Abstract
Background and Aim
This study aimed to identify the indications for liver transplantation (LT) based on underlying etiology and to characterize the patients who underwent LT.
Materials and Methods
We conducted a multicenter cross-sectional observational study across 11 tertiary centers in Turkiye from 2010 to 2020. The study included 5,080 adult patients.
Results
The mean age of patients was 50.3±15.2 years, with a predominance of female patients (70%). Chronic viral hepatitis (46%) was the leading etiological factor, with Hepatitis B virus infection at 35%, followed by cryptogenic cirrhosis (24%), Hepatitis C virus infection (8%), and alcohol-related liver disease (ALD) (6%). Post-2015, there was a significant increase in both the number of liver transplants and the proportion of living donor liver transplants (p<0.001). A comparative analysis of patient characteristics before and after 2015 showed a significant decline in viral hepatitis-related LT (p<0.001), whereas fatty liver disease-related LT significantly increased (p<0.001).
Conclusion
Chronic viral hepatitis continues to be the primary indication for LT in Turkiye. However, the proportions of non-alcoholic fatty liver disease (NAFLD) and ALD-related LT have seen an upward trend over the years.
Keywords: Etiology, HBV, NAFLD, liver transplantation
Introduction
Cirrhosis and its complications are the predominant indications for liver transplantation (LT) globally.[1] Cirrhosis, both with and without hepatocellular carcinoma (HCC), is a leading cause of death worldwide. Cirrhosis ranks as the 11th most common cause of mortality, while HCC stands as the 16th most common; combined, they contribute to 3.5% of all global deaths.[2] In Western countries, the most prevalent causes of cirrhosis are hepatitis C virus (HCV) infection, alcohol consumption, and non-alcoholic fatty liver disease (NAFLD), whereas hepatitis B virus (HBV) infection is the principal cause in developing countries.[3] In Turkiye, HBV infection continues to be a significant contributor to liver-related morbidity and mortality.[4,5] HBV-related cirrhosis, with or without HCC, accounts for about 40–50% of LT cases.[6]
NAFLD has become an increasingly critical public health issue worldwide. From 1988 to 2008, while the prevalence of chronic liver disease (CLD) and cirrhosis remained stable, the incidence of NAFLD and NAFLD-related cirrhosis steadily rose.[7–11] By 2014, NAFLD-related cirrhosis had emerged as the second most common reason for LT in the United States, representing 17.4% of all LTs.[10] In Turkiye, NAFLD prevalence exceeds 30%,[12] with higher rates observed in patients with obesity, type 2 diabetes mellitus (T2DM), hyperlipidemia, and metabolic syndrome (MeS).[13,14] This study aims to identify the indications for LT by underlying etiology and to examine the characteristics of patients who underwent LT in the past decade.
Materials and Methods
We conducted a multicenter, cross-sectional retrospective observational study at 11 tertiary centers in Turkiye from 2010 to 2020. The study included 5,080 adult patients who underwent LT. To analyze the changing etiology patterns over time, we divided the timeframe into two periods: January 1, 2010, to December 31, 2014 (first period), and January 1, 2015, to December 31, 2020 (second period). Cirrhosis was defined using clinical, biochemical, and histological findings when available. International Classification of Diseases, Tenth Revision (ICD-10) codes, were employed to identify cirrhosis and its complications. Indications were categorized into several groups: viral hepatitis, alcohol-related liver disease (ALD), NAFLD, autoimmune liver diseases (autoimmune hepatitis [AIH], primary biliary cholangitis [PBC], primary sclerosing cholangitis [PSC]), and miscellaneous factors, based on ICD-10 diagnostic codes. Etiological diagnoses adhered to international criteria. Patients with acute liver failure, those who underwent retransplantation or multi-organ transplantation were excluded. A specialized electronic case report form (CRF) was designed for data collection and recording, with each center entering relevant data into the CRF. This study received approval from the local ethical committee of Dokuz Eylul University School of Medicine (Date: May 05, 2022, No: 2022/19-14).
Definitions
The primary endpoints of this study were to identify the indications for LT by underlying cause before and after January 2015. The secondary endpoints focused on defining the clinical characteristics of patients who underwent LT. Patients were monitored at regular intervals in an outpatient clinic during the follow-up period.
Statistical Analysis
The Shapiro–Wilk test verified the normality assumption. Continuous variables were summarized as mean ± standard deviation (SD), while categorical variables were presented as frequencies (n) and percentages (%). The Pearson chi-square and Fisher’s Exact test were utilized to examine relationships between categorical variables. The independent t-test was applied for parametric comparisons between two independent groups. Post-hoc analysis included Bonferroni correction. All statistical analyses were performed using IBM SPSS Statistics for Windows, Version 23.0 (IBM Corp., Armonk, NY). A two-sided p<0.05 was considered statistically significant.
Results
Our study enrolled a total of 5,080 liver transplant recipients. The majority of these patients were female (69.6%), with a mean age of 50.3±15.2 years (range: 18–86 years). Chronic viral hepatitis was the most prevalent indication for LT in the cohort, accounting for 46.4% of cases. The leading etiology was HBV infection (35.2%), followed by cryptogenic cirrhosis (CC) (23.5%), HCV infection (8.2%), and alcohol-related liver disease (ALD) (6.2%). Among the participants, 939 patients (18.5%) had been diagnosed with hepatocellular carcinoma (HCC) prior to LT. A significant majority (79.7%) underwent living donor liver transplantation (LDLT), while the rest (20.3%) received cadaveric donor LT (Fig. 1). The baseline characteristics of the patients are presented in Table 1.
Figure 1.
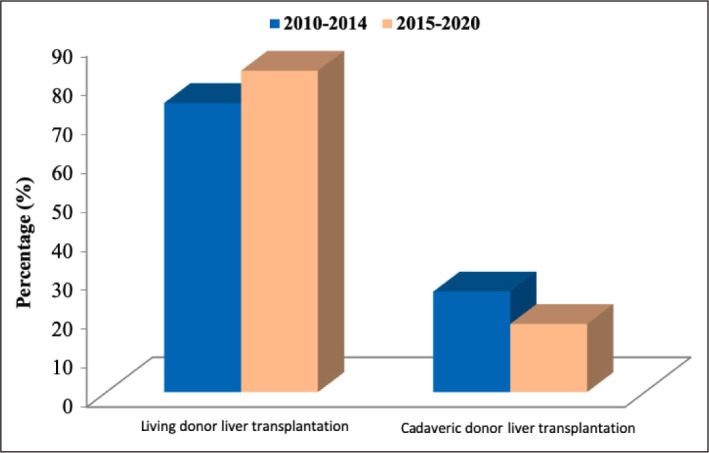
Live and cadaveric liver transplant before January 2015 and after January 2015.
Table 1.
Characteristics of patients who underwent liver transplantation
| Parameters | Periods | p | |||
|---|---|---|---|---|---|
| Between 2010–2014 (n=1677) | Between 2015–2020 (n=3403) | ||||
| n | % | n | % | ||
| Age (years), mean±SD | 50.0±1.9 | 50.7±5.8 | 0.707 | ||
| Gender | 0.930 | ||||
| Male | 509 | 30.4 | 1037 | 30.5 | |
| Female | 1168 | 69.6 | 2366 | 69.5 | |
| Liver transplantation | <0.001 | ||||
| Live LT | 1244 | 74.2 | 2807 | 82.5 | |
| Cadaveric LT | 433 | 25.8 | 596 | 17.5 | |
| HCC | 277 | 16.5 | 662 | 19.5 | 0.011 |
| Etiology | |||||
| Viral hepatitis-related | 1012 | 60.3 | 1458 | 42.8 | <0.001 |
| HBV | 668 | 40 | 1125 | 33.1 | <0.001 |
| HCV | 196 | 11.7 | 223 | 6.6 | <0.001 |
| HDV | 148 | 8.8 | 110 | 3.2 | <0.001 |
| Autoimmune liver diseases | |||||
| AIH | 56 | 3.3 | 167 | 4.9 | 0.010 |
| PBC | 24 | 1.4 | 64 | 1.9 | 0.248 |
| PSC | 18 | 1.1 | 97 | 2.9 | <0.001 |
| NAFLD | 5 | 0.3 | 82 | 2.4 | <0.001 |
| ALD | 69 | 4.1 | 250 | 7.3 | <0.001 |
| CC | 347 | 20.7 | 849 | 24.9 | 0.001 |
| WD | 57 | 3.4 | 65 | 1.9 | 0.001 |
| BCS | 28 | 1.7 | 103 | 3 | 0.004 |
| HC | 3 | 0.2 | 9 | 0.3 | 0.761 |
| AAD | 3 | 0.2 | 10 | 0.3 | 0.564 |
| Others | 55 | 3.3 | 245 | 7.2 | <0.001 |
Statistical analysis (Student’s t-test, Pearson chi-square test, Fisher’s Exact test). SD: Standard deviation; HCC: Hepatocellular carcinoma; HBV: Hepatitis B virus; HCV: Hepatitis C virus; HDV: Hepatitis D virus; AIH: Autoimmune hepatitis; PBC: Primary biliary cholangitis; PSC: Primary sclerosing cholangitis; NAFLD: Non-alcoholic fatty liver disease; ALD: Alcoholic liver disease; CC: Cryptogenic cirrhosis; WD: Wilson’s disease; BCS: Budd-Chiari syndrome; HC: Haemochromatosis; AAD: Alpha1-antitripsin deficiency; LT: Liver transplantation.
Post-2015, there was a notable increase in the number of liver transplants (from 1,244 to 2,807 transplants) and the proportion of LDLTs (from 74.2% to 82.5%) (p<0.001). Comparing patient characteristics before and after January 2015, there was a significant reduction in viral hepatitis-related LTs (from 60.3% to 42.8%) (p<0.001), while the proportion of fatty liver disease-related LTs, including NAFLD and ALD, significantly increased (from 4.4% to 9.8%) (p<0.001) (Table 1). HBV infection remained the primary reason for LT, though its proportion decreased from 39.8% to 33.1% (p<0.001). Notably, NAFLD-related cirrhosis became the most rapidly increasing indication for LT (Fig. 2). After 2015, the incidence of HCC-related LTs significantly increased from 16.5% to 19.5% (p=0.011). Interestingly, the proportion of LTs related to cryptogenic cirrhosis rose from 20.7% to 24.9% over the years (p=0.001).
Figure 2.
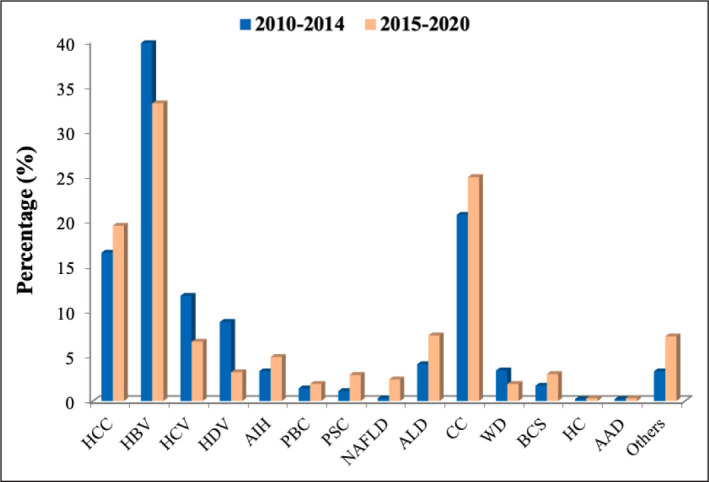
Indications for liver transplantation before January 2015 and after January 2015.
Discussion
This multicenter study, involving the leading LT centers in Turkiye, identifies evolving trends in LT indications over the years. Chronic viral hepatitis (46%) emerged as the most frequent indication in our cohort, with HBV infection (35%) as the predominant etiology of cirrhosis. Notably, the proportion of HBV-related LTs decreased from 40% to 33%, aligning with previous studies that identified chronic viral hepatitis as a primary cause of cirrhosis and HCC in Turkiye.[4,5,15]
There has been a dramatic shift in the main indications for LT over time. Prior to 1980, malignancies represented 50% of all LT indications, but this figure declined to 10% by the 1990s. Currently, cirrhosis is the leading indication.[11] The etiological trend of cirrhosis is evolving, influenced by effective treatments for viral hepatitis and rising prevalence of obesity and metabolic disorders. In Western populations, fatty liver diseases, including ALD and NAFLD, have become leading LT indications, surpassing HCV infection and HCC.[11,16] NAFLD, in particular, has emerged as the fastest-growing etiology of cirrhosis. Prior to 2000, the proportion of NAFLD-related cirrhosis was negligible. However, in the United States, the proportion of NAFLD-related LT increased by 162% between 2003 and 2014.[10] In Turkiye, Degertekin et al.[17] reported a high NAFLD prevalence of 48%. Our study found that, during the second period, there was a decrease in HBV-related LTs and an increase in NAFLD-related and ALD-related LTs (p<0.001), likely due to rising obesity, diabetes, and NAFLD prevalence in Turkiye.[18–20] These findings corroborate previous studies that show a decline in viral hepatitis-related LTs and an increase in NAFLD- and ALD-related LTs.[11,16,21]
This is the first multicenter study to detail recent etiological trends in LT indications in Turkiye. Its main strength lies in the retrospective analysis. Despite meticulous examination of patient characteristics in the CRF, potential misclassifications of cirrhosis etiology, especially in CC- and NAFLD-related cases, particularly before January 2015, cannot be ruled out.
Conclusion
While HBV infection remains the principal etiology for LT in Turkiye, NAFLD-related cirrhosis and LT represent a growing burden.
Acknowledgement
The authors extend their gratitude to Basak Oguz Yolcular for the invaluable support provided during the statistical analysis phase of this study.
Footnotes
How to cite this article: Akarsu M, Dolu S, Harputluoglu M, Yilmaz S, Akyildiz M, Gencdal G, et al. Changing trends in the etiology of liver transplantation in Turkiye: A multicenter study. Hepatology Forum 2024; 5(1):3–6.
Ethics Committee Approval
The Dokuz Eylul University Clinical Research Ethics Committee granted approval for this study (date: 25.05.2022, number: 2022/19-14).
Peer-review
Externally peer-reviewed.
Author Contributions
Concept – MA, SD, RI; Design – SY, MA,GG, KYP, DD, HA, IT, FG, ZK; Supervision – HG, SK, GK, MAK, MK, MTG, YB; Fundings – MA, SD, MH, SY, MA, GG, KYP, DD, HA, IT, FG, ZK, HG, SK, GK, MAK, MK, MTG, YB, ABD, AS, ZME, FE, RI; Materials – MA, SD, MH, SY, MA, GG, KYP, DD, HA, IT, FG, ZK, HG, SK, GK, MAK, MK, MTG, YB, ABD, AS, ZME, FE, RI; Data Collection and/or Processing – MA, SD, MH, SY, MA, GG, KYP, DD, HA, IT, FG, ZK, HG, SK, GK, MAK, MK, MTG, YB, ABD, AS, ZME, FE, RI; Analysis and/or Interpretation – ABD, AS, ZME, FE; Literature Search – MA, SD, RI, HG, SK, GK, MAK, MK, MTG, YB, ABD, AS, ZME, FE; Writing – MA, SD, RI, SY, MA,GG, KYP, DD, HA, IT, FG, ZK, GK, MAK, MK, MTG, YB; Critical Reviews – MA, SD, RI, IT, YB.
Conflict of Interest
The authors have no conflict of interest to declare.
Financial Disclosure
The authors declared that this study has received no financial support.
References
- 1.Krasinskas AM, Eghtesad B, Kamath PS, Demetris AJ, Abraham SC. Liver transplantation for severe intrahepatic noncirrhotic portal hypertension. Liver Transpl. 2005;11(6):627–634. doi: 10.1002/lt.20431. discussion 610-611. [DOI] [PubMed] [Google Scholar]
- 2.Asrani SK, Devarbhavi H, Eaton J, Kamath PS. Burden of liver diseases in the world. J Hepatol. 2019;70(1):151–171. doi: 10.1016/j.jhep.2018.09.014. [DOI] [PubMed] [Google Scholar]
- 3.Setiawan VW, Stram DO, Porcel J, Lu SC, Le Marchand L, Noureddin M. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology. 2016;64(6):1969–1977. doi: 10.1002/hep.28677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bayan K, Yilmaz S, Tuzun Y, Yildirim Y. Epidemiological and clinical aspects of liver cirrhosis in adult patients living in Southeastern Anatolia: leading role of HBV in 505 cases. Hepatogastroenterology. 2007;54(80):2198–2202. [PubMed] [Google Scholar]
- 5.Ökten A, Acar A, Çakaloğlu Y, Kaymakoğlu S, Boztaş G. Karaciğer sirozunun etyolojisi (1052 vakanın analizi) T Klin Gastroenterohepatoloji. 1995;6:45–49. [Turkish] [Google Scholar]
- 6.Akarsu M, Onem S, Turan I, Adali G, Akdogan M, Akyildiz M, et al. Recommendations for Hepatitis B Immunoglobulin and Antiviral Prophylaxis Against Hepatitis B Recurrence After Liver Transplantation. Turk J Gastroenterol. 2021;32(9):712–719. doi: 10.5152/tjg.2021.21608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wong RJ, Singal AK. Trends in liver disease etiology among adults awaiting liver transplantation in the United States, 2014–2019. JAMA Netw Open. 2020;3(2):e1920294. doi: 10.1001/jamanetworkopen.2019.20294. [DOI] [PubMed] [Google Scholar]
- 8.Wen PH, Lu CL, Strong C, Lin YJ, Chen YL, Li CY, Tsai CC. Demographic and Urbanization Disparities of Liver Transplantation in Taiwan. Int J Environ Res Public Health. 2018 Jan 23;15(2):177. doi: 10.3390/ijerph15020177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mathur AK, Schaubel DE, Gong Q, Guidinger MK, Merion RM. Sex-based disparities in liver transplant rates in the United States. Am J Transplant. 2011;11(7):1435–1443. doi: 10.1111/j.1600-6143.2011.03498.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cholankeril G, Wong RJ, Hu M, Perumpail RB, Yoo ER, Puri P, et al. Liver transplantation for nonalcoholic steatohepatitis in the us: temporal trends and outcomes. Dig Dis Sci. 2017;62(10):2915–2922. doi: 10.1007/s10620-017-4684-x. [DOI] [PubMed] [Google Scholar]
- 11.Adam R, Karam V, Delvart V, O’Grady J, Mirza D, Klempnauer J, et al. All contributing centers ( www.eltr.org); European Liver and Intestine Transplant Association (ELITA) Evolution of indications and results of liver transplantation in Europe. A report from the European Liver Transplant Registry (ELTR) J Hepatol. 2012;57(3):675–688. doi: 10.1016/j.jhep.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 12.Kaya E, Yılmaz Y. Non-alcoholic fatty liver disease: A growing public health problem in Turkey. Turk J Gastroenterol. 2019;30(10):865–871. doi: 10.5152/tjg.2019.18045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bellentani S, Scaglioni F, Marino M, Bedogni G. Epidemiology of nonalcoholic fatty liver disease. Dig Dis. 2010;28(1):155–161. doi: 10.1159/000282080. [DOI] [PubMed] [Google Scholar]
- 14.Rodríguez-Perálvarez M, Gómez-Bravo MÁ, Sánchez-Antolín G, De la Rosa G, Bilbao I, Colmenero J, on behalf of the Spanish Society of Liver Transplantation (SETH) Consensus Panel Expanding Indications of Liver Transplantation in Spain: Consensus Statement and Recommendations by the Spanish Society of Liver Transplantation. Transplantation. 2021;105(3):602–607. doi: 10.1097/TP.0000000000003281. [DOI] [PubMed] [Google Scholar]
- 15.Idilman R, Aydogan M, Oruncu MB, Kartal A, Elhan AH, Ellik Z, et al. Natural history of cirrhosis: Changing trends in etiology over the years. Dig Dis. 2021;39(4):358–365. doi: 10.1159/000512746. [DOI] [PubMed] [Google Scholar]
- 16.Alqahtani SA, Larson AM. Adult liver transplantation in the USA. Curr Opin Gastroenterol. 2011;27(3):240–247. doi: 10.1097/MOG.0b013e3283457d5d. [DOI] [PubMed] [Google Scholar]
- 17.Değertekin B, Tozun N, Demir F, Söylemez G, Parkan Ş, Gürtay E, et al. The changing prevalence of non-alcoholic fatty liver disease (NAFLD) in Turkey in the last decade. Turk J Gastroenterol. 2021;32(3):302–312. doi: 10.5152/tjg.2021.20062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Satman I, Yilmaz T, Sengül A, Salman S, Salman F, Uygur S, et al. Population-based study of diabetes and risk characteristics in Turkey: results of the turkish diabetes epidemiology study (TURDEP) Diabetes Care. 2002;25(9):1551–1556. doi: 10.2337/diacare.25.9.1551. [DOI] [PubMed] [Google Scholar]
- 19.Satman I, Omer B, Tutuncu Y, Kalaca S, Gedik S, Dinccag N, et al. TURDEP-II Study Group Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28(2):169–180. doi: 10.1007/s10654-013-9771-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yilmaz Y, Yilmaz N, Ates F, Karakaya F, Gokcan H, Kaya E, et al. Fatty Liver Diseases Special Interest Groups The prevalence of metabolic-associated fatty liver disease in the Turkish population: A multicenter study. Hepatol Forum. 2021;2(2):37–42. doi: 10.14744/hf.2021.2020.0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Younossi Z, Tacke F, Arrese M, Chander Sharma B, Mostafa I, Bugianesi E, et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 2019;69(6):2672–2682. doi: 10.1002/hep.30251. [DOI] [PubMed] [Google Scholar]


