Fig. 4—
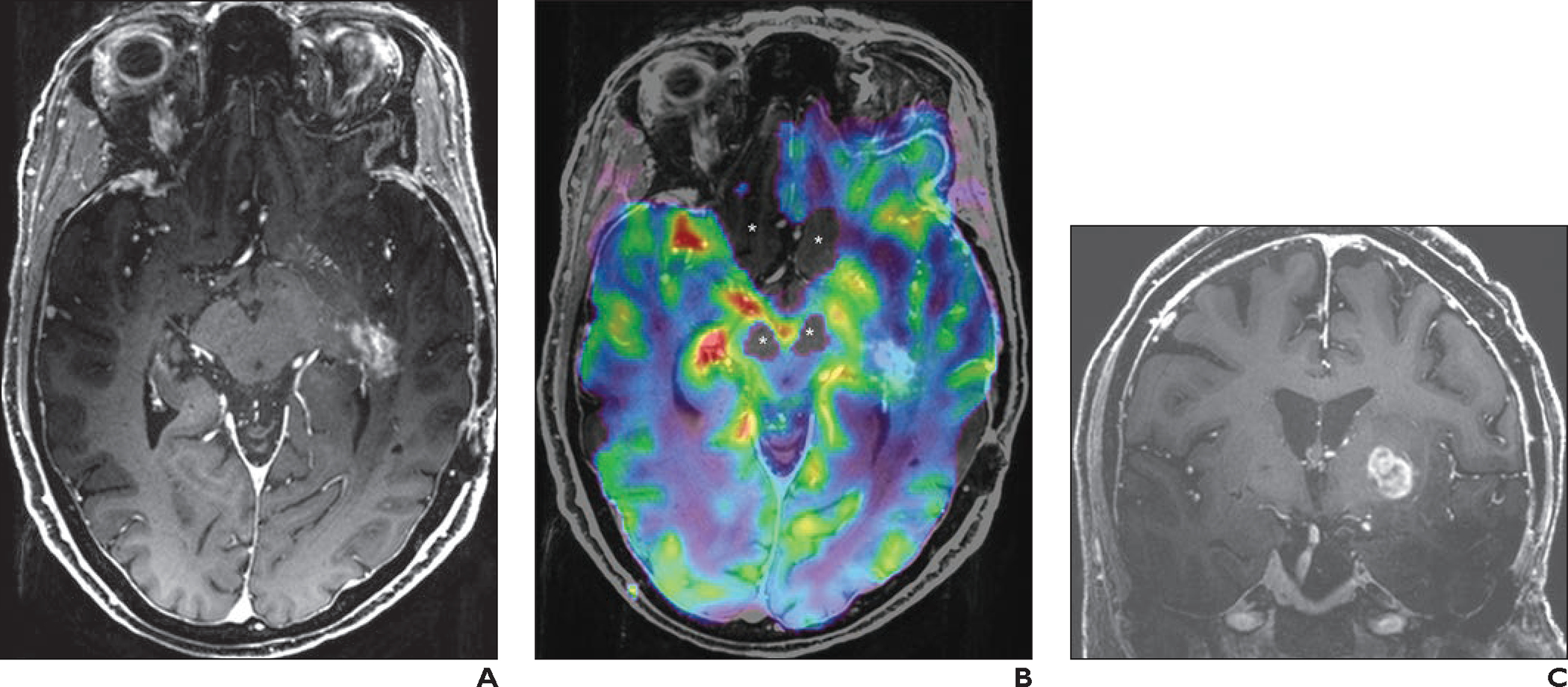
69-year-old woman with history of left temporal lobe low-grade oligoastrocytoma who had undergone resection and radiotherapy. Follow-up imaging was stable until new patchy enhancement was identified in left temporal lobe 16 years after surgery. This patchy enhancement remained stable on follow-up MRI examinations for 2 years. Patient then developed new seizures and was referred for 7-T MRI with dynamic susceptibility contrast perfusion imaging.
A, Axial contrast-enhanced 3D T1-weighted MP-RAGE image shows patchy enhancing area in left temporal lobe, which was stable in comparison with prior examinations (not shown).
B, Fused axial 3D T1-weighted MP-RAGE and relative cerebral blood volume (rCBV) map shows lesion (blue). Perfusion signal is lacking near skull base (asterisks), attributable to susceptibility effects.
C, Coronal contrast-enhanced 3D T1-weighted MP-RAGE image shows new enhancing mass in left basal ganglia.
D, Coronal fused 3D T1-weighted MP-RAGE and rCBV map image shows markedly increased perfusion (yellow, red) corresponding to enhancing lesion in C. Because rCBV map is obtained with thin slices (1.6 mm), coronal reformatted images do not show significant staircase artifact. Perfusion signal is lacking near lower portions of temporal lobes (arrow) owing to susceptibility effects.
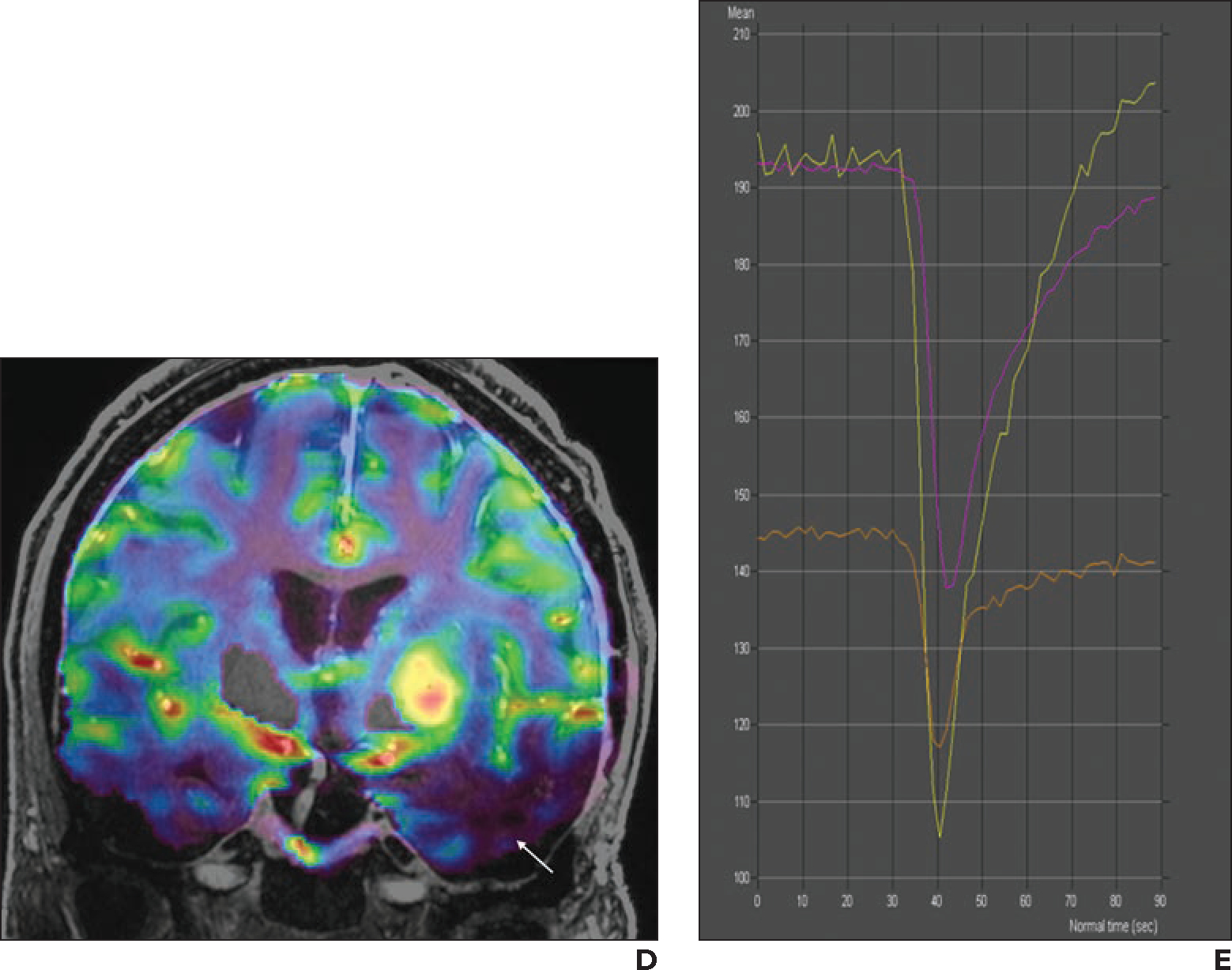
E, Screenshot shows perfusion graph. Yellow line indicates left basal ganglion lesion (corresponding to D, mean rCBV, 474); purple line indicates left temporal lobe lesion (corresponding to B, mean rCBV, 223); orange line indicates normal-appearing contralateral white matter (mean rCBV, 139). Ratio of mean rCBV between lesion and contralateral white matter is 3.4 for left basal ganglion lesion and 1.6 for left temporal lobe lesion. On basis of perfusion data, left basal ganglion lesion was considered to represent malignant tumor, and left temporal lobe lesion was considered to represent radiation necrosis. Patient declined biopsy of left basal ganglion lesion and was referred to hospice.
