Figure 3. Critical periods of sex hormonal transition during the lifespan.
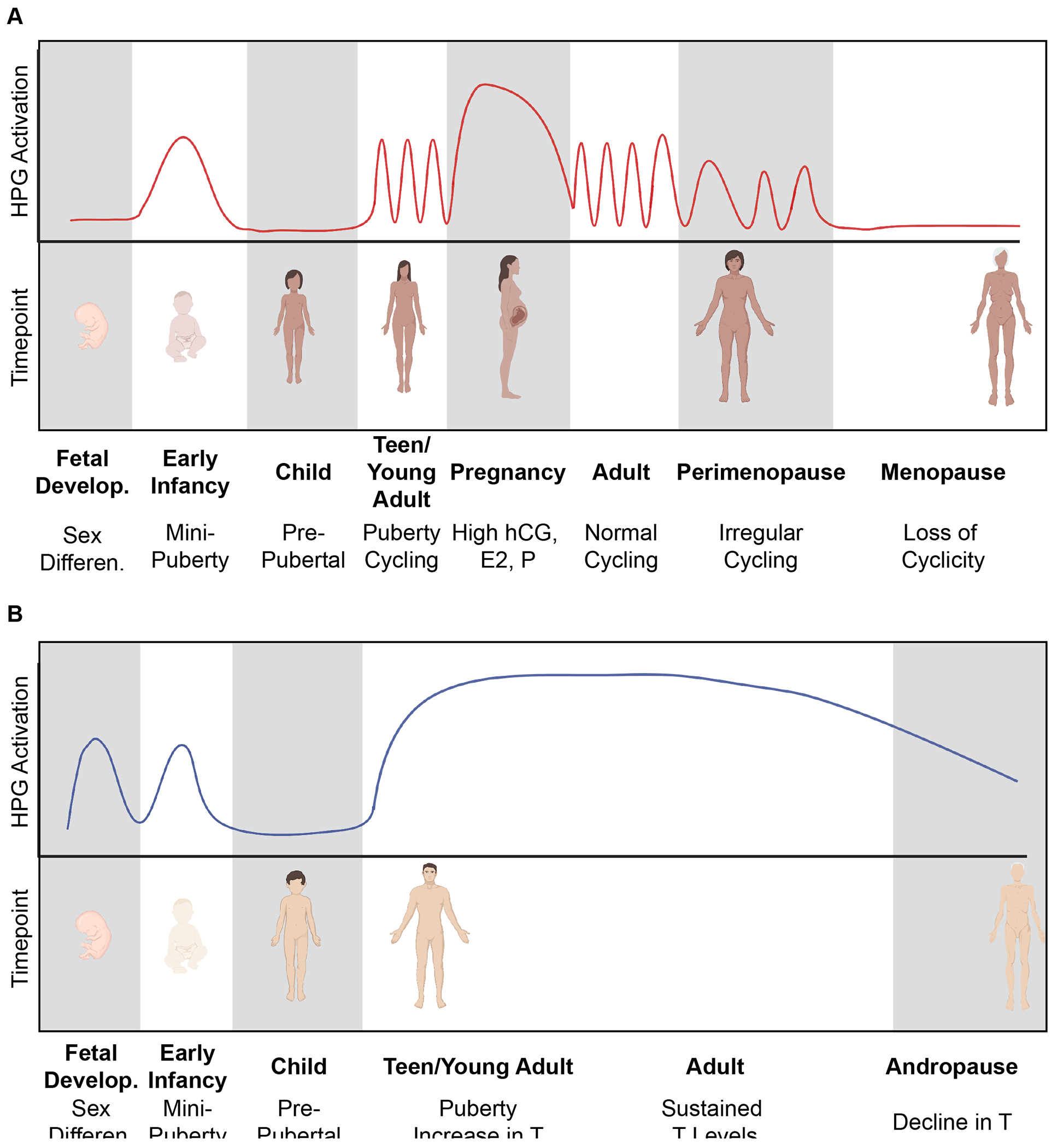
A) Females undergo many important hormonal transitions throughout the lifespan. During fetal development, the absence of male sex hormones causes sex differentiation of female secondary sex characteristics. During early infancy, a “minipuberty” period solidifies the HPG axis and further develops the ovaries and female genitalia. The pre-pubertal window of childhood has low HPG axis activity until the onset of puberty. Female puberty begins the menstrual cycle and hormone levels within the HPG axis are constantly changing. Pregnancy causes cycling to pause and hormones (hCG, E2, P, protein hormones) stay elevated to maintain the healthy pregnancy. Parturition is associated with a sharp decline in pregnancy hormones and a return to normal cyclicity. During peri-menopause, cyclicity becomes irregular as the ovarian follicular reserve is depleted. In the absence of follicles, ovarian hormones (E2, P) are not produced and cycling ceases completely to enter the menopausal period (~50 years old). B) In males, sex differentiation is determined by the production of T and AMH during fetal development. Males also undergo a “minipuberty” during early infancy with activation of the HPG axis which causes the continued development of the testes and external male genitalia. During pre-pubertal childhood, there is relative quiescence of the HPG axis until the onset of puberty. HPG axis activation during puberty results in the increase in T under the control of LH. In addition, FSH triggers the production of sperm by Sertoli cells. T levels remain relatively steady across the lifespan (with small decreases with aging), until ~70 years old when T declines during andropause. Created with Biorender.com.
