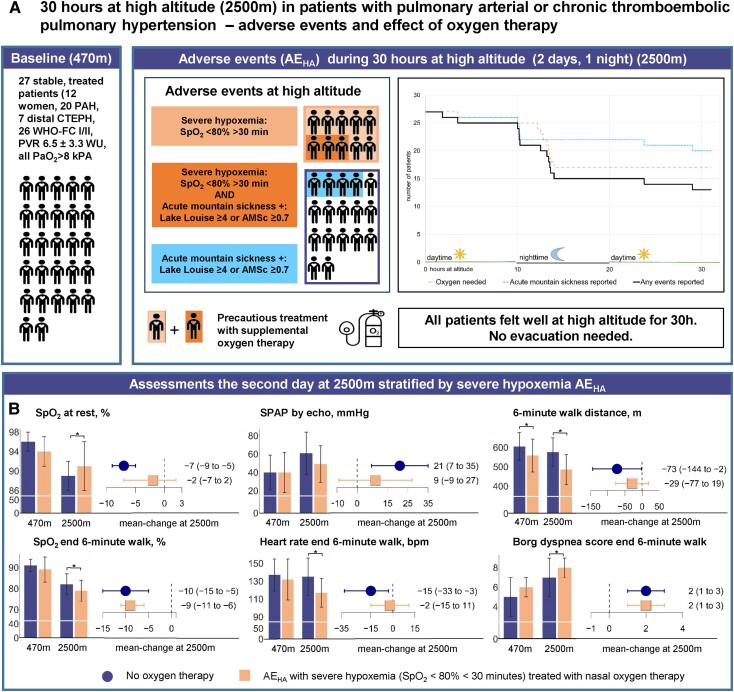
Figure 1.
(A) Baseline characteristics of 27 patients with pulmonary vascular disease defined as pulmonary arterial hypertension or distal chronic thromboembolic pulmonary hypertension are shown (left sector, WHO-FC, WHO dyspnoea functional class; PVR, pulmonary vascular resistance; PaO2, partial pressure of oxygen in arterial blood). Adverse events at high altitude (AEHA) including severe hypoxaemia and acute mountain sickness are graphically illustrated (middle sector). The sector on the right reveals the time to AEHA overall (solid black line) and stratified for patients with severe hypoxaemia treated with supplemental oxygen therapy (long dashed orange line) and those with acute mountain sickness without severe hypoxaemia (dotted blue line), with colours corresponding to the illustration in the middle sector. (B) Assessments at 470 and 2500 m are shown stratified for patients without supplemental oxygen therapy at 2500 m (left dark blue bars and whiskers) and patients with severe hypoxaemia AEHA at 2500 m (right orange bars and whiskers). Bars at the left of each of the six subpanels represent means and standard deviations, whiskers represent mean difference and 95% confidence interval. *Significant difference (P < .05) as calculated by a mixed-linear regression model by intervention (2500 vs. 470 m) corrected for the intervention sequence as a fixed effect and subjects as a random effect. SPAP, systolic pulmonary artery pressure assessed from tricuspid regurgitation velocity without adding right atrial pressure by echocardiography