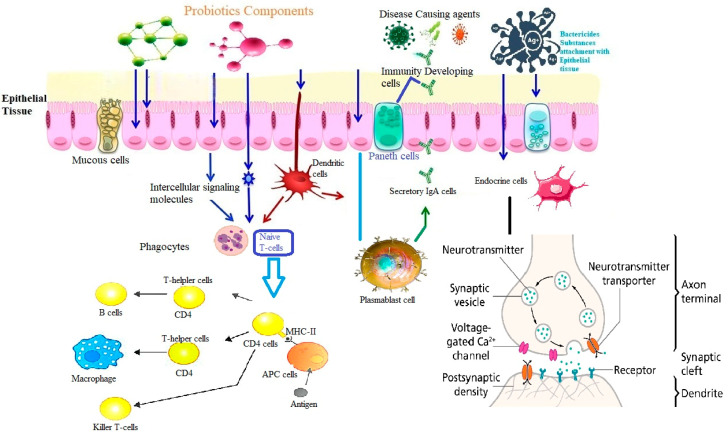
Figure 6.
Probiotics and immune system of the gut—Shortline description of the immune—modulatory activity of probiotic: Probiotic components are stimulated through intercellular signaling or through neuro-transmitters the proliferation and chemiotaxis of immune cells series such as dendritic cells (DCs), macrophages, CD4, B and T lymphocyte or generally antigen-presenting cells (APCs). Specialized cells (Microfold-M cells) located in the epithelium overlying Peyer’s patch, receive the antigens and then, with the help of probiotics, they are transferred to the DCs, where the activation process of CD8+/CD4+ naïve T cells and direct helper T cell responses towards Th1, Th2, Th17, or regulatory patterns, is triggered. Once disease-causing agents appear in the GIT, probiotic bacteria are involved in the production of antibodies by plasm-blast cells (or short-lived plasma cells) and activate the Paneth cells in the Lieberkuhn crypts to produce antimicrobial peptides. In addition, probiotic bacteria have the ability to stimulate the production of IgAs in the intestinal lumen, contributing to the enhancement of mucosal and systemic immunity. Finally, stimulation and subsequent signaling of intestinal endocrine cells (EECs) by probiotics can be observed. Enteroendocrine cells produce various hormones which are stored in vesicles within the EECs. The release of these hormones is a regulated process that involves membrane depolarization and calcium influx into the cells.