Abstract
A 62-year-old male was transferred to our hospital complaining of palpitations. His heart rate was 185/min. Electrocardiogram showed a narrow QRS regular tachycardia and the tachycardia changed spontaneously to another narrow QRS tachycardia with two alternating cycle lengths. The arrhythmia was stopped by the administration of adenosine triphosphate. Findings from electrophysiological study suggested that there was an accessory pathway (AP) and dual atrioventricular (AV) nodal pathways. After AP ablation, any other tachyarrythmias were not induced. We supposed that the tachycardia was paroxysmal supraventricular tachycardia involving AP and anterograde conduction alternating between slow and fast AV nodal pathways.
Keywords: paroxysmal supraventricular tachycardia, regularly irregular narrow QRS tachycardia, accessory pathway, dual atrioventricular nodal pathway
Introduction
Paroxysmal supraventricular tachycardia (PSVT) is known as a narrow or wide QRS regular tachycardia and can be treated by catheter ablation. There are few reports of PSVT with two alternating cycle lengths (CLs) being treated by accessory pathway (AP) ablation. Here, we report a case of successful catheter ablation for PSVT that is shown as a regularly irregular narrow QRS tachycardia.
Case Report
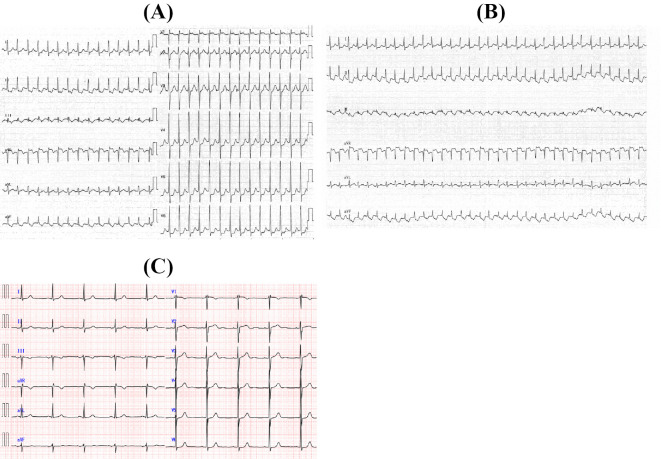
A 62-year-old male was transferred to our hospital complaining of palpitations. He had undergone mitral valve plasty and surgical pulmonary vein isolation due to mitral valve regurgitation and paroxysmal atrial fibrillation 1 year earlier. He had suffered from recurrent palpitations for 4 months. His palpitations had sudden onset and sudden stop. His heart rate was 185/min, blood pressure was 131/96 mmHg, and SpO2 was 99% (room air). Physical examination revealed a systolic murmur at the apical site. Electrocardiogram (ECG) showed a narrow QRS regular tachycardia (Fig. 1A). The tachycardia changed spontaneously to a regularly irregular narrow QRS tachycardia with two alternating CLs (Fig. 1B). The tachycardia was stopped with the administration of adenosine triphosphate (ATP). There was no delta wave on the ECG of sinus rhythm (Fig. 1C). Laboratory data were within normal limits, except for brain natriuretic peptide, which was 120 pg/mL. Chest X-ray did not show cardiomegaly. Echocardiography revealed normal left ventricular function and mild mitral regurgitation. The patient was admitted to our hospital to undergo electrophysiology study (EPS) and catheter ablation.
Figure 1.
ECGs of this patient. (A) Regular tachycardia. (B) Regularly irregular tachycardia. (C) Sinus rhythm. There were no delta waves.
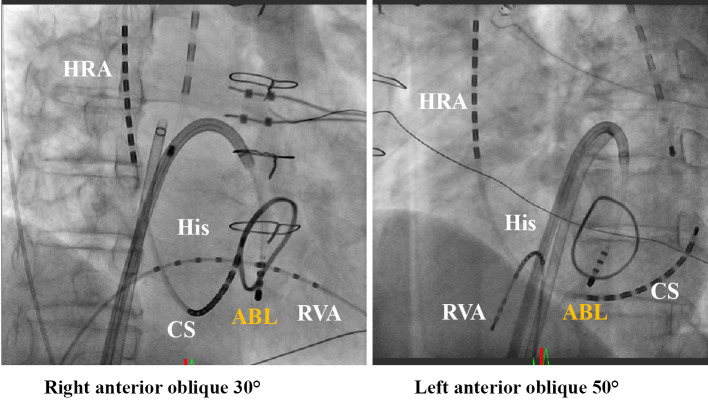
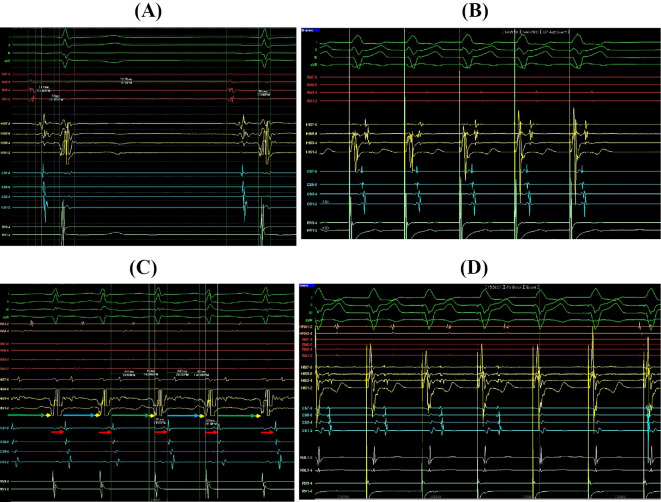
Catheter locations are shown (Fig. 2). Baseline intracardial ECG is shown (Fig. 3A). Ventriculoatrial (VA) conduction was positive (Fig. 3B). The earliest atrial activation site of retrograde conduction was the proximal coronary sinus (CS). VA conduction did not show decremental conduction. During incremental ventricular pacing, 1:1 VA conduction occurred up to 200 ppm and 2:1 VA conduction was observed from 210 ppm. ATP did not create VA block. These findings suggested that the AP was located posterior septal of the mitral annulus. High right atrium (HRA) pacing easily initiated narrow QRS regular tachycardia in which the CL was 330 ms. The tachycardia changed spontaneously to a regularly irregular narrow QRS tachycardia with two alternating CLs. The CLs changed from 330 ms to 370 ms (Fig. 3C). Atrial-His (AH) intervals alternately changed from 207 ms (Fig. 3C blue arrow) to 247 ms (Fig. 3C green arrow). Hisventricle (HV) and VA intervals were fixed at 42 ms and 81 ms respectively. The sequence of all VA conduction was the same and the earliest atrial activation site of retrograde conduction was the proximal CS. Checking the reset phenomenon was difficult because the CL changed alternately. We tried to measure the changing VA interval by para-Hisian pacing but were unable to because of the immediate initiation of clinical PSVT upon para-Hisian pacing. We were also unable to check the dual AV nodal conduction before AP ablation because HRA pacing easily initiated PSVT. Although the information on AV nodal conduction was unclear, we supposed that retrograde AP conduction was necessary to maintain this tachyarrythmia. We decided to perform AP ablation first and to check the AV nodal conduction after. We ablated the mitral annulus at the 6 o'clock point (Fig. 2). Kent block was achieved. After AP ablation, VA conduction was still positive. But the earliest activation site of VA conduction changed (His 5-6) (Fig. 3D). VA conduction showed decremental conduction and ATP made VA block. Extra-stimulus pacing from the HRA showed the jump-up phenomenon with no echo. These findings suggested that there was dual AV nodal conduction. After AP ablation, no tachyarrythmias were induced.
Figure 2.
Fluoroscopic imaging of the catheters. HRA: high right atrium, His: his bundle, RVA: right ventricle apex, CS: coronary sinus, ABL: ablation catheter
Figure 3.
Intracardiac electrograms; right atrium (RA), His-bundle 1-2 dipole placed at His bundle distal region, His 3-4, His 5-6, His 7-8 placed at His bundle proximal region, coronary sinus 1-2 dipole placed at CS distal region, CS 3-4, CS 5-6, CS 7-8 dipole placed at CS proximal, and right ventricle apex. (A) Baseline intracardiac ECG. AH interval was 117 ms, HV interval was 33 ms, QRS duration was 80 ms and A-A interval was 1,270 ms. (B) VA conduction before ablation. Earliest atrial activation site was CS proximal. (C) Regularly irregular tachycardia. All HV and VA intervals were 42 ms (yellow arrow) and 81 ms (red arrow) respectively. AH intervals were alternating from 207 ms (blue arrow) to 247 ms (green arrow). (D) VA conduction after AP ablation when administrating ATP. Earliest atrial activation site changed to His 5-6. ATP made VA block.
We supposed that this PSVT was composed of an AP located posterior septal of the mitral annulus and antegrade conduction alternating between slow and fast AV nodal pathways. We decided not to perform slow pathway ablation based on the EPS findings. At the 1 year follow-up, the patient reported no further palpitations.
Discussion
This report suggests two important findings. First, PSVT can present as a narrow QRS tachycardia with two alternating CLs when composed of both AP and dual AV nodal pathways. Second, AP ablation alone may be sufficient to treat this kind of PSVT.
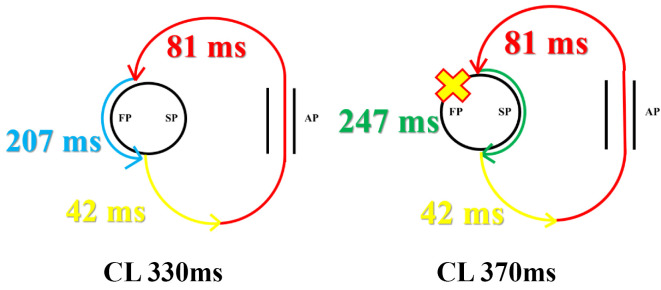
EPS showed that the patient had an AP located posterior septal of the mitral annulus and dual AV nodal pathways. The tachycardia showed 1:1 AV conduction; alternating CLs of 330 ms and 370 ms (RR alternans), alternating AH intervals of 207 ms and 247 ms (AH alternans), and fixed HV and VA intervals of 42 ms and 81 ms respectively. From these findings the tachycardia can be explained as orthodromic atrioventricular reentrant tachycardia (AVRT) involving the posterior septal mitral annulus AP with antegrade conduction alternating between slow and fast AV nodal pathways (Fig. 4). Because of the refractory period of the fast pathway, VA conduction was too early to make the AV nodal fast pathway react every time. The existing slow pathway might have been needed to maintain this PSVT, and the tachycardia then exhibited two alternating CLs. It was reported that the coexistence of dual AV nodal pathways in patients with Wolff-Parkinson-White syndrome or a concealed bypass tract is 12% (1). They suggested that 12% of AVRT could exhibit regularly irregular narrow QRS tachycardia. These findings suggested that there might be more cases than expected that exhibit AVRT with antegrade conduction alternating between slow and fast AV nodal pathways.
Figure 4.
Image of PSVT with two alternate CL. HV interval (yellow arrow) and VA interval (red arrow) were the same. AH interval was 207 ms when AVRT conducted the fast pathway (bule arrow). The fast pathway could not react to the return of VA conduction because of its refractory period. Therefore AVRT conducted the slow pathway, and its interval was 247 ms (green arrow). FP: fast pathway, SP: slow pathway, AP: accessory pathway
Although this patient had AP and dual AV nodal pathways, we performed AP ablation only. The treatment choices for this tachycardia were AP ablation, slow pathway ablation, or both. Because no echo after the jump-up phenomenon was observed, we did not perform slow pathway ablation. To the best of our knowledge, there have only been two reports of PSVT involving AP with antegrade conduction alternating between slow and fast AV nodal pathways successfully treated by AP ablation alone (2,3). These reports did not mention whether they checked for no echo after the jump-up phenomenon or not and long term result. It is important to check for echo after the jump-up phenomenon in order to decide whether slow pathway ablation is needed or not. In this case, after only AP ablation, this patient has not suffered from further palpitations and no tachycardias have been documented during the 1 year follow-up period. This relatively long-term follow-up case suggests that AP ablation may be sufficient to treat this kind of tachyarrythmia.
Conclusion
We experienced a rare case of successful catheter ablation for paroxysmal supra ventricular tachycardia with two alternating CLs treated by AP ablation only.
The authors state that they have no Conflict of Interest (COI).
References
- 1. Csanadi Z, Klein GJ, Yee R, Thakur RK, Li H. Effect of dual atrioventricular node pathways on atrioventricular reentrant tachycardia. Circulation 91: 2614-2618, 1995. [DOI] [PubMed] [Google Scholar]
- 2. Mohanan Nair KK, Namboodiri N, Banavalikar B, et al. Narrow QRS tachycardia with RR alternans: what is the mechanism? Pacing Clin Electrophysiol 39: 1148-1149, 2016. [DOI] [PubMed] [Google Scholar]
- 3. Meryem K, Ahmet K, Emin K, et al. Tachycardia cycle length alternans during a narrow QRS complex tachycardia with eccentric retrograde atrial activation sequence: what is the mechanism? J Arrhythm 91: 209-210, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]