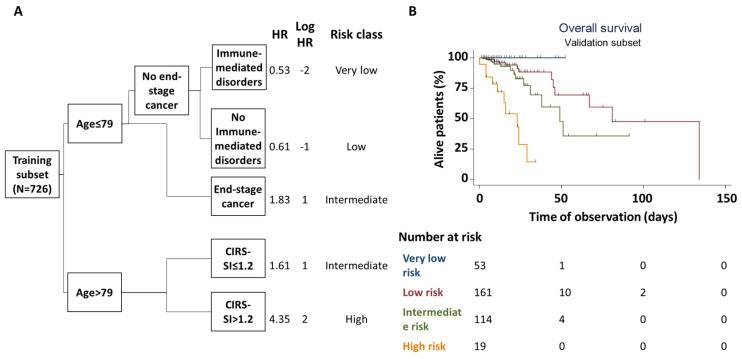
Figure 1.
Multivariate derivation and validation of factors associated with in-hospital mortality. (A) depicts the classification and regression tree analysis for in-hospital mortality in the training subset. The model included age, ADL/IADL dependency, cardiovascular disorders, immune–mediated disorders, end-stage cancer, admission from nursing homes or ICUs, average cumulative illness rating scale severity index (CIRS-SI), average nine equivalents of manpower score (NEMS), circulation support with at least one vasoactive drug. Only age, CIRS-SI, end-stage cancer and (absence of) immunological disorders were identified as significant strata for patient risk classification. Based on derived, log-transformed hazard ratios (HR), four risk groups were defined (very low risk, blue; low risk, red; intermediate risk, green; high risk, orange). This classification was then applied to patients in the validation subset (B) to assess its performance in identifying patients at higher vs. lower risk of in-hospital death. Cox’s regression analysis in this subset confirmed the significant correlation between the derived risk classification and the actual risk of in-hospital mortality (Log rank = 24.91; p < 0.001).