Alzheimer's disease pathologies using QUIVER. Acta Neuropathol Commun. 2023;11(1):45. doi: 10.1186/s40478-023-01541-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Bhatia HS, Brunner AD, Öztürk F, Kapoor S, Rong Z, Mai H, et al. Spatial proteomics in three-dimensional intact specimens. Cell. 2022;185(26):5040–5058.e5019. doi: 10.1016/j.cell.2022.11.021. [DOI] [PubMed] [Google Scholar]
- 285.Ben-Chetrit N, Niu X, Swett AD, Sotelo J, Jiao MS, Stewart CM, et al. Integration of whole transcriptome spatial profiling with protein markers. Nat Biotechnol. 2023;41(6):788–793. doi: 10.1038/s41587-022-01536-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Vandereyken K, Sifrim A, Thienpont B, Voet T. Methods and applications for single-cell and spatial multi-omics. Nat Rev Genet. 2023;24(8):494–515. doi: 10.1038/s41576-023-00580-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Wang Y, Tong Q, Ma SR, Zhao ZX, Pan LB, Cong L, et al. Oral berberine improves brain dopa/dopamine levels to ameliorate Parkinson's disease by regulating gut microbiota. Signal Transduct Target Ther. 2021;6(1):77. doi: 10.1038/s41392-020-00456-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Dal Co A, Ackermann M, van Vliet S. Spatial self-organization of metabolism in microbial systems: a matter of enzymes and chemicals. Cell Syst. 2023;14(2):98–108. doi: 10.1016/j.cels.2022.12.009. [DOI] [PubMed] [Google Scholar]
- 289.Yuan Z, Zhou Q, Cai L, Pan L, Sun W, Qumu S, et al. SEAM is a spatial single nuclear metabolomics method for dissecting tissue microenvironment. Nat Methods. 2021;18(10):1223–1232. doi: 10.1038/s41592-021-01276-3. [DOI] [PubMed] [Google Scholar]
- 290.Korologou-Linden R, Bhatta L, Brumpton BM, Howe LD, Millard LAC, Kolaric K, et al. The causes and consequences of Alzheimer's disease: phenome-wide evidence from Mendelian randomization. Nat Commun. 2022;13(1):4726. doi: 10.1038/s41467-022-32183-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Viejo L, Noori A, Merrill E, Das S, Hyman BT, Serrano-Pozo A. Systematic review of human post-mortem immunohistochemical studies and bioinformatics analyses unveil the complexity of astrocyte reaction in Alzheimer's disease. Neuropathol Appl Neurobiol. 2022;48(1):e12753. doi: 10.1111/nan.12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Aerqin Q, Wang ZT, Wu KM, He XY, Dong Q, Yu JT. Omics-based biomarkers discovery for Alzheimer's disease. Cell Mol Life Sci. 2022;79(12):585. doi: 10.1007/s00018-022-04614-6. [DOI] [PubMed] [Google Scholar]
- 293.Cohn W, Melnik M, Huang C, Teter B, Chandra S, Zhu C, et al. Multi-omics analysis of microglial extracellular vesicles from human Alzheimer's disease brain tissue reveals disease-associated signatures. Front Pharmacol. 2021;12:766082. doi: 10.3389/fphar.2021.766082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Clark C, Dayon L, Masoodi M, Bowman GL, Popp J. An integrative multi-omics approach reveals new central nervous system pathway alterations in Alzheimer's disease. Alzheimers Res Ther. 2021;13(1):71. doi: 10.1186/s13195-021-00814-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Cummings J, Lee G, Nahed P, Kambar M, Zhong K, Fonseca J, et al. Alzheimer's disease drug development pipeline: 2022. Alzheimers Dement. 2022;8(1):e12295. doi: 10.1002/trc2.12295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Gong B, Ji W, Chen X, Li P, Cheng W, Zhao Y, et al. Recent advancements in strategies for abnormal protein clearance in Alzheimer's disease. Mini Rev Med Chem. 2022;22(17):2260–2270. doi: 10.2174/1389557522666220214092824. [DOI] [PubMed] [Google Scholar]
- 297.Šimić G, Babić Leko M, Wray S, Harrington C, Delalle I, Jovanov-Milošević N, et al. Tau protein hyperphosphorylation and aggregation in Alzheimer's disease and other tauopathies, and possible neuroprotective strategies. Biomolecules. 2016;6(1):6. doi: 10.3390/biom6010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Vitek GE, Decourt B, Sabbagh MN. Lecanemab (BAN2401): an anti-beta-amyloid monoclonal antibody for the treatment of Alzheimer disease. Expert Opin Investig Drugs. 2023;32:89–94. doi: 10.1080/13543784.2023.2178414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in early Alzheimer's disease. N Engl J Med. 2023;388(1):9–21. doi: 10.1056/NEJMoa2212948. [DOI] [PubMed] [Google Scholar]
- 300.Hung SY, Fu WM. Drug candidates in clinical trials for Alzheimer's disease. J Biomed Sci. 2017;24(1):47. doi: 10.1186/s12929-017-0355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Liu X, She W, Sung HH, Williams ID, Qian P. Tau-aggregation inhibitors derived from Streptomyces tendae MCCC 1A01534 protect HT22 cells against okadaic acid-induced damage. Int J Biol Macromol. 2023;231:123170. doi: 10.1016/j.ijbiomac.2023.123170. [DOI] [PubMed] [Google Scholar]
- 302.Zheng J, Xu M, Walker V, Yuan J, Korologou-Linden R, Robinson J, et al. Evaluating the efficacy and mechanism of metformin targets on reducing Alzheimer's disease risk in the general population: a Mendelian randomisation study. Diabetologia. 2022;65(10):1664–1675. doi: 10.1007/s00125-022-05743-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Xu X, Sun Y, Cen X, Shan B, Zhao Q, Xie T, et al. Metformin activates chaperone-mediated autophagy and improves disease pathologies in an Alzheimer disease mouse model. Protein Cell. 2021;12(10):769–787. doi: 10.1007/s13238-021-00858-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Chen S, Gan D, Lin S, Zhong Y, Chen M, Zou X, et al. Metformin in aging and aging-related diseases: clinical applications and relevant mechanisms. Theranostics. 2022;12(6):2722–2740. doi: 10.7150/thno.71360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Akter R, Afrose A, Rahman MR, Chowdhury R, Nirzhor SSR, Khan RI, et al. A comprehensive analysis into the therapeutic application of natural products as SIRT6 modulators in Alzheimer's disease, aging, cancer, inflammation, and diabetes. Int J Mol Sci. 2021;22(8):4180. doi: 10.3390/ijms22084180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Childs BG, Gluscevic M, Baker DJ, Laberge RM, Marquess D, Dananberg J, et al. Senescent cells: an emerging target for diseases of ageing. Nat Rev Drug Discov. 2017;16(10):718–735. doi: 10.1038/nrd.2017.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Wang TW, Johmura Y, Suzuki N, Omori S, Migita T, Yamaguchi K, et al. Blocking PD-L1-PD-1 improves senescence surveillance and ageing phenotypes. Nature. 2022;611(7935):358–364. doi: 10.1038/s41586-022-05388-4. [DOI] [PubMed] [Google Scholar]
- 308.Kirkland JL, Tchkonia T. Senolytic drugs: from discovery to translation. J Intern Med. 2020;288(5):518–536. doi: 10.1111/joim.13141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Xu M, Pirtskhalava T, Farr JN, Weigand BM, Palmer AK, Weivoda MM, et al. Senolytics improve physical function and increase lifespan in old age. Nat Med. 2018;24(8):1246–1256. doi: 10.1038/s41591-018-0092-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Justice JN, Nambiar AM, Tchkonia T, LeBrasseur NK, Pascual R, Hashmi SK, et al. Senolytics in idiopathic pulmonary fibrosis: results from a first-in-human, open-label, pilot study. EBioMedicine. 2019;40:554–563. doi: 10.1016/j.ebiom.2018.12.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Chen P, Guo Z, Zhou B. Insight into the role of adult hippocampal neurogenesis in aging and Alzheimer's disease. Ageing Res Rev. 2023;84:101828. doi: 10.1016/j.arr.2022.101828. [DOI] [PubMed] [Google Scholar]
- 312.Gonzales MM, Garbarino VR, Kautz TF, Palavicini JP, Lopez-Cruzan M, Dehkordi SK, et al. Senolytic therapy in mild Alzheimer's disease: a phase 1 feasibility trial. Nat Med. 2023;29(10):2481–2488. doi: 10.1038/s41591-023-02543-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.