ABSTRACT
Identification of the diverse animal hosts responsible for spill-over events from animals to humans is crucial for comprehending the transmission patterns of emerging infectious diseases, which pose significant public health risks. To better characterize potential animal hosts of Lassa virus (LASV), we assessed domestic and non-domestic animals from 2021–2022 in four locations in southern Nigeria with reported cases of Lassa fever (LF). Birds, lizards, and domestic mammals (dogs, pigs, cattle and goats) were screened using RT-qPCR, and whole genome sequencing was performed for lineage identification on selected LASV positive samples. Animals were also screened for exposure to LASV by enzyme-linked immunosorbent assay (ELISA). Among these animals, lizards had the highest positivity rate by PCR. Genomic sequencing of samples in most infected animals showed sub-lineage 2 g of LASV. Seropositivity was highest among cattle and lowest in pigs. Though the specific impact these additional hosts may have in the broader virus-host context are still unknown – specifically relating to pathogen diversity, evolution, and transmission – the detection of LASV in non-rodent hosts living in proximity to confirmed human LF cases suggests their involvement during transmission as potential reservoirs. Additional epidemiological data comparing viral genomes from humans and animals, as well as those circulating within the environment will be critical in understanding LASV transmission dynamics and will ultimately guide the development of countermeasures for this zoonotic health threat.
KEYWORDS: Lassa virus, LASV genomes, non-rodents, animals, Nigeria, LASV lineages 2 g
Introduction
Lassa virus (LASV), a zoonotic virus of the family Arenaviridae and genus Mammarenavirus, is the causative agent of Lassa fever (LF). LF is endemic in most parts of Western Africa with thousands of LASV infections occurring in humans annually. Of these, several hundredths die as a result of the infection [1,2]. In Nigeria, 1968 LF cases were confirmed between January 2022 and September 2023 [3]. Natal mastomys (Mastomys natalensis) was first demonstrated to be the natural reservoir host for LASV; however, LASV has been shown to be maintained in multiple rodent reservoirs [1,4–7]. LF outbreaks normally correlate with the movement of these rodent reservoirs from forests and farms to human dwellings. This is commonly observed to peak during the dry season (between December and April) when there is an increase in forest burning and a decrease in farming [8,9].
The true incidence of LF remains unknown, and it is believed to be driven in part by the prevalence of rodent reservoirs in human dwellings. Evidence of rodent transmission and human-to-human transmission (especially nosocomial infections) have been previously documented [1,5,6,10,11]. During a LF outbreak with an unusual surge in the number of cases in Nigeria in 2018, Siddle et al. [12] studied the viral strains responsible for the infections. The data generated from their research implicated cross-species transmission from local rodent populations rather than sustained extensive human-to-human transmission. They also found that the increase in cases was not attributable to a particular LASV strain. Their findings suggested that numerous distinct cross-species transmission events from a genetically diverse reservoir continue to sustain LASV infections.
Serological and viral evidence of LASV infection have been found in other rodents such as roof rats (Rattus rattus) and house mice (Mus musculus) [6,7,11]. Specifically, Olayemi et al. [6] found that the African wood mouse (Hylomyscus pamfi) and the reddish-white mastomys (Mastomys erythroleucus) were positive for LASV by PCR over several years at the same sites and are likely to be legitimate reservoirs and not simply incidental hosts. Additionally, LASV isolated from H. pamfi did not cluster systematically with any of the four well-established lineages [13]. In a study of natal mastomys from Mali, Manning et al. [14] described an emerging fifth lineage of LASV. These data illustrate that the evolution of LASV and the dynamics of the virus are more complex genetically and ecologically than previously appreciated and are likely maintained by multiple reservoirs. This has implications for the epidemiology and control of LF, and for understanding the circulating LASV variants as zoonotic threats when developing vaccines and drugs.
Besides rodent reservoirs, non-human primates (NHPs) are susceptible to infection. NHPs of several species have been used as animal models for LASV infection in assessing potential therapeutics [15–17]. Ogunro et al. [18] found serologic evidence of natural LASV infection in four Mona monkeys (Cercopithecus mona) and one Anubis Baboon (Papio Anubis), and antigenic evidence from one Mona monkey in southern Nigeria, raising the question of whether NHPs play a role in the epidemiology of LF.
The commensal nature, strategic habitats, and activities of natal mastomys facilitates their interactions with other rodent and non-rodent species [19,20]. Because it is not only humans that come in contact with rodents, it is important to broaden LF surveillance to include domesticated and non-domesticated terrestrial non-rodent animals. This study of domestic and wild animals in close contact with humans in LF endemic areas was designed to identify non-rodent species’ potential as hosts or reservoirs of LASV. Additionally, we assessed the presence of LASV variants with spill-over potential circulating in animal hosts. Here, we report the first detection and characterization of LASV in non-rodents by quantitative RT–PCR (RT-qPCR) and Next Generation Sequencing (NGS). We also show exposure and seroconversion to LASV in multiple domestic terrestrial non-rodent animals in southern Nigeria.
Materials and methods
Ethical approval
Ethical approval for this study was obtained from the Nigeria Health Research Ethics Committee (NHREC01/01/2007), the National Veterinary Research Institute (NVRI), Jos, Nigeria (AEC/03/120/22) and the Animal Care and Use Review Office (ACURO) of the United States Army Medical Research and Development Command (USAMRDC).
Study sites
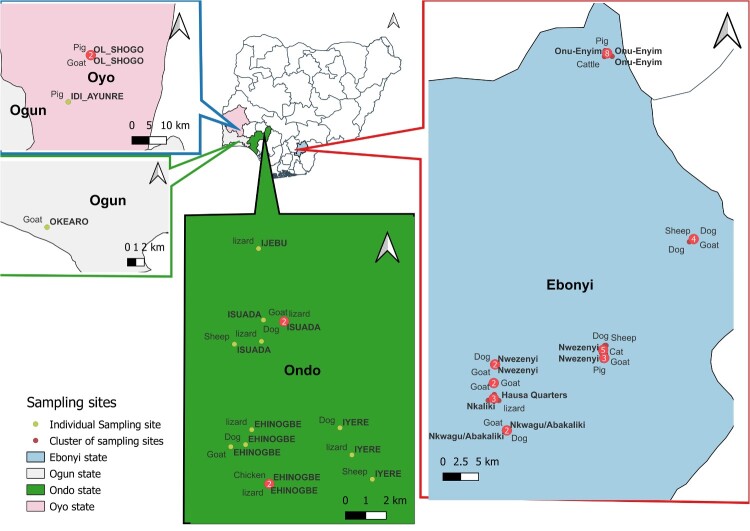
From May 2021 to October 2022, spanning across two different LF seasons, non-rodents were sampled in two disease endemic regions in southeastern (Ebonyi State) and southwestern (Ondo State) Nigeria, and two LF non-endemic regions in southwestern (Ogun and Oyo States) Nigeria. Samples were collected from four communities (Ijebu-Owo, Isuada, Ehin-Ogbe and Iyere) in Owo Local Government Area (LGA), Ondo State; six communities (Hausa Quarters, Nkaliki, Nkwagu Nwezenyi, Odunukwe and Onu-Eyim) within six LGAs in Ebonyi State; two communities (Ijebu-Ode and Oke-Aro) from two LGAs in Ogun State; and five communities (Agbowo, Amosun-Akinyele, Idi-Ayunre, Ilu-Tuntun and Olorunsogo) from four LGAs in Oyo State in Nigeria (Figure 1).
Figure 1.
Geospatial summary of study sites.
Sample collection
Animals included in this study were observed to live in proximity with humans. Prior to sample collection from domestic animals such as dogs, cats, sheep, goats, cattle, pigs, and poultry found within consented households, physical examination was performed on each animal and clinical parameters were recorded. These included physical presentation, presence of ocular/nasal discharge, faecal appearance, respiratory sounds and rate, heart sounds and rate, body temperature, mucous membrane colour, body score and presence of ectoparasites. The hydration status of each animal examined was assessed based on the degree of dryness of hair coat and mucous membranes (conjunctiva and oral wall) and the sunkenness of eyes.
When possible, blood, oral and rectal swabs were collected from each animal. Animals were restrained by an animal handler using best practices and without inflicting pain to the animals. Five millilitres (5 ml) of blood was collected into sterile EDTA tubes from the jugular vein (in sheep, goat and, cattle), cephalic vein (dogs and cats), wing vein (poultry) and anterior vena cava (pigs) and processed for plasma. Oral and rectal swabs were collected and stored in viral transport medium or DNA/RNA ShieldTM (ZYMO RESEARCH).
Lizards (specifically Agama agama) were also trapped for sample collection in the evenings from crevices and other hideouts in and around the houses. Oral and cloacal swabs were collected from the lizards and transferred into a viral transport medium or DNA/RNA shieldTM (ZYMO RESEARCH). After samples were collected from the lizards, they were marked and released.
All samples collected were aliquoted in duplicate and transported to the laboratory via cold chain. One aliquot of each sample was stored at −20°C until analysed, while the second aliquot was kept at −80°C for long-term storage.
RNA extraction and reverse transcription polymerase chain reaction (RT-qPCR)
Total RNA was extracted from 140 µl of plasma, oral, and/or rectal /cloacal swabs of non-rodent animals using QIAamp Viral RNA extraction kit (Qiagen, Hilden, Germany) according to the manufacturer’s instructions. Three microliters (3 µl) of the isolated RNA from each sample was then used for the detection of LASV nucleic acid using Superscript III Platinum SYBR Green one-step RT-qPCR kit (Life Technologies, CA, USA). Specific primers targeting the nucleoprotein (NP) gene on the S segment of the viral genome (LASV-NG-F – 5′ – YAC AGG GTC YTC TGG WCG ACC – 3′ and LASV-NG-R – 3′ – RAT GAT GCA RCT TGA CCC AAG – 3′), as previously described [7,21] were used. Each sample type was run in duplicate, and the average cycle threshold (Ct) value was recorded. Negative extracts (NE) and No Template controls (NTC) were used as negative controls while the positive controls were the g-Block synthesized for the project and the previously confirmed LASV positive samples described by Happi et al, 2022 [7]. An animal was considered positive if at least one of the samples tested from that animal had Ct value <40 with all the negative controls confirmed negative and positive controls confirmed positive for each run.
LASV enzyme-linked Immunosorbent assay (ELISA)
An indirect ELISA was performed on plasma samples using ReLASV® Pan-Lassa IgG/IgM ELISA Test Kits (Zalgen Labs, LLC) with the LASV Nucleoprotein (NP) as the capture antigen to detect antibodies (IgG). A 1:100 dilution of LASV-naïve samples (dog, goat, sheep, cattle, and pig sera from USA), test samples, and negative control were prepared and 100 µl of these diluted preparations were dispensed in duplicate onto the ELISA plate microwells. The plate was incubated for 30 min at ambient temperature (18–30°C) and washed 4 times with 300 µl of wash solution (Tween20 /PBS wash buffer). Anti-animal (corresponding to each animal species) IgG horseradish peroxidase-conjugated secondary antibody solution reagent (100 µl) was then added to each well. This was followed by a second incubation and wash. 100 µl/well of the One-Component substrate was then added to the plate and incubated for 10 min at ambient temperature in the dark. Finally, 100 µl/well of the Stop solution was added to terminate the enzyme reaction. The optical density (O.D.) value of each well of the prepared plate was read at 450 and 630 nm using the Biotek 800 TS ELISA plate reader and recorded to determine the concentration of IgG. After this, the delta O.D. values were calculated by subtracting the (630 nm – mean blank) values from the (450 nm – mean blank) values. Negative cut-off was determined to be mean O.D. values of the naïve plasma samples from LASV free regions (USA) per animal species plus 3 standard deviations (3SD). Samples higher than the cut-off were recorded as positive.
Data analyses
Data were documented serially using the unique animal identification number and were analysed using version 8 Epi Info software (Centers for Disease Control and Prevention, Atlanta, GA) and SPSS for windows (version 25.0, SPSS Inc., Chicago, IL). Simple graphs for results illustration were prepared using GraphPad Prism version 8.0 (GraphPad Software, San Diego, California USA) and Microsoft Excel, while the map showing the spatial distribution was done using the QGIS version 3.22.9 (GPS software). Discrete variables (proportions of LASV positive animals and samples, and frequency of LASV seropositivity) were compared using a test of proportion by calculating chi-square with Yate’s continuity correction. Normally distributed, continuous variables (clinical parameters) were compared by Student’s t-tests and/or analysis of variance (ANOVA), as applicable. Variables not conforming to a normal distribution (geometric mean ct values) were compared by Mann–Whitney U-test or Kruskal–Wallis, as applicable. All tests of significance were two-tailed and values of p < 0.05 were indicative of statistical significance.
Library preparation and genome sequencing of PCR LASV positive non-rodents
We constructed sequencing libraries from 48 LASV PCR positive samples with Ct ≤ 33. For this, cDNA was generated from RNA extracts using the Nextera XT library preparation kit [22], followed by paired-end sequencing using the Illumina NextSeq 2000 p2-300 cycle cartridge on a NextSeq 2000 instrument (Illumina, San Diego, CA, USA).
Genome assembly
We performed de novo assembly and reference-based refinement with the viral-ngs pipeline [23] to produce six partial and complete genomes from animals sampled from July 2021 to March 2022. These included three goats (sampled from Abakaliki), one dog and two lizards (sampled from Owo).
Phylogenetic analysis
To determine the evolutionary relationships of the study’s sequences to known Lassa diversity, we downloaded all publicly available LASV sequences from the NCBI virus database. We filtered the sequence dataset to remove (1) laboratory strains (passaged, recombinant), (2) duplicates, (3) sequences without collection times, and (4) sequences < 500nt. Sequences were trimmed to their coding regions for the L (N = 754) and S (N = 1185) segments respectively in sense orientation. We aligned the L and S segments independently using MAFFT v7.505 and curated the alignment manually [24]. We reconstructed phylogenetic trees including our partial and complete sequences using IQTREE2 v2.2 [25] under ModelFinderPlus [26] and assessed bifurcation support by UFBoot2 [27]. The best-fit models for the L and S segments were TIM2 + F + R10 and SYM + R10 respectively. For the Lineage 2 phylogenies, we additionally filtered out all sequences with more than 10% ambiguous nucleotides and sequences that were below 50% segment length.
Results
Summary of samples analysed for LASV using RT-qPCR and ELISA
A total of 1596 samples collected from 870 non-rodents were analysed. Of these non-rodents, 585 were analysed for LASV by RT-qPCR (Supplementary Table S1), 679 for LASV IgG detection by ELISA (Supplementary Table S2), while 392 were analysed by both RT-qPCR and ELISA methods.
LASV detection using RT-qPCR
From the 585 animals analysed by RT-qPCR, 144 (24.6%) tested positive for LASV, with those from Ebonyi State (91/243; 37.4%) having a significantly higher positivity compared to those from other states (p < 0.0001) (Table 1).
Table 1.
Non-rodent LASV RT-qPCR positivity rate.
| State | Study Community | Overall | Rectal swab | Oral swab | ||||||
| |
|
Total analysed |
No. positive |
% Positivity |
Total analysed |
No. positive |
% Positivity |
Total analysed |
No. positive |
% Positivity |
| Ebonyi | Hausa Quarters | 24 | 2 | 8.3 | 18 | 2 | 11.1 | 17 | 1 | 5.9 |
| Ndinwikwe Iboko | 6 | 5 | 88.3 | 6 | 2 | 33.3 | 6 | 4 | 66.7 | |
| Nkaliki | 55 | 7 | 12.7 | 38 | 7 | 18.4 | 37 | 2 | 5.4 | |
| Nkwagu | 17 | 8 | 47.1 | 17 | 6 | 35.3 | 17 | 8 | 47.1 | |
| Nwezenyi | 83 | 42 | 47.1 | 69 | 35 | 50.7 | 72 | 12 | 16.7 | |
| Odunukwe | 10 | 4 | 40 | 8 | 3 | 37.5 | 9 | 2 | 22.2 | |
| Onu-Enyim | 48 | 23 | 47.9 | 45 | 16 | 35.6 | 43 | 9 | 20.9 | |
| Total | 243 | 91 | 37.4 | 201 | 71 | 35.3 | 201 | 38 | 18.9 | |
| Ondo | Ehinogbe | 91 | 11 | 12.1 | 69 | 4 | 5.8 | 69 | 8 | 11.6 |
| Ijebu-Owo | 33 | 6 | 18.2 | 20 | 0 | 0 | 17 | 6 | 35.3 | |
| Isuada | 63 | 14 | 22.2 | 38 | 6 | 15.8 | 39 | 10 | 25.6 | |
| Iyere | 72 | 11 | 15.3 | 47 | 5 | 10.6 | 46 | 8 | 17.4 | |
| Total | 259 | 42 | 16.2 | 174 | 15 | 8.6 | 171 | 32 | 18.7 | |
| Ogun | Ijebu | 13 | 1 | 7.7 | 13 | 0 | 0 | 13 | 1 | 7.7 |
| Oke-Aro | 47 | 5 | 10.6 | 47 | 2 | 4.3 | 47 | 3 | 6.4 | |
| Total | 60 | 6 | 10 | 60 | 2 | 3.3 | 60 | 4 | 6.7 | |
| Oyo | Amosun-Akinyele | 3 | 0 | 0 | 3 | 0 | 0 | 3 | 0 | 0 |
| Idi-Ayunre | 3 | 1 | 33.3 | 3 | 1 | 33.3 | 3 | 1 | 33.3 | |
| Ilu Tuntun | 3 | 0 | 0 | 3 | 0 | 0 | 3 | 0 | 0 | |
| Olorunshogo | 5 | 4 | 80 | 5 | 2 | 40 | 5 | 3 | 60 | |
| Agbowo | 9 | 0 | 0 | 9 | 0 | 0 | 9 | 0 | 0 | |
| Total | 23 | 5 | 21.7 | 23 | 3 | 13 | 23 | 4 | 17.4 | |
| Grand Total | 585 | 144 | 24.6 | 458 | 91 | 19.9 | 455 | 78 | 17.1 | |
Note: No., Number, %, percentage.
LASV RT-qPCR of animals by communities in each study location
In Ebonyi State, four of the study communities had a LASV positivity rate ≥40% while Hausa Quarters (8.3%) and Nkaliki (12.7%) communities had <40% LASV positive animals. The positivity rate of LASV in non-rodents was significantly lower in Hausa Quarters compared to other communities (p = 0.002) (Table 1).
In Ondo State, LASV RT-qPCR positivity in all the four study communities was 16.6% (range 12.1% to 20.6%) with the least and highest rate being in Ehinogbe and Isuada, respectively. There was no significant difference in positivity rate among the study communities.
The overall LASV RT-qPCR positivity rate in the non-rodents from Ogun State was 10% (Table 1) with no significant difference between the samples tested in the two study communities (7.7% in Ijebu versus 10.6% in Oke-Aro; p = 1.0).
From the total of 21.7% LASV RT-qPCR positivity rate observed in Oyo State, only two communities [Idi-Ayunre (33.3%) and Olorunshogo (80%)] showed LASV positivity by RT-qPCR.
LASV RT-qPCR results in the different non-rodent species
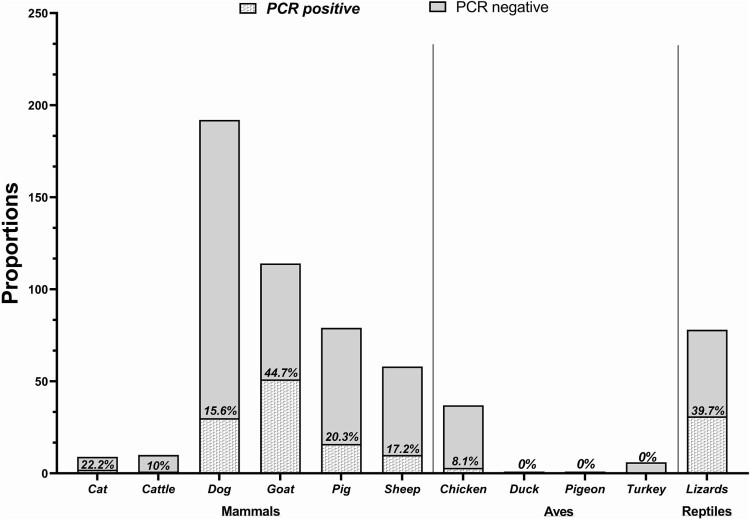
The frequency distribution of LASV positive animals by RT-qPCR are summarized in Figure 2. Among the avian species tested, only chickens were LASV positive (8.1%). The reptiles, represented by lizards only, were 39.7% positive. Interestingly, all genera of non-rodent mammals showed positivity for LASV with the lowest positive rate (1/10; 10%) in cattle and the highest (51/114; 44.7%) in goats. In a pooled data analysis based on the animal classes, LASV positivity rate was significantly higher (p = 0.0002) in lizards (31/78; 39.7%), compared with mammals (110/462; 23.8%) and birds (3/45; 6.7%). Within mammals, LASV positivity rate was significantly higher in goats compared with other animals (p < 0.0001) (Figure 2).
Figure 2.
Prevalence of LASV in non-rodents.
Seasonal variation of LASV infection in non-rodents
Data for seasonal variation in LASV positivity were available only from Ebonyi and Ondo States. Therefore, data from Ogun and Oyo state were excluded from this analysis. There was no significant difference in LASV positivity rate during these two sampling periods (p = 0.23).
LASV RT-qPCR results by sample type
LASV positivity rate was significantly lower in plasma samples compared with other sample types (p = 0.001) with the positivity rates being 7.7% (12/156) using plasma, 16.5% (75/455) using oral swabs, and 20.5% (94/458) using rectal swab samples. Out of the 144 LASV RT-qPCR-positive non-rodents, the positivity rates based on sample types were distributed as 58 (40.3%) rectal swabs, 41 (28.5%) oral swabs, 6 (4.2%) plasma. Two (1.4%) animals were LASV positive with plasma and oral swabs, 4 (2.8%) positive with plasma and rectal swabs, and 33 (22.9%) animals positive with rectal and oral swabs. With the use of oral swabs for LASV detection by RT-qPCR, animals exhibited a total LASV positivity rate of 18.1% with the highest (33.3%; 24/72) recorded in lizards, followed by mammals (14.4%; 49/340) and birds (4.7%; 2/43). In the non-rodent mammals, LASV positive rates from oral swabs were distributed as 0% in cattle, 10.3% in sheep, 13.9% in pigs, 15.9% in goats, 16.7% in cats, and 17.6% dogs. With cattle excluded from the statistical comparison, there was no significant difference in LASV positivity rate with oral swabs across all the non-rodent mammals (p = 0.82). Interestingly, lizards showed a significantly higher LASV positivity using oral swabs compared to other animals (p < 0.0001).
Clinical findings in LASV-positive domestic animals
Most LASV-positive domestic animals examined appeared relatively healthy, though a few were lethargic, slightly emaciated, or cachectic as shown in Supplementary Table S3. Abnormal rapid breathing (tachypnoea) was observed in almost all LASV-positive domestic animals tested (90–97.9%). In particular, there was a significant difference (p < 0.05) in the percentage of LASV-positive animals with tachypnoea versus normal respiratory rate (97.9/2.1%). Although tachypnoea was also recorded in most LASV negative animals, it was significantly higher in LASV-positive goats and dogs (p < 0.04). There was no significant difference in all other clinical findings between LASV-positive and-negative animals tested (Supplementary Table S3).
Seropositivity to Pan-Lassa NP IgG/IgM in non-rodents by study sites
A total of 679 non-rodent mammals (cattle, dogs, goats, pigs and sheep) were tested for LASV IgG using ELISA. Geographical distribution of the mammals tested for LASV by ELISA across the four study states is shown in Supplementary Table S2. The total seropositivity in all animals tested was 10.8% (73 of 679). Though not statistically significant, the prevalence of LASV IgG was highest in Ogun State (14.8%, Supplementary Table S2).
Seropositivity to Pan-Lassa NP IgG/IgM in animals by study communities
Table 2 parses the LASV seropositivity by each study community in the four states; in Ebonyi State, LASV seropositivity rates in mammals varied moderately among communities, ranging from 4.1% in Nkaliki to 23.1% in Onu-Enyim. In Ondo State, LASV seropositivity rates varied from 2.2% in Ijebu-Owo to 13.2% in the Iyere community. In Ogun State, LASV seropositivity rates in the study community ranged from 3.4% in Abeokuta to 25% in Ijebu-Ode and Oke-Aro. In Oyo State, three of the five study communities (Agbowo, Ilu-Tuntun and Olorunshogo) had no seropositivity while the other two (Amosun-Akinyele and Idi Ayunre) had 25% seropositivity each.
Table 2.
LASV seropositivity in non-rodents in Nigeria.
| State |
Study Community |
Total analysed |
No. positive |
% Positivity |
P value |
| Ebonyi | Hausa Quarters | 10 | 1 | 10 | 1.0 |
| Ndinwikwe Iboko | 4 | 0 | 25 | – | |
| Nkaliki | 49 | 2 | 4.1 | 0.03 | |
| Nkwagu | 14 | 1 | 7.1 | 0.48 | |
| Nwezenyi | 117 | 14 | 12 | 0.52 | |
| Odunukwe | 9 | 0 | 12 | – | |
| Onu-Enyim | 65 | 15 | 23.1 | 0.01 | |
| Total | 261 | 35 | 13.4 | - | |
| Ondo | Ehinogbe | 105 | 11 | 10.5 | 0.53 |
| Ijebu | 46 | 1 | 2.2 | 0.08 | |
| Isuada | 64 | 4 | 6.3 | 0.39 | |
| Iyere | 106 | 16 | 15.1 | 0.008 | |
| Total | 321 | 29 | 9 | - | |
| Ogun | Abeokuta | 4 | 1 | 25 | 0.55 |
| Ijebu | 29 | 1 | 3.4 | 0.003 | |
| Oke-Aro | 28 | 7 | 25 | 0.16 | |
| Total | 51 | 9 | 14.8 | - | |
| Oyo | Agbowo | 9 | 0 | 0 | - |
| Amosun-Akinyele | 4 | 1 | 25 | 0.26 | |
| Idi-Ayunre | 4 | 1 | 25 | 0.26 | |
| Ilu-Tuntun | 5 | 0 | 0 | - | |
| Olorunshogo | 7 | 0 | 0 | - | |
| Total | 29 | 2 | 6.9 | - | |
| Grand Total | 679 | 73 | 10.8 | - | |
Note: No., Number, %, percentage.
Pan-Lassa NP IgG/IgM seropositivity by animal species
Overall, LASV seropositivity among non-rodents tested was significantly higher in cattle (p = 0.03) and pigs (p = 0.003) compared to other animals evaluated in this study but the rate was significantly lower in goats (p = 0.04) (Table 3). Evaluating the data by state shows that LASV seropositivity rate was significantly higher in pigs (p = 0.00006) but significantly lower in dogs (p = 0.002) compared with other non-rodents sampled in Ebonyi State. However, in Ondo State, LASV seropositivity rate was significantly higher in cattle and dogs (p = 0.01 each), but significantly lower in goats (p = 0.0009) compared with other animals tested.
Table 3.
Geographic distribution of LASV seropositivity in non-rodents.
| State |
Animal type |
No. analysed |
No. positive |
% Positivity |
P-value |
| Ebonyi | Cattle | 33 | 7 | 21.2 | 0.1 |
| Dog | 89 | 4 | 4.5 | 0.01 | |
| Goat | 89 | 8 | 9 | 0.24 | |
| Pig | 18 | 8 | 44.4 | 0.00002 | |
| Sheep | 39 | 6 | 15.4 | 0.53 | |
| Total | 268 | 33 | 12.3 | - | |
| Ondo | Cattle | 10 | 3 | 30 | 0.05 |
| Dog | 98 | 16 | 16.3 | 0.003 | |
| Goat | 127 | 2 | 1.6 | 0.0008 | |
| Pig | 20 | 2 | 10 | 0.7 | |
| Sheep | 66 | 6 | 9.1 | 0.99 | |
| Total | 321 | 29 | 9 | - | |
| Ogun | Cattle | - | - | - | - |
| Dog | - | - | - | - | |
| Goat | 13 | 0 | 0 | - | |
| Pig | 41 | 7 | 17.1 | 0.7 | |
| Sheep | 7 | 2 | 28.6 | 0.61 | |
| Total | 61 | 9 | 14.8 | - | |
| Oyo | Cattle | 3 | 0 | 0 | - |
| Dog | - | - | - | - | |
| Goat | 3 | 0 | 0 | - | |
| Pig | 21 | 2 | 9.5 | - | |
| Sheep | 2 | 0 | 0 | - | |
| Total | 29 | 2 | 6.9 | - | |
| Overall | Cattle | 46 | 10 | 21.7 | 0.02 |
| Dog | 187 | 20 | 10.7 | 0.98 | |
| Goat | 232 | 10 | 4.3 | 0.0001 | |
| Pig | 100 | 19 | 19 | 0.004 | |
| Sheep | 114 | 14 | 12.3 | 0.56 | |
| Total | 679 | 73 | 10.8 | - |
Note: No., Number, %, percentage.
Comparison between RT-qPCR and ELISA LASV positivity in animals
Of the 392 non-rodents whose samples were analysed for both LASV RT-qPCR and PAN-Lassa NP IgG/IgM ELISA, 265 (67.6%) were negative by both RT-qPCR and ELISA, 91 (23.2%) were positive by ELISA only, 27 (7.4%) by RT-qPCR only, and 7 (1.8%) were positive by both RT-qPCR and ELISA. The animals positive for both assays were dogs (n = 1), goats (n = 3), and pigs (n = 3) (Table 4). Of the seven animals positive by both assays, six were from Ebonyi State, while one (pig) was from Oyo State.
Table 4.
RT-qPCR and ELISA outcomes in non-rodents.
| Analyses outcome | Animal types | |||||
| |
Cattle |
Dog |
Goat |
Pig |
Sheep |
ALL |
| Negative (%) | 6 (50) | 135 (75) | 56 (52.3) | 26 (59.1) | 42 (80.8) | 265 (67.6) |
| ELISA pos Only (%) | 2 (33.3) | 17 (9.4) | 1 (0.9) | 5 (11.4) | 4 (7.7) | 29 (7.4) |
| RT-qPCR pos only (%) | 1 (16.7) | 27 (15) | 47 (43.9) | 10 (22.7) | 6 (11.5) | 91 (23.2) |
| ELISA and RT-qPCR pos (%) | 0 (0) | 1 (0.6) | 3 (2.8) | 3 (6.8) | 0 (0) | 7 (1.8) |
| TOTAL (%) | 9 (100) | 180 (100) | 107 (100) | 44 (100) | 52 (100) | 392 (100) |
Note: ELISA, Enzyme-linked immunosorbent assay; RT-qPCR, Real-Time Quantitative Polymerase Chain Reaction; ALL, all animals; pos, positive.
LASV sequencing in non-rodents
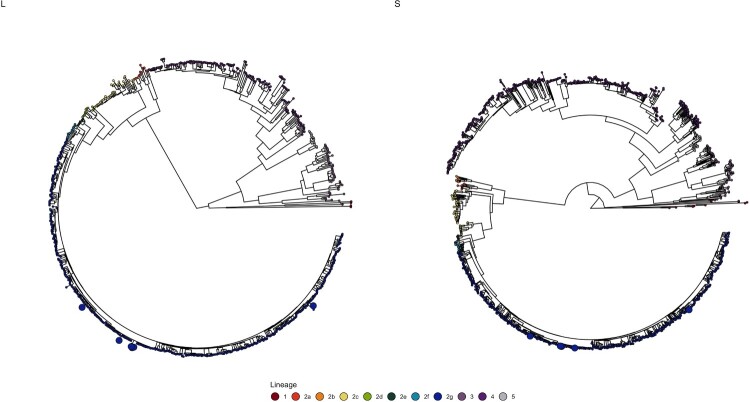
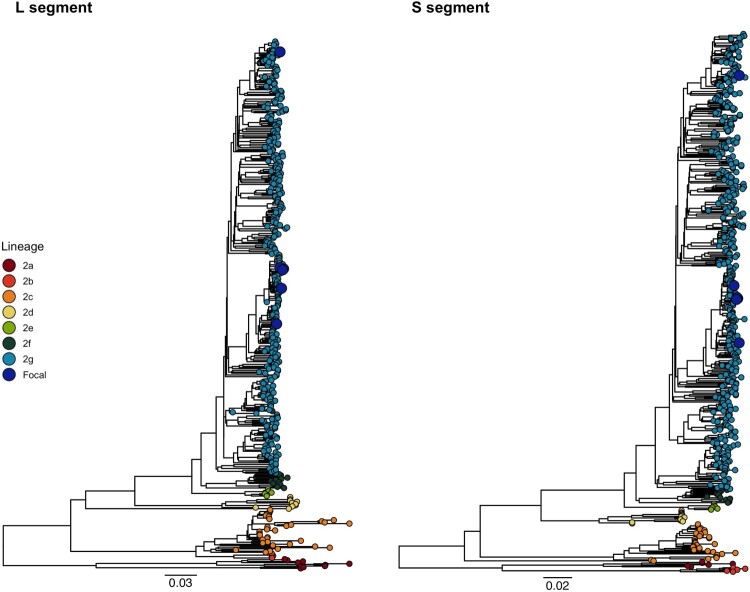
Six whole LASV genomes with the accession numbers BankIt2738696 AINKWGOT002OS-2 OR493499; BankIt2738703 OWEHDOG007OS-2 OR493500; BankIt2738699 AINKWGOT003RS-2 OR493501; BankIt2738701AIODUGOT002RS-2 OR493502; BankIt2738705 OWEHLIZ002CS-2 OR493503; BankIt2738707 OWIYLI013CS-2 OR493504 from three goats, one dog, and two lizards were assembled. We found that all sequences (n = 6 for S segment, n = 6 for L segment) clustered within lineage 2, which circulates predominantly in Southern Nigeria (Figure 3). We also found that our sequences sampled in 2021 from Owo (two lizards and one dog), formed a well-supported monophyletic cluster in the subtree annotated as Sub-lineage 2 g in both the L and S phylogeny (Figure 4). Our LASV sequences obtained from non-rodents in Owo clustered across both segments with human LAVS sequences from patients’ cases in Owo, and the wider Ondo State during the 2017–2018 outbreak. The three LASV sequences obtained from goats in Abakaliki (Ebonyi State) in 2022, were interspersed throughout Sub-lineage 2 g across both segments, clustering with sequences sampled from humans and rodents in Owo from 2017 to 2019. Furthermore, we found that previous sequences from Ebonyi State from Sublineage 2 a–c show substantial divergence to our new sequences across both segments (Figure 4). We did not find any evidence of reassortment in our sequences.
Figure 3.
The L and S segment phylogenies of Lassa virus lineages annotated according to Ehichioya et al. [28]. The sequences generated in this study are highlighted by size. All newly generated sequences fall within lineage 2 sublineage g (in blue). Phylogenies are rooted by midpoint for clarity.
Figure 4.
The L and S segment phylogenies of Lineage 2 annotated according to Ehichioya et al. [28]. The sequences generated in this study are highlighted by size (Shown in larger blue circles).
Discussion
In this LASV zoonotic surveillance study we evaluated the ecological complexity of the virus among a large variety of domestic and non-domestic animals. We report the first detection of LASV by RT-qPCR (21.6% positivity) and serology (11.5% seropositivity) in multiple non-rodents living closely with humans in LF-endemic and non-endemic regions in southern Nigeria. In addition, we report the first complete genomes of LASV obtained from non-rodents and provide evidence that they are infected with the same lineage 2 g of the virus circulating in human populations in southern Nigeria. LASV infection has been reported in numerous small rodent reservoirs [5–7,29] and recently in non-human primates [18]. However, to date, no evidence of the virus in domestic animals other than dogs [30] has been documented, despite their proximity to humans. Our findings indicate that LASV infections occur in previously unreported non-rodent hosts, and that these animals are likely to be full-fledged reservoirs and not just incidental hosts.
In this study, various levels of LASV infection rates in various animals were recorded. Overall, cats and dogs had moderately high LASV positivity (22.2% and 15.6% respectively). This may be because of the predator-prey relationship between cats, dogs and rodents (mice and rats). Dogs and cats often prey on rodents around the house and bushes/field close to the house [31,32] potentially exposing them to these pathogens. Notably, a high LASV positivity was recorded in lizards. This is not surprising because lizards and small rodents are frequently in contact (through exposure to faecal materials and urine) as they are both found in buildings and farms where they forage for the same food and shelter compared to other animals. Moreover, zoonotic bacteria and viruses have previously been isolated from the guts of lizards found living closely with humans and animals [33,34].
Domestic animals, including goats, pigs and chickens, are usually reared in backyard farms in many regions of west Africa, including Nigeria. This is expected because subsistence farming serves as a means of livelihood to many families [35]. Detection of LASV in these farmed animals considering their close contact with humans and other animals, particularly the shared environment, water, and food with small rodent LASV reservoirs, provide opportunities for cross-species infections. Furthermore, zoonosis may occur in humans when pathogens from the wild spill over into livestock, amplify within the livestock and thereafter infect humans during handling, processing, or consumption [29]. In this study, goats had the highest LASV positivity (44.7%), despite their small role in viral zoonosis transmission. Surprisingly, pigs, which have been reported to act as intermediate/amplification hosts for new emerging zoonotic diseases such as Japanese Encephalitis Virus, Influenza virus, Nipah virus and Coronaviruses [37], had a relatively lower LASV positivity of 20.3%. Host plasticity and the abundance of animal hosts can remarkably increase the incidence of disease in humans [36]. Therefore, there is a need for further investigation into the role of goats and other non-rodent animals in LASV transmission.
The positivity to LASV by PCR in non-rodents was highest in Ebonyi State and among mammals, it was highest in goats. Non-rodents, particularly goats and chickens, in sampled communities in Ebonyi State live in human dwellings and share their food. Goats are in constant contact with small rodents and humans in these communities. We hypothesize that the virus likely circulates among those animal taxa and humans, with a potential to cause reverse zoonosis. In Ondo State, the highest LASV positivity was recorded in dogs. In Ondo State, unlike in Ebonyi State, dogs live closely with humans, often in their houses. These findings further emphasize the role contact with small rodents and humans may play in the infection of non-rodent animals.
Although in 2021 and 2022, no reports of human LF infections were reported in Ogun and Oyo [38,39], seroconversion to LASV and its evidence by PCR in these animals suggest that the pathogen circulates among animals in those states. It is likely that LF cases may either be under-reported, undiagnosed, or that transmission to humans is minimal. Genome-wide Association Studies (GWAS) of humans with respect to LF suggest that the Yoruba who form the majority of people living in Southwestern Nigeria (including Oyo and Ogun) are resistant to LASV infections, because of the presence of natural selection signal in the human LARGE gene [40]. However, there is a need for further investigation in these states to elucidate the prevalence and disease ecology of LASV infection in both humans and animals.
Though Happi et al. [7] suggested specific tissues of choice suitable for LASV detection in small rodents, in this study, oral and rectal swabs were determined to be more suitable when compared with plasma. Detection of LASV in non-rodents using the oral and rectal swabs corroborates other studies of viral detections [41–43] and this should also be considered when collecting samples for non-rodent LASV detection. Although most LASV naturally infected domestic animals appeared to be relatively healthy, a few clinical signs were recorded, and these vary slightly from taxa to taxa. Notably, some of these signs were common in most LASV infected animals and were significantly different when compared to LASV negative animals.
Most LASV infected domestic animals showed body temperatures within normal reference range and a relatively high viral cycle threshold, suggesting a low viral load. This is possibly indicative of the animal trying to contain the infection and not showing major clinical signs. This is similar to what is observed in LASV positive non-asymptomatic humans [44,45] and the rodent reservoirs.
The moderate to mild dehydration observed in this study in LASV infected animals has been reported as a consistent clinical finding in NHPs [46]. In addition, abnormal rapid breathing (tachypnoea), which was observed in almost all LASV naturally infected domestic animals sampled in our study, is also a clinical sign consistent with human LF and LASV infection in NHPs [45,46]. However, no clinical signs specific to LASV infection was recorded in the animals examined.
In this study, several animals from each mammalian genus tested, exhibited seroconversion to LASV. While serological data supports the PCR findings of LASV infection in non-rodents, the record of LASV positive animals using both PCR and ELISA suggest that those animals could be infected with different pathogenic variants or strains belonging to different lineages with no cross reactivity or cross protection to infection. There could also be a potential reinfection of the animals by the same viral variant. However, the higher prevalence of LASV-positivity by PCR compared to anti LASV IgG detection suggests that most animals were actively infected.
The sampled animals and the human cases the LASV cluster with phylogenetically most likely resulted from spill-over events from shared common ancestors of the current but severely undersampled diversity circulating in the rodent reservoir [13]. However, without additional sampling of the rodent reservoir and non-rodents, we cannot determine the role non-rodent hosts have in zoonotic infections. It is not clear whether LASV infection in non-rodent animals represents sporadic infections from the rodent reservoir, reverse zoonoses or whether LASV has circulated in these host populations for a longer period. These questions can and will be further addressed by phylodynamic modelling of divergence estimates and discrete trait analyses.
The phylogenetic interspersion of the Abakaliki singletons is expected, as high LASV genetic diversity is maintained by endemic persistence in the rodent reservoirs over a wide geographic range. However, the phylogenetic placement of the Abakaliki sequences is inconsistent with both the geographic structure previously reported in the phylogeny, with Sub-lineage 2 a–c predominating in Ebonyi, and the smaller scale movement of the reservoir [28,47]. The geographic mixture of Sub-lineage 2g evident in our goat sequences suggests that the spatial distribution and movement of the lineage in rodent populations may be less confined than previously thought [48]. It is highly likely that increased systematic sampling of the rodent reservoir and non-rodent animals will result in the discovery of novel diversity and potentially expanded geographic range of sub-lineages [47,49,50].
The genomic confirmation of circulating LASV in domestic animals and lizards and the unravelling of its monophlyletic clustering with lineage 2, which circulates predominantly in Southern Nigeria from humans in Ondo will provide additional valuable information to be used for current public health preventive (early pathogen detection, vaccine design and advocacy prevention) and control measures.
Conclusion
This study reports the first documentation of LASV in various non-rodent animals, suggesting that LASV may also be maintained in non-rodent hosts. The detection of LASV in these animals raises the question of their potential involvement in the transmission and maintenance of LASV in the environment. The identification and genomic characterization of LASV in non-rodents will provide a better insight into the current knowledge of the host-LASV interaction as well as the evolution and diversity of the virus. This will allow for better predictions of future Lassa fever emergence. Lastly, there is a critical need to understand infectivity and transmissibility amongst the various non-rodent animal species identified in this study, and their potential to contribute to human infections. To this end, the fight against LASV infection, a zoonotic disease, strongly requires the employment of the One Health surveillance approach.
Supplementary Material
Acknowledgements
We are grateful to pet owners and small farmers who granted permission to access and sample their animals. We also thank staff of Owo, Veterinary Center, Ondo State, who allowed us to collect samples from sick animals which were brought for treatment in their clinic. We sincerely appreciate all the support staff at ACEGID, too numerous to name here, and other support personnel in the communities visited for their tremendous contributions.
Funding Statement
This work primarily was funded by Emerging Infectious Diseases Branch (EIDB) under Cooperative Agreement with the Henry M. Jackson Foundation (#W81XWH-18-2-0040). This work also received support from a cohort of generous donors through the TED’s Audacious Project, including the ELMA Foundation, MacKenzie Scott, and the Skoll Foundation. Additional support for this work was through grants from the National Institute of Allergy and Infectious Diseases (https://www.niaid.nih.gov), NIH-H3Africa (https://h3africa.org) (award number U01HG007480, and U54HG007480, respectively), the World Bank grants project ACE-019 and ACE-IMPACT. Further support was also received from the Rockefeller Foundation (Grant #2021 HTH), the Africa CDC through the African Society of Laboratory Medicine [ASLM] (Grant #INV018978), and the Science for Africa Foundation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.Monath TP, Newhouse VF, Kemp GE, et al. . Lassa virus isolation from Mastomys natalensis rodents during an epidemic in Sierra Leone. Science. 1974;185(4147):263–265. doi: 10.1126/science.185.4147.263 [DOI] [PubMed] [Google Scholar]
- 2.CDC. Lassa Fever. CDC . 2019. Available from: https://www.cdc.gov/vhf/lassa/index.html.
- 3.Lassa fever Situation report. Cumulative Epi week 35, 2023 and Comparaison with the previous year 2022 . Nigeria Centre for Disease Control and Prevention. Available from: https://ncdc.gov.ng/themes/common/files/sitreps/393479e44be567dfaae3718cceac01ab.pdf.
- 4.Wulff H, Fabiyi A, Monath TP.. Recent isolations of Lassa virus from Nigerian rodents. Bull World Health Organ. 1975;52(4–6):609–613. [PMC free article] [PubMed] [Google Scholar]
- 5.Lecompte E, Fichet-Calvet E, Daffis S, et al. . Mastomys natalensis and Lassa Fever, West Africa. Emerg Infect Dis. 2006;12(12):1971–1974. doi: 10.3201/eid1212.060812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olayemi A, Cadar D, Magassouba N, et al. . New hosts of the Lassa virus. Sci Rep. 2016;6:25280, doi: 10.1038/srep25280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Happi AN, Olumade TJ, Ogunsanya OAet al. . Increased prevalence of lassa fever virus-positive rodents and diversity of infected species found during human lassa fever epidemics in Nigeria. Microbiol Spectr 2022;10(4):e0036622. doi: 10.1128/spectrum.00366-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fichet-Calvet E, Lecompte E, Koivogui L, et al. . Fluctuation of Abundance and Lassa Virus Prevalence in Mastomys natalensis in Guinea, West Africa. Vector Borne Zoonotic Dis. 2007;7(2):119–128. doi: 10.1089/vbz.2006.0520 [DOI] [PubMed] [Google Scholar]
- 9.Adetola OO, Adebisi M.. Impacts of deforestation on the spread of mastomys natalensis in Nigeria. World Scientific News. 2019. [Google Scholar]
- 10.Fisher-Hoch SP, Tomori O, Nasidi A, et al. . Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practice. Br Med J. 1995;311(7009):857–859. doi: 10.1136/bmj.311.7009.857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olayemi A, Obadare A, Oyeyiola A, et al. . Arenavirus Diversity and Phylogeography of Mastomys natalensis Rodents, Nigeria. Emerg Infect Dis. 2016;22(4):687–690. doi: 10.3201/eid2204.150155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Siddle KJ, Eromon P, Barnes KG, et al. . Genomic analysis of Lassa virus during an increase in cases in Nigeria in 2018. N Engl J Med. 2018;379(18):1745–1753. doi: 10.1056/NEJMoa1804498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andersen KG, Shapiro BJ, Matranga CB, et al. . Clinical sequencing uncovers origins and evolution of Lassa virus. Cell. 2015;162(4):738–750. doi: 10.1016/j.cell.2015.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manning JT, Forrester N, Paessler S.. Lassa virus isolates from Mali and the Ivory Coast represent an emerging fifth lineage. Front Microbiol. 2015;6:1037, doi: 10.3389/fmicb.2015.01037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walker DH, Wulff H, Lange JV, et al. . Comparative pathology of Lassa virus infection in monkeys, Guinea-pigs, and Mastomys natalensis. Bull World Health Organ. 1975; 52(4–6):523–534. [PMC free article] [PubMed] [Google Scholar]
- 16.Tang-Huau T-L, Feldmann H, Rosenke K.. Animal models for Lassa virus infection. Curr Opin Virol. 2019; 37:112–117. doi: 10.1016/j.coviro.2019.07.005 [DOI] [PubMed] [Google Scholar]
- 17.Sattler RA, Paessler S, Ly H, et al. . Animal models of Lassa fever. Pathogens. 2020;9(3):197, doi: 10.3390/pathogens9030197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogunro BN, Olugasa BO, Kayode A, et al. . Detection of antibody and antigen for Lassa virus nucleoprotein in monkeys from southern Nigeria. JEpidemiol Glob Health. 2019;9(2):125–127. doi: 10.2991/jegh.k.190421.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meerburg BG, Singleton GR, Kijlstra A.. Rodent-borne diseases and their risks for public health. Crit Rev Microbiol. 2009; 35(3):221–270. doi: 10.1080/10408410902989837 [DOI] [PubMed] [Google Scholar]
- 20.Bonwitt J, Sáez AM, Lamin J, et al. . At home with Mastomys and Rattus: Human-Rodent interactions and potential for primary transmission of Lassa Virus in domestic spaces. Am J Trop Med Hyg. 2017;96(4):935–943. doi: 10.4269/ajtmh.16-0675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shah RR. Rapid response, high-throughput extraction of biosafety Level 4 viral nucleic acids. dashharvardedu 2017. http://nrs.harvard.edu/urn-3:HUL.InstRepos:37736768.
- 22.Matranga CB, Gladden-Young A, Qu J, et al. . Unbiased deep sequencing of RNA viruses from clinical samples. J Vis Exp. 2016;(113):54117, doi: 10.3791/54117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park D, Tomkins-Tinch C, Ye S, et al. Broadinstitute/viral-ngs: v1.25.0. Zenodo. 2019. [accessed 2023 August 14]. Available from: https://zenodo.org/record/3509008.
- 24.Katoh K, Standley DM.. Mafft multiple sequence alignment software version 7: improvements in performance and usability. Mol Biol Evol. 2013;30(4):772–780. doi: 10.1093/molbev/mst010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Minh BQ, Schmidt HA, Chernomor O, et al. . IQ-TREE 2: new models and efficient methods for phylogenetic inference in the genomic era. Mol Biol Evol. 2020;37(5):1530–1534. doi: 10.1093/molbev/msaa015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kalyaanamoorthy S, Minh BQ, Wong TKF, et al. . Model finder: fast model selection for accurate phylogenetic estimates. Nat Methods. 2017;14(6):587–589. doi: 10.1038/nmeth.4285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoang DT, Chernomor O, von Haeseler A, et al. . UFBoot2: improving the ultrafast Bootstrap approximation. Mol Biol Evol. 2018;35(2):518–522. doi: 10.1093/molbev/msx281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ehichioya DU, Dellicour S, Pahlmann M, et al. . Phylogeography of Lassa Virus in Nigeria. J Virol. 2019;93(21):e00929-19. doi: 10.1128/jvi.00929-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yadouleton A, Agolinou A, Kourouma F, et al. . Lassa virus in Pygmy Mice, Benin, 2016–2017. Emerg Infect Dis. 2019;25(10):1977–1979. doi: 10.3201/eid2510.180523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Georges AJ, Gonzalez JP, Abdul-Wahid S, et al. . Antibodies to Lassa and lassa-like viruses in man and mammals in the Central African Republic. Trans R Soc Trop Med Hyg. 1985;79(1):78–79. doi: 10.1016/0035-9203(85)90242-1 [DOI] [PubMed] [Google Scholar]
- 31.Elton CS. The use of cats in farm rat control. The British Journal of Animal Behaviour. 1953;1:151–155. doi: 10.1016/S0950-5601(53)80015-8 [DOI] [Google Scholar]
- 32.Galetti M, Sazima I.. Impact of feral dogs in an urban Atlantic forest fragment in southeastern Brazil. Nat Conserv. 2006;4:146–151. [Google Scholar]
- 33.Ogunleye OA, Ajuwape TP, Alaka OO, et al. . Characterization of a Salmonella enterica serotype Pullorum isolated from a lizard co-habitating with poultry. African Journal of Microbiology Research. 2013;7:1215–1221. doi: 10.5897/AJMR2013.6028 [DOI] [Google Scholar]
- 34.Ajayi JO, Ogunleye AO, Happi AN, et al. . Bacteria isolated from the oral and cloaca swabs of lizards co-habitating with poultry in some poultry farms in Ibadan, Oyo State, Nigeria. Afr J Biomed Res. 2015;18:211–215. [Google Scholar]
- 35.Swanepoel F, Stroebel A, Moyo S. The role of livestock in developing communities: enhancing multifunctionality competitiveness of smallholder livestock producers in Botswana View project. 2010.
- 36.Karesh WB, Dobson A, Lloyd-Smith JO, et al. . Ecology of zoonoses: natural and unnatural histories. Lancet. 2012;380(9857):1936–1945. doi: 10.1016/S0140-6736(12)61678-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McLean RK, Graham SP.. The pig as an amplifying host for new and emerging zoonotic viruses. One Health. 2022;14:100384, doi: 10.1016/j.onehlt.2022.100384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nigeria Centers for Disease Control and Prevention . Lassa fever Situation Report. 2021 https://ncdc.gov.ng/themes/common/files/sitreps/54f285bdd8e7a0370151c2ff9332c30a.pdf.
- 39.Nigeria Centre for Disease Control Lassa fever Situation Report. Epi Week 50 . 12–18 December 2022 – Nigeria | ReliefWeb. reliefweb.int. 2023. https://reliefweb.int/report/nigeria/ncdc-lassa-fever-situation-report-epi-week-50-12-18-december-2022.
- 40.Andersen KG, Shylakhter I, Tabrizi S, et al. . Genome-wide scans provide evidence for positive selection of genes implicated in Lassa fever. Philos Trans R Soc, B. 2012 Mar 19;367(1590):868–877. doi: 10.1098/rstb.2011.0299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bjustrom-Kraft J, Woodard K, Giménez-Lirola L, et al. . Porcine epidemic diarrhea virus (PEDV) detection and antibody response in commercial growing pigs. BMC Vet Res. 2016;12:99. doi: 10.1186/s12917-016-0725-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smoľak D, Šalamúnová S, Jacková A, et al. . Analysis of RNA virome in rectal swabs of healthy and diarrheic pigs of different age. Comp Immunol Microbiol Infect Dis. 2022;90–91:101892. doi: 10.1016/j.cimid.2022.101892 [DOI] [PubMed] [Google Scholar]
- 43.Walczak M, Szczotka-Bochniarz A, Żmudzki J, et al. . Non-Invasive sampling in the aspect of African swine fever detection – a risk to accurate diagnosis. Viruses. 2022;14(8):1756, doi: 10.3390/v14081756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fisher-Hoch SP, Craven RB, Forthall DN, et al. . Safe intensive-care management of a severe case of Lassa fever with simple barrier nursing techniques. Lancet. 1985;326(8466):1227–1229. doi: 10.1016/s0140-6736(85)90752-4 [DOI] [PubMed] [Google Scholar]
- 45.Downs IL, Shaia CI, Zeng X, et al. . Natural history of aerosol induced Lassa fever in non-human primates. Viruses. 2020;12(6):593, doi: 10.3390/v12060593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hensley LE, Smith MA, Geisbert JB, et al. . Pathogenesis of lassa fever in cynomolgus macaques. Virol J. 2011;8:205, doi: 10.1186/1743-422x-8-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Klitting R, Kafetzopoulou LE, Thiery W, et al. . Predicting the evolution of the Lassa virus endemic area and population at risk over the next decades. Nat Commun. 2022;13(1):5596, doi: 10.1038/s41467-022-33112-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mariën J, Kourouma F, Magassouba N, et al. . Movement patterns of Small Rodents in Lassa fever-endemic villages in Guinea. EcoHealth. 2018;15(2):348–359. doi: 10.1007/s10393-018-1331-8 [DOI] [PubMed] [Google Scholar]
- 49.Simons D. Lassa fever cases suffer from severe underreporting based on reported fatalities. Int Health. 2023;15(5):608–610. doi: 10.1093/inthealth/ihac076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arruda LB, Free HB, Simons D, et al. . Current sampling and sequencing biases of Lassa mammarenavirus limit inference from phylogeography and molecular epidemiology in Lassa fever endemic regions. PLOS Glob Public Health. 2023;3(11):e0002159. doi: 10.1371/journal.pgph.0002159 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.