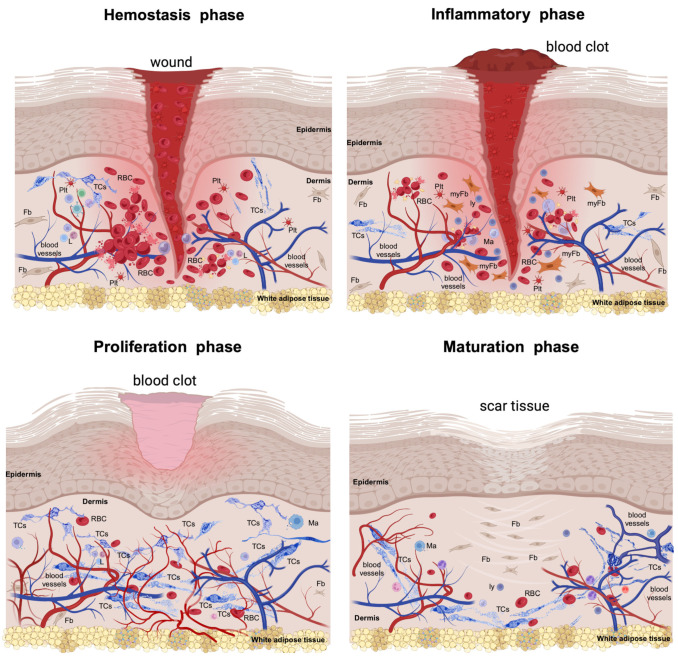
Figure 1.
The injury of the skin triggers a series of physiologic and morphological events for repairing the injured structures. This cascade of healing falls into four overlapping phases. The hemostasis phase (primarily about coagulation) is acute and begins with injury, followed by the formation of the blood clot that dams the bloodshed; the platelets become activated by their contact with basement membranes and collagen fibres and begin aggreging. Thrombin initiates the formation of the fibrin mesh. The inflammatory phase (which is mainly about removing the cellular debris) is orchestrated by neutrophils and macrophages and their variegated secretory panel. Clinically, it lasts about 6 days and the Celsus cardinal signs feature this phase. The proliferative phase (which is about filling and covering the skin defect) structurally features the formation of the granular tissue and neoangiogenesis and wound covering by the neighbouring epithelial cells. All these intricate processes can last about 3 weeks. In both the inflammatory and proliferative phases, the formerly destroyed network of interstitial cells (including telocytes, TCs) is restored to its initial parameters. The maturation phase (dominated by structural remodelling and reorganization processes) is the longest-lasting and is dominated by the rearrangement and maturation of the collagens, increasing the tensile strength. Thus, the cellular architects of the phase are the fibroblasts (Fbs) and fibrocytes. RBC—red blood cell; Plt—platelets; L—leukocytes; myFb—myofibroblast; ly—lymphocytes. The image was created with BioRender.com.