Abstract
The aim of this review is to summarise evidence that became available after publication of the 2017 European Respiratory Society statement on the diagnosis and management of obstructive sleep apnoea syndrome (OSAS) in 1- to 23-month-old children. The definition of OSAS in the first 2 years of life should probably differ from that applied in children older than 2 years. An obstructive apnoea–hypopnoea index >5 events·h−1 may be normal in neonates, as obstructive and central sleep apnoeas decline in frequency during infancy in otherwise healthy children and those with symptoms of upper airway obstruction. A combination of dynamic and fixed upper airway obstruction is commonly observed in this age group, and drug-induced sleep endoscopy may be useful in selecting the most appropriate surgical intervention. Adenotonsillectomy can improve nocturnal breathing in infants and young toddlers with OSAS, and isolated adenoidectomy can be efficacious particularly in children under 12 months of age. Laryngomalacia is a common cause of OSAS in young children and supraglottoplasty can provide improvement in children with moderate-to-severe upper airway obstruction. Children who are not candidates for surgery or have persistent OSAS post-operatively can be treated with positive airway pressure (PAP). High-flow nasal cannula may be offered to young children with persistent OSAS following surgery, as a bridge until definitive therapy or if they are PAP intolerant. In conclusion, management of OSAS in the first 2 years of life is unique and requires consideration of comorbidities and clinical presentation along with PSG results for treatment decisions, and a multidisciplinary approach to treatment with medical and otolaryngology teams.
Tweetable abstract
Management of OSAS in the first 2 years of life is unique and requires consideration of comorbidities and clinical presentation, PSG results for treatment decisions, and a multidisciplinary approach to treatment with medical and otolaryngology teams. https://bit.ly/3tjcgDt
Background
Obstructive sleep apnoea syndrome (OSAS) is characterised by recurrent events of partial or complete upper airway obstruction (hypopnoeas and obstructive or mixed apnoeas) accompanied by intermittent hypoxaemia and frequent arousals during sleep [1]. In 2- to 18-year-old children, OSAS is defined as a polysomnography (PSG)-obtained obstructive apnoea–hypopnoea index (oAHI) ≥2 events·h−1 or an obstructive apnoea index ≥1 events·h−1 of total sleep time in the presence of sleep disordered breathing (SDB) symptoms. Alternatively, OSAS can be defined as SDB symptoms in combination with an AHI ≥1 events·h−1 of total sleep time [2]. AHI and oAHI are expected to be numerically similar in otherwise healthy children aged 2–18 years without OSAS or control of breathing disorders, as central sleep apnoeas are uncommon in this age group [3]. In addition, central sleep apnoeas frequently accompany OSAS and they resolve post-adenotonsillectomy [4].
In 2017, a European Respiratory Society (ERS) Task Force prepared a statement summarising published literature on the diagnosis and management of OSAS in 1- to 23-month-old children [1]. Subsequently, several new studies provided evidence which may modify the clinical approach to OSAS in young children. Accumulating evidence suggests that the definition of OSAS in children 2 years of age or younger should differ from that applied in children older than 2 years affected by SDB symptoms due to the evolving characteristics of the sleep–wake state and their effects on respiratory parameters in combination with the predisposition of young children to obstructive and central respiratory events during sleep [5]. Neonates manifest fragmented sleep that progressively consolidates to night-time sleep and two daytime naps by late infancy [6]. Each sleep cycle in neonates lasts 30–70 min with predominantly active (rapid eye movement (REM)) sleep onset, in contrast to infants older than 2 months and children who have cycles of 75–90 min duration with non-REM sleep onset [7]. Full-term neonates spend 50–80% of total sleep time in active (REM) sleep that decreases gradually to <50% by the first year of life [8]. Active (REM) sleep predisposes young infants to respiratory events [5, 9–12]. Therefore, reference values for PSG respiratory parameters and OSAS definition and severity classification in children 2 years of age or younger should probably differ from those applied in older children [2, 13]. In a survey of sleep medicine physicians practising mostly in the USA, there was no agreement on the oAHI cut-off value defining OSAS in neonates and infants [14]. Proposed values varied from 1 to 20 events·h−1. Both OSAS definition and severity classification are of clinical importance when indications for treatment are discussed. Therefore, the aims of the present review article are: 1) to summarise studies reporting reference values for parameters of PSG, polygraphy and nocturnal oximetry in the first 2 years of life; 2) to emphasise the need for age-adjusted cut-off values of PSG, polygraphy and nocturnal oximetry parameters for the diagnosis and severity classification of OSAS in the first 2 years of life; 3) to review the application of diagnostic modalities like drug-induced sleep endoscopy (DISE) for determining the pathogenesis and severity of upper airway obstruction in young children and indications for treatment; and 4) to discuss progress in the nonsurgical and surgical therapeutic interventions for OSAS in young children, such as high-flow nasal cannula (HFNC), positive airway pressure (PAP) therapy and supraglottoplasty.
Literature search
Several studies including infants were performed between 1981 and 2001, and scoring of recordings was not based on the American Academy of Sleep Medicine (AASM) scoring rules or hypopnoeas were not identified [15]. The literature search for the current article was focused on studies published after 1 January 2016 because older literature was reviewed in the ERS statement on the diagnosis and management of OSAS in 1- to 23-month-old children [1].
An initial literature search was completed using the terms “(polysomnography and reference values) or (polysomnography and normative values) or (polygraphy and reference values) or (polygraphy and normative values) or (oximetry and reference value) or (oximetry and normative values)” with filters “birth-18 years”, “1/1/2016-2/28/2023” and “English”. We obtained 102 records and retained seven of them that provided reference values in healthy children 2 years of age or younger [16–22]. Studies on pre-term infants or those with fewer than 10 participants were excluded. A pilot study determining reference data for overnight oximetry in neonates was also excluded because recordings were collected both during sleep and wakefulness [22].
The second literature search included the term “sleep apnoea” with filters “1/1/2016-2/28/2023”, “birth-23 months” and “English”, and provided 752 references, of which six provided longitudinal PSG or polygraphy data of subjects with OSAS [23–28]. The third literature search included the terms “sleep apnoea”, “nasopharyngeal airway”, “continuous positive airway pressure”, “non-invasive ventilation”, “high flow nasal cannula”, “drug induced sleep endoscopy”, “adenotonsillectomy”, “adenoidectomy”, “tonsillectomy” and “supraglottoplasty” with the same filters.
AHI or oAHI for the diagnosis of OSAS in 1- to 24-month-old children? Are there published reference values?
In the ERS statement for OSAS in young children, it was emphasised that the 95th percentile for the central apnoea index (CAI) varies widely according to age and for this reason it has been suggested that the definition of OSAS in 1- to 23-month-old children is usually based on the oAHI [1]. This concept has been reinforced in a recent study by Stefanovski et al. [21] which showed that 39% of the AHI value in 1-month-old infants can be attributed to the CAI and a similar finding has been reported in an older study by Daftary et al. [17]. At the age of 5 months, mean AHI decreased by 75% and a third of this reduction was secondary to a decreased CAI. PSG scoring in both cohorts of healthy infants was consistent with the most recent AASM rules for the scoring of sleep and associated events [29].
However, the oAHI also incorporates hypopnoeas as demonstrated by Daftary et al. [17]. Hypopnoeas may be of the obstructive or of the central type, with the former corresponding to 53% of the oAHI value in neonates [21]. Stefanovski et al. [21] showed that at the age of 1 month, total AHI consists of central apnoeas (36%), obstructive and mixed apnoeas (24%), obstructive hypopnoeas (30%), and central hypopnoeas (10%). In several publications involving infants and frequently in everyday clinical practice, oAHI incorporates both obstructive and central hypopnoeas.
Since obstructive events in healthy infants are overall brief in duration, Daftary et al. [30] have proposed the calculation of the time in airway obstruction (TAO) during PSG to quantitate the obstructive component of the AHI. TAO during PSG is calculated as: ((total number of obstructive apnoeas×mean duration (s) of obstructive apnoeas)+(total number of hypopnoeas×mean duration (s) of hypopnoeas))/total sleep time (s) [30]. Few studies providing reference values for PSG, polygraphy and nocturnal oximetry parameters from otherwise healthy children aged 2 years or younger have been published (table 1). Based on these limited data which were collected using heterogeneous methodology (i.e. nocturnal PSG versus nocturnal polygraphy versus nap PSG), it is apparent that an oAHI >5 events·h−1 may be normal in the first month of life, while the same value corresponds to moderate-to-severe OSAS in children older than 2 years and necessitates treatment [2]. This finding reflects the progressive reduction in the frequency of upper airway obstructive events during sleep in the first 6 months of life. A similar trend is evident for central apnoeas (table 1).
TABLE 1.
Comparison of reference values of polysomnography (PSG), polygraphy and nocturnal oximetry respiratory parameters from recent studies that recruited healthy infants and used American Academy of Sleep Medicine scoring rules
| Study [ref.] (method) | Mean age | ||||
| <1 month | 1 month | 3 months | 5 months | 12 months | |
| Satomaa et al. (2016) [16] (nocturnal PSG) | |||||
| AHI, events·h−1 | 13.7 (0.5–81.7) | ||||
| oAHI, events·h−1 | 0 (0–0.3) | ||||
| ODI3, events·h−1 | 20.9 (0–79.5) | ||||
| Daftary et al. (2019) [17] (nocturnal PSG) | |||||
| AHI, events·h−1 | 14.5 (1–37.7) | ||||
| CAI, events·h−1 | 3.3 (0–27.2) | ||||
| Hypopnoea index, events·h−1 | 5.9 (0.7–12.9) | ||||
| Mean SpO2, % | 98.2 (95.5–99.7) | ||||
| ODI3, events·h−1 | 16.6 (0.5–41) | ||||
| Kanack et al. (2022) [18] (nap PSG) | |||||
| AHI, events·h−1 | 6.9 (2–23) | ||||
| oAHI, events·h−1 | 4.9 (1.7–19.1) | ||||
| CAI, events·h−1 | 0.7 (0.0–12.4) | ||||
| Stefanovski et al. (2022) [21] (nocturnal PSG) | |||||
| AHI, events·h−1 | 16.9 | 4.1 | |||
| oAHI, events·h−1 | 10.2 | 1.9 | |||
| CAI, events·h−1 | 6.6 | 2.2 | |||
| OHI, events·h−1 | 5.4 | 1.3 | |||
| Mean SpO2, % | 97.9 | 98.6 | |||
| Brockmann et al. (2013) [28] (nocturnal polygraphy) | |||||
| AHI, events·h−1 | 7.8 (95th percentile 25.5) |
4.9 (95th percentile 26.4) |
|||
| oAHI, events·h−1 | 1.5 (95th percentile 5.8) |
0.9 (95th percentile 3.4) |
|||
| CAI, events·h−1 | 5.5 (95th percentile 20.5) |
4.1 (95th percentile 24.2) |
|||
| ODI3, events·h−1 | 8.2 (95th percentile 24.9) |
7.5 (95th percentile 24) |
|||
| Evans et al. (2018) [19] (nocturnal oximetry) | |||||
| Mean SpO2, % | 97.05 | 97.65# | |||
| ODI3, events·h−1 | 25.4 | 13.9 | |||
|
Vezina
et al. (2020) [20]
(nocturnal polygraphy) | |||||
| AHI¶, events·h−1 | 4.2 (90th percentile 10.7) |
||||
| CAI, events·h−1 | 2.5 (90th percentile 7.1) |
||||
| OAI, events·h−1 | 0 (90th percentile 0.5) |
||||
| Median SpO2, % | 97.1 (10th percentile 95.5) |
||||
| ODI3, events·h−1 | 6.7 (90th percentile 15.8) |
||||
Data are presented as median (range), mean or median (95th, 90th or 10th percentile). AHI: apnoea–hypopnoea index; oAHI: obstructive apnoea–hypopnoea index (obstructive and mixed apnoeas and obstructive hypopnoeas per hour of total sleep time); ODI3: oxygen desaturation (≥3%) index; CAI: central apnoea index; SpO2: arterial oxygen saturation measured by pulse oximetry; OHI: obstructive hypopnoea index; OAI: obstructive and mixed apnoeas index. #: 3–4 months; ¶: hypopnoeas were scored with at least 50% drop in the amplitude of the airflow signal.
Although the study by Brockmann et al. [28] was published in 2013, it has been included in table 1 because it provides reference values for polygraphy parameters in 1- and 3-month-old infants. Additionally, hypopnoeas in the specific study were defined as a reduction in nasal flow by ≥30% relative to the pre-event baseline with a corresponding decrease in arterial oxygen saturation measured by pulse oximetry (SpO2) by ≥3% or an arousal, a definition that is consistent with the current AASM Manual scoring criteria [29]. Of note, scoring of arousals was not based on encephalogram or submental electromyogram recordings. Reference values for PSG parameters in the second year of life have been presented in a study by Scholle et al. [3] that has two methodological limitations: 1) only 22 subjects aged 1.1–1.9 years were studied and 2) hypopnoeas were scored if there was a ≥50% fall in the amplitude of the nasal pressure signal compared with the pre-event baseline (2007 AASM Manual) [31]. The 90th percentiles for the AHI and CAI were 4.3 and 2.1 events·h−1, respectively, and there were no hypopnoeas. Nevertheless, these values are not directly comparable with PSG results obtained using scoring criteria from the most recent version of the AASM Manual [29].
Decline of obstructive and central events in the first year of life in infants with upper airway obstruction
The declining frequency of obstructive events during sleep in infancy has been confirmed by a retrospective cohort of 38 subjects without craniofacial or upper airway anomalies or genetic syndromes who had serial PSGs at median ages of 4 and 11 weeks [23]. An interesting speculation by the authors of the study is that at least some of the obstructive events recorded by PSG may be due to nasal obstruction induced by the nasal airflow prongs that were introduced into the narrow infant nostrils [23].
Moreover, the frequency of obstructive events may decline with age even in infants with comorbidities. In another retrospective cohort study, 26 children younger than 3 years (median age 7.2 months) who were diagnosed with mild OSAS (oAHI 1–5 events·h−1) and did not receive any treatment had at least two PSGs performed 3–12 months apart [24]. Comorbidities included trisomy 21, cardiac disease, reactive airway disease/asthma, hypertension and prematurity [24]. In follow-up PSG, the oAHI decreased significantly from 2.7 to 1.3 events·h−1; OSAS resolved in eight children (30.8%) and deteriorated in only one (3.8%).
Similarly, a retrospective analysis of data from 13 infants with central AHI ≥5 events·h−1 diagnosed at 0.6–1.6 months of life who had a history of apnoeas and oxygen desaturations requiring admission or evaluation but without any confirmed underlying disease demonstrated that at a median age of 12.4 months, the central AHI decreased from 26.1 to 4.2 events·h−1 [25].
In summary, a limited number of retrospective studies revealed that obstructive and central sleep apnoeas decline in frequency during infancy not only in otherwise healthy children but also in those with symptoms and signs of upper airway obstruction or clinically apparent apnoeas.
Challenges in the diagnosis, severity classification and treatment indications of OSAS
Given that obstructive and central sleep apnoeas or hypopnoeas decline in frequency with age in both otherwise healthy infants and in infants with upper airway obstruction, cut-off values of PSG respiratory parameters for OSAS definition and severity classification represent a “moving target” with implications for treatment recommendations. In a study of 296 infants younger than 1 year who underwent PSG due to noisy breathing, witnessed apnoeic events and/or desaturations, an inverse relationship of both the oAHI and CAI with increasing age was demonstrated [32]. This reduction reflects the decreasing number of obstructive and central respiratory events during sleep in the growing infant. If this age effect is not taken into consideration and criteria similar to those for older children are used (i.e. oAHI ≤1 events·h−1 for primary snoring, oAHI 1–5 events·h−1 for mild OSAS and oAHI >5 events·h−1 for moderate-to-severe OSAS), an increased proportion of children aged 2 years or younger will be offered treatment for SDB [2].
Laryngomalacia represents an interesting example for how clinical impression and PSG interpretation using criteria for older children may lead to conflicting severity classification of upper airway obstruction. Based on international consensus clinical criteria, laryngomalacia can be classified as mild, moderate or severe [33]. Verkest et al. [34] reviewed data of 44 children aged 6.3–29.8 months with laryngomalacia who were evaluated with PSG. Using clinical criteria and endoscopic findings, 39% of subjects were classified as mild, 43% as moderate and 18% as severe laryngomalacia. After considering results of PSG, 20% and 5% of patients from the mild severity level were re-classified to the moderate and severe level, respectively, whereas 30% were moved from the moderate severity level to the severe level.
Ratanakorn et al. [26] analysed data of 102 infants with laryngomalacia, 57 (56%) of whom had OSAS alone (oAHI >1 events·h−1) and 45 (44%) had both OSAS and central sleep apnoea (CAI >5 events·h−1). Initial PSG was completed within the first 6 months of life and it was repeated every 3–6 months until infants achieved both oAHI and CAI <5 events·h−1. Those who were treated with supraglottoplasty relative to subjects who did not undergo supraglottoplasty had a similar oAHI during the first 6 months of life (baseline) and achieved OSAS resolution at a similar age (oAHI <1 event·h−1 at 35.2 months of age for the supraglottoplasty group versus 41.5 months for the nonsurgically treated group; p=0.60). oAHI decreased significantly at 6–12 months of age in the supraglottoplasty group but not in the nonsurgically treated group. Thus, obstructive events decreased in frequency earlier in infants who underwent supraglottoplasty, but they ultimately resolved with age regardless of whether surgical treatment was offered or not.
The discrepancy between the severity classifications of upper airway obstruction based on clinical criteria compared with PSG results is most apparent among patients 6 months of age or younger. DeHaan et al. [35] presented a large cohort of 233 subjects with symptoms and signs of upper airway obstruction of various aetiologies who underwent PSG at ages younger than 6 months (31%), 6–12 months (23%) or 12–24 months (46%). A higher proportion of participants evaluated at an age younger than 6 months were classified as having severe upper airway obstruction based on PSG criteria (AHI >10 events·h−1) than using clinical criteria (82.4% versus 20.4%, respectively). This discrepancy was much less apparent when children aged 12–24 months were considered (34.6% in the severe category based on PSG criteria versus 20.9% using clinical criteria).
Recently published British Thoracic Society guidelines for diagnosing and monitoring paediatric SDB suggested the use of PSG or polygraphy for diagnosis of SDB in children younger than 2 years of age but also emphasised that AHI values are not validated for intervention in this group [36].
In summary, taking into consideration that the frequency of obstructive and central sleep apnoea/hypopnoea events decreases during infancy in both healthy subjects and patients with upper airway obstruction, there is an urgent need to develop and use age-adjusted reference values for respiratory PSG parameters when diagnosing OSAS and classifying its severity in subjects younger than 2 years.
Pattern of upper airway obstruction in young children
The mechanisms and pattern of upper airway obstruction in infants and young children may differ from those in children older than 2 years of age in whom adenotonsillar hypertrophy is the major cause of upper airway obstruction. Especially in neonates, differences in upper airway anatomy such as a superiorly positioned larynx, a relatively large tongue and large occiput, in combination with craniofacial abnormalities or muscle hypotonia, may all contribute to the pathogenesis of OSAS [37]. An increased prevalence of dynamic abnormalities such as laryngomalacia and pharyngeal wall collapse has been reported in children below the age of 1 year and these conditions persist later in children with abnormal muscle tone [38]. On the other hand, the prevalence of fixed upper airway abnormalities like adenotonsillar hypertrophy increases in the first 2 years of life in children with OSAS and normal muscle tone [38]. The combination of dynamic and fixed upper airway obstruction, which is commonly observed in this age group, may pose a challenge for treatment. A fixed obstruction may result in increased negative inspiratory pressures causing an inspiratory collapse of more compliant supraglottic tissue resulting in laryngomalacia. In this scenario, removal of the fixed obstruction may also improve the dynamic collapse and surgical treatment may not be necessary [39, 40].
In a large retrospective study including more than 413 children under 3 years of age undergoing PSG at a large tertiary care centre, <35% of children below the age of 1 year presented with enlarged tonsils [41]. Herzig et al. [42] investigated the effect of age on the pattern of upper airway collapse during DISE in surgically naïve nonsyndromic children at risk for persistent OSAS and concluded that the youngest age group (2–5 years) had the highest prevalence of multilevel obstruction (59%). All these data support the notion that dynamic factors such as upper airway muscle hypotonia, laryngomalacia and multilevel upper airway obstruction due to craniofacial malformations or syndromic conditions are more commonly involved at a younger age [38]. Hence, insight into the pattern of upper airway obstruction might be helpful in treatment selection and should be included in shared decision making for these patients.
DISE as a tool for upper airway evaluation in infants and young children
DISE refers to a flexible upper airway endoscopy performed during a sedative state. It allows for a dynamic and three-dimensional evaluation of the entire upper airway. Readily available to most paediatric ear, nose and throat (ENT) surgeons, DISE is nowadays the most used tool to identify the site(s) of upper airway obstruction in children with OSAS [43]. Several aspects concerning paediatric DISE were recently addressed in an Expert Consensus statement published by the American Academy of Otorhinolaryngology–Head and Neck Surgery (AAO-HNS) [43]. Although there is no consensus regarding the optimal sedation for DISE, propofol and dexmetomidine have been identified as the most optimal agents for DISE in children. It is recommended to use inhalational anaesthesia only during the induction and to obtain intravenous access, but its use should be discontinued prior to the diagnostic part of the procedure. In addition, guidance for standardised scoring of paediatric DISE was recently published by Parikh et al. [44]. If performed in appropriate conditions with paediatric anaesthesia and ENT teams, DISE is considered a safe and well-tolerated procedure. Potential complications that may occur are laryngospasm and bronchospasm, oversedation, hypotension, bradycardia and respiratory depression, but there is no contraindication for DISE provided the child is considered fit to undergo anaesthesia [45].
DISE should be considered in children at risk for persistent OSAS such as those with severe disease (oAHI >10 events·h−1), small tonsils, Down syndrome, craniofacial anomalies and/or neuromuscular disorders [43]. Although these criteria would be often applicable to infants and young children with OSAS, DISE is not yet routinely performed in this age group. Despite the increased risk for multilevel obstruction, only 69% of experts on paediatric OSAS agreed or partially agreed that DISE should be performed before adenotonsillectomy in children less than 2 years of age [46], an observation which may, at least partially, be related to the lack of publications on DISE-directed treatment outcome in infants and young children.
Only a few reports specifically addressed the role of DISE in young children. Boudewyns et al. [47] performed DISE in 28 surgically naïve but otherwise healthy and nonobese children aged 1.5 years (range 1.3–1.8 years) with severe OSAS. DISE-directed treatment resulted in a significant improvement of OSAS and 71.4% had a post-operative oAHI <2 events·h−1. In the article, circumferential upper airway narrowing was associated with a less favourable outcome. In a second article by Boudewyns et al. [40], DISE was performed in 34 surgically naïve children without comorbidities that could affect upper airway anatomy or function. Interestingly, DISE altered treatment decision making in 35% and these infants did not routinely undergo adenotonsillectomy.
Love et al. [39] performed a retrospective analysis of DISE-directed treatment outcome in 79 surgically naïve children less than 2 years of age. The study population was divided in two groups: 38 children with and 41 children without laryngomalacia. Among the children without laryngomalacia, adenotonsillectomy was performed in 52.6% and adenoidectomy in 84.2%, respectively, and resulted in significant improvement in OSAS severity. Supraglottoplasty was the most commonly performed procedure (92.3%) in children with laryngomalacia, either as a single procedure (56.1%) or in conjunction with adenoidectomy (46.2%) or tonsillectomy (26.3%). Post-treatment PSG was available for 22 patients with laryngomalacia and showed a significant improvement in OSAS severity with a 78% reduction in AHI. The authors emphasised that DISE resulted in a deviation from standard treatment by adenotonsillectomy in 56% of the children presenting with OSAS and laryngomalacia [39].
He et al. [48] reported the outcome of DISE-directed surgery in 21 infants and 35 children with OSAS without tonsillar hypertrophy. The authors observed significant improvements in oAHI and oxygen saturation nadir. Infants were more likely to have an improvement in oAHI after surgery and more likely to undergo supraglottoplasty compared with older children.
Although DISE is a widely accepted diagnostic tool in children, there are still large variations in clinical practice, such as indications, anaesthetic protocol and grading system [43]. Moreover, it is yet unknown whether the upper airway of young children behaves differently under general anaesthesia and most studies on anaesthetic protocols for DISE were developed in children older than 2 years of age.
In many centres, DISE is performed at the start of the anaesthetic procedure and if a surgical target is identified, the child will then be intubated and treated accordingly. This requires a pre-operative discussion about the possible surgical interventions but is often preferred by parents to avoid multiple general anaesthetics.
Studies using DISE in young children demonstrated a different pattern of upper airway obstruction in infants and young children, with multilevel obstruction, dynamic collapse of upper airway tissues and hypotonia being commonly observed. Despite limited evidence, we suggest that DISE may be useful in selecting the most appropriate surgical intervention in these young children, thus avoiding unnecessary surgery and its complications while ensuring a favourable treatment outcome.
Progress in nonsurgical and surgical interventions for the management of upper airway obstruction in young children
Nasopharyngeal airway
A nasopharyngeal airway (NPA) is a short-length flexible tube which is passed through the nose and behind the tongue and positioned at the top of the larynx. It creates a patent airway by eliminating the obstruction due to the glossoptosis and has been most commonly used in children with Pierre Robin Sequence (PRS) [49]. An NPA is considered as a bridging treatment while awaiting mandibular growth. Successful resolution of obstruction with NPA in PRS varies between studies from 67% to 100% [50]. Hicks et al. [51] reported a retrospective review of upper airway management in PRS and suggested an algorithm using baseline and titration PSG. NPA was used as first-line management for children with moderate-to-severe OSAS (AHI >5 events·h−1); 10 of the 20 patients treated with NPA and noninvasive support (supplemental oxygen and appropriate positioning) showed improvement post-NPA insertion.
Alencar et al. [52] divided children with PRS into two groups according to the type of treatment in early infancy: 38 were treated with NPA (more severe cases) and 24 with postural treatment (less severe cases). All children were evaluated at 2–6 years of age using the Denver II Developmental Screening Test and Neurological Evolutionary Examination. According to Denver II, 73.7% children in the NPA group and 79.2% in the postural group showed normal development. Considering all areas of development, there were no significant differences between the NPA and postural groups, suggesting that treatment of severe upper airway obstruction with NPA supports neurodevelopment in children with PRS.
Although there is no consensus for the duration of NPA use, studies report 2–8 months [50]. Complications associated with the use of NPA include worsening of gastro-oesophageal reflux, intranasal stenosis and blockage of the NPA with secretions [50]. NPA treatment may not be widely available in all settings as parental education and support by a medical team are essential for long-term treatment with NPA at home and this setup may not be available in all specialised centres.
Continuous PAP therapy and noninvasive PAP
Continuous PAP (CPAP) therapy involves the application of a constant positive pressure to the upper and lower airway, whereas noninvasive positive pressure ventilation (NPPV) therapy delivers bilevel PAP, i.e. inspiratory PAP and expiratory PAP [53, 54]. In short, CPAP therapy is mainly used to stent the upper airway in children of OSAS. In children with OSAS accompanied with hypoventilation or for children with primarily hypoventilation, NPPV is the appropriate treatment.
The 2017 ERS statement on the diagnosis and management of OSAS in 1- to 23-month-old children recommended CPAP therapy for infants with moderate-to-severe OSAS who are not candidates for, or do not improve after, upper airway surgery [1]. The 2022 ERS statement on paediatric long-term noninvasive ventilation also favours the use of CPAP above invasive ventilation as long-term CPAP provides benefit across numerous anatomical and functional factors predisposing infants to upper airway obstruction with less risk than invasive ventilation [55]. This, in addition to the high rate of resolution of underlying upper airway obstruction, even in infants with long-term risk factors, supports the consideration of a trial of long-term CPAP/NPPV before considering a tracheostomy in infants with upper airway obstruction [56].
CPAP is, in general, started at pressures of 4–6 cmH2O and titrated up to 10 cmH2O, and is an effective and well-tolerated treatment. The data on the use of long-term CPAP/NPPV in infants stem mostly from relatively small, single-centre, retrospective studies, with some prospective registries [57, 58]. A more recent study by Cielo et al. [59] compared 41 infants and 109 school-aged children with OSA and CPAP treatment. After CPAP titration, oAHI was reduced by a median of 92% in infants. CPAP was used in infants on 95% of nights, which was significantly higher than the use in older children (83%). In both groups, behavioural issues were the most commonly identified barriers for successful CPAP therapy [59]. Because of the longer sleep need in infants, it is advised to maximise adherence, namely to aim for CPAP use during each and the entire night-time sleep [60].
CPAP can also be applied as a temporary intervention in infants with PRS awaiting craniofacial surgery to allow for further growth and maturation of the upper airway. The study by Cielo et al. [59] reported a successful weaning rate of 56%. This is a relatively unique feature for OSAS in infants; however, there are no data on the optimal timing to assess clinical improvement, which is largely based on individual experience and asks for a personalised treatment approach. It is recommended to plan a close follow-up as there are also other particularities in this population, such as interface side-effects, need for specific equipment and regular interface assessment. Most studies report only minor interface-related complications with therapy. High occurrence of facial flattening has also been described, but the long-term consequences and potential reversibility of this finding are unknown. The most common interface for administering CPAP or NPPV is a nasal mask; an oronasal mask is used in cases of uncontrollable mouth leak or severe nasal obstruction. Availability of appropriate masks for young children may vary in different countries and maybe a limiting factor for PAP use.
High-flow nasal cannula
HFNC therapy generates PAP through the delivery of humidified air or air/oxygen mixtures at high flow rates through a nasal cannula (an open interface) that is more comfortable than nasal masks used for PAP therapy. During HFNC therapy, gas is supplied at a constant flow rate, which does not adjust to maintain a certain pressure and pressure is not monitored. HFNC is effective in improving the oAHI in children with OSAS in the sleep laboratory [61–64]. A meta-analysis concluded that although limited numbers of heterogeneous and uncontrolled titration studies indicated that HFNC improves oAHI and oxygen saturation in children with OSAS, further research is needed on long-term efficacy and compliance with a focus on different age groups [65].
15 infants with OSAS who underwent HFNC titration PSG were evaluated retrospectively [66]. Although HFNC significantly improved oAHI and SpO2 nadir, five failed to respond to HFNC, which was defined as addition of oxygen. All patients had reported good adherence for at least 3 months while six used HFNC therapy for more than 6 months at home [66].
22 children (average age 12.8 months) with moderate-to-severe OSAS were retrospectively evaluated to determine the efficacy of HFNC treatment in the sleep laboratory and at home [67]. 59% of these young children had genetic disorders, including Down syndrome; 32% had a history of premature birth and 14% had chronic lung disease. 36% had persistent OSAS following upper airway surgery. The use of HFNC during the titration study was associated with improvements in oAHI, oxygenation and ventilation. Although the average CAI did not change during HFNC titration, there was an increase in CAI among five patients with chronic medical conditions. 50% of the patients needed supplemental oxygen; most had diagnoses that increased their risk for nocturnal hypoxaemia. 19 patients were prescribed home HFNC for OSAS treatment and reported adherence was measured at 6 and 12 months. At 6 and 12 months, 75% and 58% continued treatment, respectively. OSAS resolved in some children over the 12-month period [67].
HFNC may be an option in young children with persistent moderate-to-severe OSAS following surgical therapy or as a bridge until definitive therapy. Although one study suggested that subjective adherence to HFNC may be similar to CPAP adherence in older children, adherence to HFNC cannot be objectively monitored as CPAP machines and home treatment should be closely monitored if CPAP-intolerant children are discharged home on HFNC [68]. As CAI may increase, performing a titration study for treatment-emergent central apnoea is recommended [67]. Although the precise reasons for this are unclear, suggested mechanisms include lowering of carbon dioxide levels below the apnoea threshold, stimulation of the Hering–Breuer inflation reflex and overstimulation of airflow-sensitive receptors in the upper airway [69]. Of note, as HFNC affects airflow signals in the sleep laboratory, assessment of apnoeas and hypopnoeas may be challenging depending on the setup.
There is a potential additional effect of improved ventilation with HFNC that is distinct from providing PAP [70]. Washout of the nasopharyngeal dead space with HFNC may lead to reduced rebreathing of expired air compared with the added dead space of the CPAP mask [70]. Another potential advantage is prevention of midface hypoplasia associated with PAP therapy. A HFNC interface with a modified circuit connected to a standard ventilator to provide CPAP therapy has been reported in case series of infants and children who are CPAP intolerant [71].
HFNC is a novel therapy and can be considered for long-term therapy only if other therapy options fail to treat OSAS or in PAP-intolerant young children. Also, prospective, multicentre studies with long-term data for home use as well as home units with alarms and adherence data are needed before HFNC can be recommended for wide use in infants and young children with OSAS. There are also additional financial barriers to this therapy as it is a high-cost treatment in settings where it is not covered by the health insurance systems.
Other nonsurgical therapies
As the treatment of young children with OSAS is challenging, Brockbank et al. [72] studied the effect of supplemental oxygen on sleep and respiratory events in infants with OSAS. There was a significant reduction in obstructive events with oxygen treatment, but as expected it did not normalise oAHI. Respiratory event-related oxygen desaturations and oxygenation improved, and although obstructive apnoeas were slightly longer there was no significant adverse effect of supplemental oxygen on alveolar ventilation. Supplemental oxygen may be considered as an alternative treatment for infants who are not good candidates for CPAP or surgery, but these patients need to be watchfully followed as there are only limited data and no long-term follow-up data evaluating clinical outcomes for this therapy.
Although there are limited data regarding the efficacy and safety of positional therapy for infants with OSAS, prone positioning during sleep is recommended for infants with PRS as a conservative treatment option. Changes in PSG parameters for prone versus nonprone body positions in 11 infants were analysed by Hong et al. [73]. Although 82% of the infants had a decrease in oAHI, supporting the theory that gravity favours anterior tongue and jaw position and partially relieves the upper airway obstruction from glossoptosis, there was no resolution of OSAS in any of the participants in the prone position. Notably, one infant had worsening of OSAS, suggesting that this therapy should be objectively evaluated in individual infants. It should be noted that prone sleep positioning is not generally recommended for infants due to increased risk of sudden infant death syndrome.
Adenoidectomy and tonsillectomy
Surgical removal of the adenoids and tonsils is recommended by the American Academy of Paediatrics and AAO-HNS as an effective treatment for paediatric OSAS with success rates of 60–80% [74–78]. However, these guidelines are generally limited to children aged 2 years or older. Nonetheless, accumulating evidence indicates that adenotonsillectomy can lead to significant improvements in sleep-related quality of life and OSAS in young children [79–81].
In a recent cohort study of 87 children aged under 3 years, adenotonsillectomy effectively improved OSAS severity in the majority of children, but 78% of the patients had a post-operative AHI ≥1 events·h−1 and 8% an AHI ≥10 events·h−1 [82]. A possible explanation for this high rate of persistent OSAS is the fact that young children often have coincident upper airway abnormalities [83]. This was highlighted by the research of Argyriou et al. [84] who performed microlaryngoscopy and bronchoscopy in 158 selected children (median age 3 years) scheduled to undergo adenotonsillectomy for OSAS. More than half of patients had an airway abnormality, such as laryngomalacia (36%) or subglottic stenosis (17%), and these findings were most common in children aged 1–3 years. In addition, 32% of patients had signs of gastro-oesophageal reflux, which may worsen upper airway oedema.
Intracapsular tonsillectomy is a technique that involves removing the obstructing tonsillar tissue while leaving the tonsil capsule undisturbed. It may offer certain benefits over total tonsillectomy, particularly for the length of recovery and bleeding rates [85]. The drawback of intracapsular techniques is the risk of tonsillar regrowth and consequent recurrence of symptoms, which occurs in up to 10% of patients [86]. In a Swedish retrospective chart review of 28 000 children, young age at first surgery was associated with an increased need for revision surgery [87]. Similarly, in an English cohort study of 1300 children treated with intracapsular tonsillectomy, age under 2 years at the time of the surgery and severe OSAS were identified as independent risk factors for revision surgery [88].
Adenoidectomy is often considered as a single procedure in infants and young toddlers given the substantial morbidity associated with tonsillectomy in this age group. According to a national Swedish registry, adenoidectomy is commonly performed in children under 2 years, while adenotonsillectomy is the predominant procedure in older children [89]. A systematic review and meta-analysis by Reckley et al. [90] assessed the PSG outcomes of adenoidectomy for OSAS and concluded that adenoidectomy alone can alleviate OSAS, with an overall improvement in AHI from 18.1 to 3.1 events·h−1. Children under 12 months benefitted the most. Since the Reckley et al. [90] meta-analysis, three studies have been published on the efficacy of isolated adenoidectomy for OSAS [91–93]. The need for revision or additional surgery ranged from 18% to 34%, with risk factors being young age at the time of surgery, tonsillar size and gastro-oesophageal reflux [91–93].
Although relatively safe, adenotonsillectomy is not without risks and may result in complications which range from major events such as post-operative pulmonary oedema, haemorrhage and upper airway obstruction to minor events such as transient hypoxaemia or poor oral intake. Based on the recognition that peri-operative adverse events are more frequent in young children, the AAO-HNS recommended in their 2019 guideline that children under 3 years of age should be managed as inpatients following tonsillectomy [75, 94–97]. Gehrke et al. [98] retrospectively studied a large cohort of children and found that young age (under 3 years) was only associated with post-operative complications within the first 3 h after adenotonsillectomy or adenoidectomy. Castano et al. [99] evaluated the adenotonsillectomy complication rate in 188 children aged 3 years or younger. They observed post-operative complications in 18%, the majority of which suffered from poor oral intake. Two subjects developed post-operative pulmonary oedema and five had desaturations requiring supplemental oxygen. The authors concluded that adenotonsillectomy is safe in young children and challenged the notion that overnight hospitalisation is necessary in all children under 3 years. In another retrospective study, children under 2 years had a significantly higher post-operative complication rate (38% versus 22%), particularly due to respiratory distress, when compared with children 2–3 years old [100]. Finally, Billings et al. [101] correlated pre-operative PSG parameters with the risk of respiratory compromise following adenotonsillectomy. In their cohort of 195 children aged 3 years or younger, 18% with severe OSAS required supplemental oxygen as opposed to 6% with mild-to-moderate OSA.
Adenoidectomy is less invasive than adenotonsillectomy and therefore associated with less post-operative risks. In a recent retrospective chart review, 17% of young children who underwent adenoidectomy had a post-operative event, which mainly consisted of transient fever, and this risk was similar across all age groups [102]. Significant respiratory events, including oxygen desaturations, use of CPAP or NPA, were seen in 3% of patients. In a subgroup analysis of children under 18 months, younger age and higher baseline AHI were associated with the development of adverse events. Based on these results, the authors advocated that children aged 18 months or younger should be monitored in hospital following adenoidectomy. This statement is corroborated by a retrospective cohort study of Patel et al. [103] who reported that only seven out of 76 children under 2 years received post-operative inpatient care after adenoidectomy, with three of them requiring CPAP.
Five population-based studies recently investigated the morbidity of tonsillectomy [104–108]. In all of them, young age was significantly associated with an increased rate of respiratory complications [104–108]. Interestingly, however, in a large cohort of more than 500 000 children, young age was not identified as a predictive factor of post-operative mortality in multivariable analysis correcting for the presence of complex comorbidities [108].
In conclusion, adenotonsillectomy can effectively improve nocturnal breathing and quality of life in infants and young toddlers with OSAS. Similarly, adenoidectomy can be an efficacious surgical procedure, particularly in children under 12 months of age. However, it is important to note that persistent disease is not uncommon in this age group. Post-operatively, children under 2 years should be monitored in hospital due to the increased risk of respiratory complications. The efficacy and safety of adenoidectomy and tonsillectomy surgery in this age group calls for careful decision making based on accurate upper airway assessment and multidisciplinary discussion.
Supraglottoplasty
Laryngomalacia is a common cause of OSAS among infants and young children. Infants and young children with laryngomalacia and OSAS present earlier in life and have a poorer quality of life compared with surgically naïve young children with OSAS but without laryngomalacia [39]. Supraglottoplasty is considered the first-line surgical treatment for children with severe laryngomalacia [33]. In 2016, two meta-analyses on supraglottoplasty as a treatment modality for laryngomalacia and OSAS were published [109, 110].
Lee et al. [109] included seven studies in their meta-analysis on the outcome of supraglottoplasty as primary or secondary treatment for OSAS in children under 2 years of age. The success rate for an AHI <1 event·h−1 varied from 13% to 50% and the success rate for an AHI <5 events·h−1 from 67% to 86%. The authors did not find a difference in success rates between children with and without comorbidities. Farhood et al. [110] focused on the outcome of supraglottoplasty for congenital laryngomalacia and OSAS, and excluded cases with state-dependent or late-onset laryngomalacia. Five out of six studies reported by Farhood et al. [110] were also included in the meta-analysis by Lee et al. [109]. Farhood et al. [110] investigated the effect of age on success rate and found a significant improvement in AHI only in the younger age (<7 months) group. However, the number of patients included in each group was limited (n=10) and no formal conclusions could be drawn. Although children with more severe disease at baseline had greater improvement, the authors emphasised that most patients had residual disease in the mild to moderate range requiring further observation or multimodal treatment.
More recent studies investigated the effect of supraglottoplasty on OSAS severity in infants and young children. In the previously cited study by Love et al. [39], supraglottoplasty resulted in an improvement of AHI from 16.9±19.9 to 3.1±12.0 events·h−1. Bhushan et al. [111] reported on a historical cohort of 41 otherwise healthy patients treated with supraglottoplasty for laryngomalacia and severe OSAS. The authors found a significant improvement in post-treatment oAHI, number of arousals, percentage of REM sleep and sleep efficiency, but not in mean or nadir oxygen saturation during sleep [111]. Verkest et al. [34] reported pre- and post-operative PSG data for 17 patients with laryngomalacia and various comorbidities. Only 41% had a full recovery with a post-operative AHI <2 events·h−1; 36% had persistent mild disease and 24% had moderate OSAS. Patients with comorbidities were more likely to have persistent disease.
Cockerill et al. [112] reported the outcome of supraglottoplasty in 18 young children with Down syndrome. Pre- and post-operative PSG was performed in four patients, and all had a post-operative AHI ≤5 events·h−1, although one patient required revision supraglottoplasty to obtain this result. Nearly half (44%) of the patients in the study underwent subsequent adenotonsillectomy or tonsillectomy and the authors cautioned that supraglottoplasty should not be considered a panacea for OSAS in children with Down syndrome. However, the authors did not elaborate on how laryngomalacia was diagnosed in their study and whether DISE was used to identify the site(s) of upper airway obstruction.
In conclusion, laryngomalacia is the most common cause of OSAS in infants and young children, and is characterised by a dynamic collapse of supraglottic tissues. Supraglottoplasty is the preferred surgical technique for children with moderate-to-severe disease and results in a symptomatic improvement. Objective data obtained by PSG confirm an improvement in OSAS severity, although many patients have residual disease in the mild to moderate range requiring further observation or multimodal treatment [110].
Conclusions
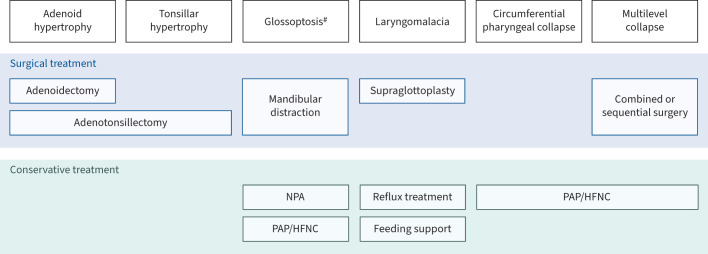
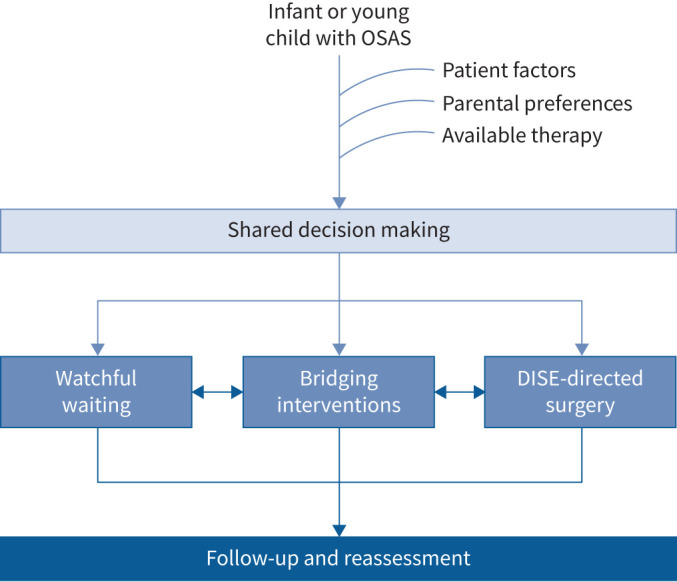
Since the publication of the 2017 ERS statement on the diagnosis and management of OSAS in children 1- to 23-months old [1], further evidence indicates that age-adjusted PSG definition and severity classification of SDB are necessary. DISE has an increasing role in decision making for surgical interventions, while nonsurgical options like PAP or HFNC can provide symptomatic relief in cases of dynamic upper airway collapse, during the waiting period for surgery or for persistent OSAS following surgery (figures 1 and 2).
FIGURE 1.
Approach to management of obstructive sleep apnoea syndrome (OSAS) in children under 2 years of age. DISE: drug-induced sleep endoscopy.
FIGURE 2.
Upper airway findings and treatment options for obstructive sleep apnoea syndrome in children under 2 years of age. #: commonly seen in children with Pierre Robin Sequence. NPA: nasopharyngeal airway; PAP: positive airway pressure; HFNC: high-flow nasal cannula.
Points for clinical practice
Reference values for PSG respiratory parameters, OSAS definition and severity classification in children 2 years of age or younger should probably differ from those applied in older children. In addition to AHI, the effect of additional parameters such as desaturation index, mean oxygen saturation and percentage time with hypoxia on clinical outcomes needs to be evaluated.
An oAHI >5 events·h−1 may be normal in the first month of life.
There are no clinical trials for OSAS treatment in infants, and outcomes such as growth and neurodevelopment have not been established for potential trials.
The combination of dynamic and fixed upper airway obstruction may pose a challenge for treatment, and DISE may be useful in selecting the most appropriate surgical intervention in these young children.
For patients who are not candidates for airway surgery, NPA insertion in PRS, CPAP or NPPV may decrease upper airway resistance and promote normal alveolar ventilation.
Adenotonsillectomy can effectively improve nocturnal breathing and quality of life in infants and young children with OSAS.
Laryngomalacia is a common cause of OSAS in this young age group and supraglottoplasty can provide symptomatic improvement for children with moderate-to-severe upper airway obstruction.
Questions for future research
Available reference values for respiratory PSG parameters are obtained from a very small number of studies, only a few of which are based on nocturnal PSG. There is an urgent need to develop and use age-adjusted reference values for respiratory PSG parameters when diagnosing OSAS and classifying its severity in subjects younger than 2 years.
Development of weaning protocols for infants on CPAP/NPPV in cases of expected improvement over time is needed.
Prospective studies evaluating the long-term efficacy and adherence of HFNC therapy in children <2 years of age will help to determine whether this will be a treatment alternative in CPAP-intolerant young children.
Future studies should evaluate the outcome of DISE-directed surgery in children according to the site of upper airway obstruction and comorbidities.
Footnotes
Provenance: Commissioned article, peer reviewed.
Number 1 in the Series “Sleep and Breathing Conference 2023” Edited by Maria R. Bonsignore, Dirk Pevernagie and Refika Ersu
Conflict of interest: None of the authors have any conflict of interest that is related to the content of this manuscript.
References
- 1.Kaditis AG, Alonso Alvarez ML, Boudewyns A, et al. . ERS statement on obstructive sleep disordered breathing in 1- to 23-month-old children. Eur Respir J 2017; 50: 1700985. doi: 10.1183/13993003.00985-2017 [DOI] [PubMed] [Google Scholar]
- 2.Kaditis A, Alonso Alvarez ML, Boudewyns A, et al. . Obstructive sleep disordered breathing in 2- to 18-year-old children: diagnosis and management. Eur Respir J 2016; 47: 69–94. doi: 10.1183/13993003.00385-2015 [DOI] [PubMed] [Google Scholar]
- 3.Scholle S, Wiater A, Scholle HC. Normative values of polysomnographic parameters in childhood and adolescence: cardiorespiratory parameters. Sleep Med 2011; 12: 988–996. doi: 10.1016/j.sleep.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 4.Judd RT, Mokhlesi B, Shogan A, et al. . Improvement in central sleep apnea following adenotonsillectomy in children. Laryngoscope 2022; 132: 478–484. doi: 10.1002/lary.29784 [DOI] [PubMed] [Google Scholar]
- 5.Hoppenbrouwers T, Hodgman JE, Harper RM, et al. . Polygraphic studies of normal infants during the first six months of life: III. Incidence of apnea and periodic breathing. Pediatrics 1977; 60: 418–425. doi: 10.1542/peds.60.4.418 [DOI] [PubMed] [Google Scholar]
- 6.Coons S, Guilleminault C. Development of consolidated sleep and wakeful periods in relation to the day/night cycle in infancy. Dev Med Child Neurol 1984; 26: 169–176. doi: 10.1111/j.1469-8749.1984.tb04428.x [DOI] [PubMed] [Google Scholar]
- 7.Scher MS. A developmental marker of central nervous system maturation: part I. Pediatr Neurol 1988; 4: 265–273. doi: 10.1016/0887-8994(88)90064-1 [DOI] [PubMed] [Google Scholar]
- 8.Lenehan SM, Fogarty L, O'Connor C, et al. . The architecture of early childhood sleep over the first two years. Matern Child Health J 2023; 27: 226–250. doi: 10.1007/s10995-022-03545-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hathorn MK. Analysis of periodic changes in ventilation in new-born infants. J Physiol 1978; 285: 85–99. doi: 10.1113/jphysiol.1978.sp012559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guthrie RD, Standaert TA, Hodson WA, et al. . Sleep and maturation of eucapnic ventilation and CO2 sensitivity in the premature primate. J Appl Physiol Respir Environ Exerc Physiol 1980; 48: 347–354. doi: 10.1152/jappl.1980.48.2.347 [DOI] [PubMed] [Google Scholar]
- 11.Henderson-Smart DJ, Read DJ. Reduced lung volume during behavioral active sleep in the newborn. J Appl Physiol Respir Environ Exerc Physiol 1979; 46: 1081–1085. doi: 10.1152/jappl.1979.46.6.1081 [DOI] [PubMed] [Google Scholar]
- 12.Gaultier C, Praud JP, Canet E, et al. . Paradoxical inward rib cage motion during rapid eye movement sleep in infants and young children. J Dev Physiol 1987; 9: 391–397. [PubMed] [Google Scholar]
- 13.Kaditis A, Gozal D. Sleep studies for clinical indications during the first year of life: infants are not small children. Children 2022; 9: 523. doi: 10.3390/children9040523 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kombathula R, Ingram DG, Ehsan Z. Current practice patterns in the diagnosis and management of sleep-disordered breathing in infants. J Clin Sleep Med 2019; 15: 1427–1431. doi: 10.5664/jcsm.7968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ng DK, Chan CH. A review of normal values of infant sleep polysomnography. Pediatr Neonatol 2013; 54: 82–87. doi: 10.1016/j.pedneo.2012.11.011 [DOI] [PubMed] [Google Scholar]
- 16.Satomaa AL, Saarenpaa-Heikkila O, Paavonen EJ, et al. . The adapted American Academy of Sleep Medicine sleep scoring criteria in one month old infants: a means to improve comparability? Clin Neurophysiol 2016; 127: 1410–1418. doi: 10.1016/j.clinph.2015.08.013 [DOI] [PubMed] [Google Scholar]
- 17.Daftary AS, Jalou HE, Shively L, et al. . Polysomnography reference values in healthy newborns. J Clin Sleep Med 2019; 15: 437–443. doi: 10.5664/jcsm.7670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanack MD, Nakra N, Ahmad I, et al. . Normal neonatal sleep defined: refining patient selection and interpreting sleep outcomes for mandibular distraction . Plast Reconstr Surg Glob Open 2022; 10: e4031. doi: 10.1097/GOX.0000000000004031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Evans HJ, Karunatilleke AS, Grantham-Hill S, et al. . A cohort study reporting normal oximetry values in healthy infants under 4 months of age using Masimo technology. Arch Dis Child 2018; 103: 868–872. doi: 10.1136/archdischild-2017-314361 [DOI] [PubMed] [Google Scholar]
- 20.Vezina K, Mariasine J, Young R, et al. . Cardiorespiratory monitoring data during sleep in healthy Canadian infants. Ann Am Thorac Soc 2020; 17: 1238–1246. doi: 10.1513/AnnalsATS.201909-703OC [DOI] [PubMed] [Google Scholar]
- 21.Stefanovski D, Tapia IE, Lioy J, et al. . Respiratory indices during sleep in healthy infants: a prospective longitudinal study and meta-analysis. Sleep Med 2022; 99: 49–57. doi: 10.1016/j.sleep.2022.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flint A, August D, Lai M, et al. . Determining reference data for overnight oximetry in neonates: a pilot study. Early Hum Dev 2022; 168: 105571. doi: 10.1016/j.earlhumdev.2022.105571 [DOI] [PubMed] [Google Scholar]
- 23.Kukkola HL, Kirjavainen T. Obstructive sleep apnea in young infants: sleep position dependence and spontaneous improvement. Pediatr Pulmonol 2023; 58: 794–803. doi: 10.1002/ppul.26255 [DOI] [PubMed] [Google Scholar]
- 24.Sarber KM, von Allmen DC, Tikhtman R, et al. . Polysomnographic outcomes after observation for mild obstructive sleep apnea in children younger than 3 years. Otolaryngol Head Neck Surg 2021; 164: 427–432. doi: 10.1177/0194599820954383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xiao L, Sunkonkit K, Chiang J, et al. . Unexplained significant central sleep apnea in infants: clinical presentation and outcomes. Sleep Breath 2023; 27: 255–264. doi: 10.1007/s11325-022-02612-3 [DOI] [PubMed] [Google Scholar]
- 26.Ratanakorn W, Brockbank J, Ishman S, et al. . The maturation changes of sleep-related respiratory abnormalities in infants with laryngomalacia. J Clin Sleep Med 2021; 17: 767–777. doi: 10.5664/jcsm.9046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ehsan Z, Kurian C, Weaver KN, et al. . Longitudinal sleep outcomes in neonates with Pierre Robin sequence treated conservatively. J Clin Sleep Med 2019; 15: 477–482. doi: 10.5664/jcsm.7680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brockmann PE, Poets A, Poets CF. Reference values for respiratory events in overnight polygraphy from infants aged 1 and 3 months. Sleep Med 2013; 14: 1323–1327. doi: 10.1016/j.sleep.2013.07.016 [DOI] [PubMed] [Google Scholar]
- 29.Berry RB, Quan SF, Abreu AR, et al. . The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 2.6. Darien, American Academy of Sleep Medicine, 2020. [Google Scholar]
- 30.Daftary AS, Shively L, Slaven JE, et al. . Can estimated time in airway obstruction be a useful measure for infant obstructive sleep apnea? Int J Pediatr Otorhinolaryngol 2019; 124: 208–209. doi: 10.1016/j.ijporl.2019.06.011 [DOI] [PubMed] [Google Scholar]
- 31.Iber C, Ancoli-Israel S, Chesson A, et al. . The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications. 1st Edn. Westchester, American Academy of Sleep Medicine, 2007. [Google Scholar]
- 32.Bandyopadhyay A, Slaven JE, Jackson SJ, et al. . Is obstructive apnea–hypopnea index associated with age in infants? Clin Pediatr 2023; 62: 1144–1149 doi: 10.1177/00099228231154134 [DOI] [PubMed] [Google Scholar]
- 33.Carter J, Rahbar R, Brigger M, et al. . International Pediatric ORL Group (IPOG) laryngomalacia consensus recommendations. Int J Pediatr Otorhinolaryngol 2016; 86: 256–261. doi: 10.1016/j.ijporl.2016.04.007 [DOI] [PubMed] [Google Scholar]
- 34.Verkest V, Verhulst S, Van Hoorenbeeck K, et al. . Prevalence of obstructive sleep apnea in children with laryngomalacia and value of polysomnography in treatment decisions. Int J Pediatr Otorhinolaryngol 2020; 137: 110255. doi: 10.1016/j.ijporl.2020.110255 [DOI] [PubMed] [Google Scholar]
- 35.DeHaan KL, Seton C, Fitzgerald DA, et al. . Polysomnography for the diagnosis of sleep disordered breathing in children under 2 years of age. Pediatr Pulmonol 2015; 50: 1346–1353. doi: 10.1002/ppul.23169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Evans HJ, Gibson NA, Bennett J, et al. . British Thoracic Society Guideline for diagnosing and monitoring paediatric sleep-disordered breathing. Thorax 2023; 78; 1043–1054. doi: 10.1136/thorax-2022-219582 [DOI] [PubMed] [Google Scholar]
- 37.Chandrasekar I, Tablizo MA, Witmans M, et al. . Obstructive sleep apnea in neonates. Children 2022; 9: 419. doi: 10.3390/children9030419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goldberg S, Shatz A, Picard E, et al. . Endoscopic findings in children with obstructive sleep apnea: effects of age and hypotonia. Pediatr Pulmonol 2005; 40: 205–210. doi: 10.1002/ppul.20230 [DOI] [PubMed] [Google Scholar]
- 39.Love H, Slaven JE, Mitchell RM, et al. . Outcomes of OSA in surgically naive young children with and without DISE identified laryngomalacia. Int J Pediatr Otorhinolaryngol 2020; 138: 110351. doi: 10.1016/j.ijporl.2020.110351 [DOI] [PubMed] [Google Scholar]
- 40.Boudewyns A, Saldien V, Van de Heyning P, et al. . Drug-induced sedation endoscopy in surgically naive infants and children with obstructive sleep apnea: impact on treatment decision and outcome. Sleep Breath 2018; 22: 503–510. doi: 10.1007/s11325-017-1581-7 [DOI] [PubMed] [Google Scholar]
- 41.Rayasam S, Johnson R, Lenahan D, et al. . Obstructive sleep apnea in children under 3 years of age. Laryngoscope 2021; 131: E2603–E2608. doi: 10.1002/lary.29536 [DOI] [PubMed] [Google Scholar]
- 42.Herzig MX, Hildebrand AD, Nguyen T, et al. . Drug-induced sleep endoscopy differences by age in surgically naive children with sleep-disordered breathing. JAMA Otolaryngol Head Neck Surg 2023; 149: 327–333. doi: 10.1001/jamaoto.2022.5187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Baldassari CM, Lam DJ, Ishman SL, et al. . Expert consensus statement: pediatric drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 2021; 165: 578–591. doi: 10.1177/0194599820985000 [DOI] [PubMed] [Google Scholar]
- 44.Parikh S, Boudewyns A, Friedman N, et al. . International Pediatric Otolaryngology Group (IPOG) consensus on scoring of pediatric drug induced sleep endoscopy (DISE). Int J Pediatr Otorhinolaryngol 2023; 171: 111627. doi: 10.1016/j.ijporl.2023.111627 [DOI] [PubMed] [Google Scholar]
- 45.Charakorn N, Kezirian EJ. Drug-induced sleep endoscopy. Otolaryngol Clin N Am 2016; 49: 1359–1372. doi: 10.1016/j.otc.2016.06.002 [DOI] [PubMed] [Google Scholar]
- 46.Benedek P, Balakrishnan K, Cunningham MJ, et al. . International Pediatric Otolaryngology Group (IPOG) consensus on the diagnosis and management of pediatric obstructive sleep apnea (OSA) . Int J Pediatr Otorhinolaryngol 2020; 138: 110276. doi: 10.1016/j.ijporl.2020.110276 [DOI] [PubMed] [Google Scholar]
- 47.Boudewyns A, Van de Heyning P, Verhulst S. Drug-induced sedation endoscopy in children <2 years with obstructive sleep apnea syndrome: upper airway findings and treatment outcomes. Eur Arch Otorhinolaryngol 2017; 274: 2319–2325. doi: 10.1007/s00405-017-4481-3 [DOI] [PubMed] [Google Scholar]
- 48.He S, Peddireddy NS, Smith DF, et al. . Outcomes of drug-induced sleep endoscopy-directed surgery for pediatric obstructive sleep apnea. Otolaryngol Head Neck Surg 2018; 158: 539–565. doi: 10.1177/0194599817740332 [DOI] [PubMed] [Google Scholar]
- 49.Zaballa K, Singh J, Waters K. The management of upper airway obstruction in Pierre Robin Sequence. Paediatr Respir Rev 2023; 45: 11–15. doi: 10.1016/j.prrv.2022.07.001 [DOI] [PubMed] [Google Scholar]
- 50.Abel F, Wallis C. The role of the nasopharyngeal prong in craniofacial disorders in particular the Pierre Robin sequence. Semin Fetal Neonatal Med 2021; 26: 10285. doi: 10.1016/j.siny.2021.101285 [DOI] [PubMed] [Google Scholar]
- 51.Hicks K, Billings KR, Purnell CA, et al. . An algorithm for airway management in patients with Pierre Robin sequence. J Craniofac Surg 2018; 29: 1187–1192. doi: 10.1097/SCS.0000000000004489 [DOI] [PubMed] [Google Scholar]
- 52.Alencar TRR, Marques IL, Bertucci A, et al. . Neurological development of children with isolated Robin sequence treated with nasopharyngeal intubation in early infancy. Cleft Palate Craniofac J 2017; 54: 256–261. doi: 10.1597/14-228 [DOI] [PubMed] [Google Scholar]
- 53.Kushida CA, Chediak A, Berry RB, et al. . Clinical guidelines for the manual titration of positive airway pressure in patients with obstructive sleep apnea. J Clin Sleep Med 2008; 4: 157–171. doi: 10.5664/jcsm.27133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Berry RB, Chediak A, Brown LK, et al. . Best clinical practices for the sleep center adjustment of noninvasive positive pressure ventilation (NPPV) in stable chronic alveolar hypoventilation syndromes. J Clin Sleep Med 2010; 6: 491–509. doi: 10.5664/jcsm.27941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Fauroux B, Abel F, Amaddeo A, et al. . ERS statement on paediatric long-term noninvasive respiratory support. Eur Respir J 2022; 59: 2101404. doi: 10.1183/13993003.01404-2021 [DOI] [PubMed] [Google Scholar]
- 56.Bedi PK, Castro-Codesal ML, Featherstone R, et al. . Long-term non-invasive ventilation in infants: a systematic review and meta-analysis. Front Pediatr 2018; 6: 13. doi: 10.3389/fped.2018.00013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leonardis RL, Robison JG, Otteson TD. Evaluating the management of obstructive sleep apnea in neonates and infants. JAMA Otolaryngol Head Neck Surg 2013; 139: 139–146. doi: 10.1001/jamaoto.2013.1331 [DOI] [PubMed] [Google Scholar]
- 58.Robison JG, Wilson C, Otteson TD, et al. . Analysis of outcomes in treatment of obstructive sleep apnea in infants. Laryngoscope 2013; 123: 2306–2314. doi: 10.1002/lary.23685 [DOI] [PubMed] [Google Scholar]
- 59.Cielo CM, Hernandez P, Ciampaglia AM, et al. . Positive airway pressure for the treatment of OSA in infants. Chest 2021; 159: 810–817. doi: 10.1016/j.chest.2020.08.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Amaddeo A, Griffon L, Fauroux B. Using continuous nasal airway pressure in infants with craniofacial malformations. Semin Fetal Neonatal Med 2021; 26: 101284. doi: 10.1016/j.siny.2021.101284 [DOI] [PubMed] [Google Scholar]
- 61.Amaddeo A, Khirani S, Frapin A, et al. . High flow nasal cannula for children not compliant with continuous positive airway pressure. Sleep Med 2019; 63: 24–28. doi: 10.1016/j.sleep.2019.05.012 [DOI] [PubMed] [Google Scholar]
- 62.Hawkins S, Huston S, Campbell K, et al. . High-flow, heated, humidified air via nasal cannula treats CPAP-intolerant children with obstructive sleep apnea. J Clin Sleep Med 2017; 13: 981–989. doi: 10.5664/jcsm.6700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Joseph L, Goldberg S, Shitrit M, et al. . High-flow nasal cannula therapy for obstructive sleep apnea in children. J Clin Sleep Med 2015; 11: 1007–1010. doi: 10.5664/jcsm.5014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fishman H, Al-Shamli N, Sunkonkit K, et al. . Heated humidified high flow nasal cannula therapy in children with obstructive sleep apnea: a randomized cross-over trial. Sleep Med 2023; 107: 81–88. doi: 10.1016/j.sleep.2023.04.017 [DOI] [PubMed] [Google Scholar]
- 65.Du F, Gu YH, He YC, et al. . High-flow nasal cannula therapy for pediatric obstructive sleep apnea: a systematic review and meta-analysis. Eur Rev Med Pharmacol Sci 2022; 26: 4583–4591. doi: 10.26355/eurrev_202207_29179 [DOI] [PubMed] [Google Scholar]
- 66.Kwok KL, Lau MY, Leung SY, et al. . Use of heated humidified high flow nasal cannula for obstructive sleep apnea in infants. Sleep Med 2020; 74: 332–337. doi: 10.1016/j.sleep.2020.08.005 [DOI] [PubMed] [Google Scholar]
- 67.Ignatiuk D, Schaer B, McGinley B. High flow nasal cannula treatment for obstructive sleep apnea in infants and young children. Pediatr Pulmonol 2020; 55: 2791–2798. doi: 10.1002/ppul.25009 [DOI] [PubMed] [Google Scholar]
- 68.Hawkins SM, Jensen EL, Simon SL, et al. . Correlates of pediatric CPAP adherence. J Clin Sleep Med 2016; 12: 879–884. doi: 10.5664/jcsm.5892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Narang I, Carberry JC, Eckert DJ. Central apnea and decreased drive to upper airway motoneurons during high flow nasal cannula therapy. Sleep Med 2020; 69: 98–99. doi: 10.1016/j.sleep.2020.01.017 [DOI] [PubMed] [Google Scholar]
- 70.Duong K, Noga M, MacLean JE, et al. . Comparison of airway pressures and expired gas washout for nasal high flow versus CPAP in child airway replicas. Respir Res 2021: 22: 289. doi: 10.1186/s12931-021-01880-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Overbergh C, Installe S, Boudewyns A, et al. . The Optiflow interface for chronic CPAP use in children. Sleep Med 2018; 44: 1–3. doi: 10.1016/j.sleep.2017.11.1133 [DOI] [PubMed] [Google Scholar]
- 72.Brockbank J, Astudillo CL, Che A, et al. . Supplemental oxygen for treatment of infants with obstructive sleep apnea. J Clin Sleep Med 2019; 15: 1115–1123. doi: 10.5664/jcsm.7802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Hong H, Wee CP, Haynes K, et al. . Evaluation of obstructive sleep apnea in prone versus nonprone body positioning with polysomnography in infants with Robin Sequence. Cleft Palate Craniofac J 2020; 57: 141–147. doi: 10.1177/1055665619867228 [DOI] [PubMed] [Google Scholar]
- 74.Marcus CL, Brooks LJ, Draper KA, et al. . Diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics 2012; 130: 576–584. doi: 10.1542/peds.2012-1671 [DOI] [PubMed] [Google Scholar]
- 75.Mitchell RB, Archer SM, Ishman SL, et al. . Clinical practice guideline: tonsillectomy in children (update). Otolaryngol Head Neck Surg 2019; 160: S1–S42. doi: 10.1177/0194599818814424 [DOI] [PubMed] [Google Scholar]
- 76.Marcus CL, Moore RH, Rosen CL, et al. . A randomized trial of adenotonsillectomy for childhood sleep apnea. N Engl J Med 2013; 368: 2366–2376. doi: 10.1056/NEJMoa1215881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Brietzke SE, Gallagher D. The effectiveness of tonsillectomy and adenoidectomy in the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: a meta-analysis. Otolaryngol Head Neck Surg 2006; 134: 979–984. doi: 10.1016/j.otohns.2006.02.033 [DOI] [PubMed] [Google Scholar]
- 78.Friedman M, Wilson M, Lin HC, et al. . Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg 2009; 140: 800–808. doi: 10.1016/j.otohns.2009.01.043 [DOI] [PubMed] [Google Scholar]
- 79.Mitchell RB, Kelly J. Outcome of adenotonsillectomy for obstructive sleep apnea in children under 3 years. Otolaryngol Head Neck Surg 2005; 132: 681–684. doi: 10.1016/j.otohns.2004.12.010 [DOI] [PubMed] [Google Scholar]
- 80.Brigance JS, Miyamoto RC, Schilt P, et al. . Surgical management of obstructive sleep apnea in infants and young toddlers. Otolaryngol Head Neck Surg 2009; 140: 912–916. doi: 10.1016/j.otohns.2009.01.034 [DOI] [PubMed] [Google Scholar]
- 81.Nath A, Emani J, Suskind DL, et al. . Predictors of persistent sleep apnea after surgery in children younger than 3 years. JAMA Otolaryngol Head Neck Surg 2013; 139: 1002–1008. doi: 10.1001/jamaoto.2013.4686 [DOI] [PubMed] [Google Scholar]
- 82.Rayasam SS, Abijay C, Johnson R, et al. . Outcomes of adenotonsillectomy for obstructive sleep apnea in children under 3 years of age. Ear Nose Throat J 2022; in press [ 10.1177/01455613221086526]. doi: 10.1177/01455613221086526 [DOI] [PubMed] [Google Scholar]
- 83.Rastatter JC, Schroeder JW Jr, French A, et al. . Synchronous airway lesions in children younger than age 3 years undergoing adenotonsillectomy. Otolaryngol Head Neck Surg 2011; 145: 309–313. doi: 10.1177/0194599811403071 [DOI] [PubMed] [Google Scholar]
- 84.Argyriou K, Yu B, Thevasagayam R. Evaluation of the role of microlaryngotracheobronchoscopy (MLTB) with adenotonsillectomy in 158 children with sleep-disordered breathing. Clin Otolaryngol 2021; 46: 1123–1126. doi: 10.1111/coa.13786 [DOI] [PubMed] [Google Scholar]
- 85.Parikh SR, Archer S, Ishman SL, et al. . Why is there no statement regarding partial intracapsular tonsillectomy (tonsillotomy) in the new guidelines? Otolaryngol Head Neck Surg 2019; 160: 213–214. doi: 10.1177/0194599818810507 [DOI] [PubMed] [Google Scholar]
- 86.Zhang LY, Zhong L, David M, et al. . Tonsillectomy or tonsillotomy? A systematic review for paediatric sleep-disordered breathing. Int J Pediatr Otorhinolaryngol 2017; 103: 41–50. doi: 10.1016/j.ijporl.2017.10.008 [DOI] [PubMed] [Google Scholar]
- 87.Odhagen E, Sunnergren O, Hemlin C, et al. . Risk of reoperation after tonsillotomy versus tonsillectomy: a population-based cohort study. Eur Arch Otorhinolaryngol 2016; 273: 3263–3268. doi: 10.1007/s00405-015-3871-7 [DOI] [PubMed] [Google Scholar]
- 88.Amin N, Bhargava E, Prentice JG, et al. . Coblation intracapsular tonsillectomy in children: a prospective study of 1257 consecutive cases with long-term follow-up. Clin Otolaryngol 2021; 46: 1184–1192. doi: 10.1111/coa.13790 [DOI] [PubMed] [Google Scholar]
- 89.Gerhardsson H, Stalfors J, Odhagen E, et al. . Pediatric adenoid surgery in Sweden 2004–2013: incidence, indications and concomitant surgical procedures. Int J Pediatr Otorhinolaryngol 2016; 87: 61–66. doi: 10.1016/j.ijporl.2016.05.020 [DOI] [PubMed] [Google Scholar]
- 90.Reckley LK, Song SA, Chang ET, et al. . Adenoidectomy can improve obstructive sleep apnoea in young children: systematic review and meta-analysis. J Laryngol Otol 2016; 130: 990–994. doi: 10.1017/S0022215116008938 [DOI] [PubMed] [Google Scholar]
- 91.Thadikonda KM, Shaffer AD, Stapleton AL. Outcomes of adenoidectomy-alone in patients less than 3-years old. Int J Pediatr Otorhinolaryngol 2018; 106: 46–49. doi: 10.1016/j.ijporl.2017.12.030 [DOI] [PubMed] [Google Scholar]
- 92.Stahl A, Dagan O, Nageris B, et al. . Outcomes and safety of adenoidectomy in infants up to 12 months of age compared to older children. Eur Arch Otorhinolaryngol 2020; 277: 2611–2617. doi: 10.1007/s00405-020-06047-y [DOI] [PubMed] [Google Scholar]
- 93.Chorney SR, Zur KB. Adenoidectomy without tonsillectomy for pediatric obstructive sleep apnea. Otolaryngol Head Neck Surg 2021; 164: 1100–1107. doi: 10.1177/0194599820955172 [DOI] [PubMed] [Google Scholar]
- 94.McColley SA, April MM, Carroll JL, et al. . Respiratory compromise after adenotonsillectomy in children with obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 1992; 118: 940–943. doi: 10.1001/archotol.1992.01880090056017 [DOI] [PubMed] [Google Scholar]
- 95.Rosen GM, Muckle RP, Mahowald MW, et al. . Postoperative respiratory compromise in children with obstructive sleep apnea syndrome: can it be anticipated? Pediatrics 1994; 93: 784–788. doi: 10.1542/peds.93.5.784 [DOI] [PubMed] [Google Scholar]
- 96.Statham MM, Elluru RG, Buncher R, et al. . Adenotonsillectomy for obstructive sleep apnea syndrome in young children: prevalence of pulmonary complications. Arch Otolaryngol Head Neck Surg 2006; 132: 476–480. doi: 10.1001/archotol.132.5.476 [DOI] [PubMed] [Google Scholar]
- 97.Lawlor CM, Riley CA, Carter JM, et al. . Association between age and weight as risk factors for complication after tonsillectomy in healthy children. JAMA Otolaryngol Head Neck Surg 2018; 144: 399–405. doi: 10.1001/jamaoto.2017.3431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Gehrke T, Scherzad A, Hagen R, et al. . Risk factors for children requiring adenotonsillectomy and their impact on postoperative complications: a retrospective analysis of 2000 patients. Anaesthesia 2019; 74: 1572–1579. doi: 10.1111/anae.14844 [DOI] [PubMed] [Google Scholar]
- 99.Castano JE, Freiser ME, Ramadan HH. Complications following inpatient extracapsular tonsillectomy in children 36 months and younger. JAMA Otolaryngol Head Neck Surg 2016; 142: 270–273. doi: 10.1001/jamaoto.2015.3562 [DOI] [PubMed] [Google Scholar]
- 100.Cooper F, Spektor Z, Kay DJ. Rate and risk factors for post-adenotonsillectomy complications in children under 24 months and 24 to 36 months old. Am J Otolaryngol 2020; 41: 102546. doi: 10.1016/j.amjoto.2020.102546 [DOI] [PubMed] [Google Scholar]
- 101.Billings KR, Somani SN, Lavin J, et al. . Polysomnography variables associated with postoperative respiratory issues in children <3 years of age undergoing adenotonsillectomy for obstructive sleep apnea. Int J Pediatr Otorhinolaryngol 2020; 137: 110215. doi: 10.1016/j.ijporl.2020.110215 [DOI] [PubMed] [Google Scholar]
- 102.Chorney SR, Dailey JF, Zur KB. Pediatric adenoidectomy in the very young child and indications for postoperative inpatient admission. Int J Pediatr Otorhinolaryngol 2020; 130: 109796. doi: 10.1016/j.ijporl.2019.109796 [DOI] [PubMed] [Google Scholar]
- 103.Patel R, Patel NA, Stoffels G, et al. . Adenoidectomy: inpatient criteria study. Am J Otolaryngol 2021; 42: 102765. doi: 10.1016/j.amjoto.2020.102765 [DOI] [PubMed] [Google Scholar]
- 104.Murto KTT, Katz SL, McIsaac DI, et al. . Pediatric tonsillectomy is a resource-intensive procedure: a study of Canadian health administrative data. Can J Anaesth 2017; 64: 724–735. doi: 10.1007/s12630-017-0888-y [DOI] [PubMed] [Google Scholar]
- 105.Lee HH, Dalesio NM, Lo Sasso AT, et al. . Impact of clinical guidelines on revisits after ambulatory pediatric adenotonsillectomy. Anesth Analg 2018; 127: 478–484. doi: 10.1213/ANE.0000000000003540 [DOI] [PubMed] [Google Scholar]
- 106.Amoils M, Chang KW, Saynina O, et al. . Postoperative complications in pediatric tonsillectomy and adenoidectomy in ambulatory vs inpatient settings. JAMA Otolaryngol Head Neck Surg 2016; 142: 344–350. doi: 10.1001/jamaoto.2015.3634 [DOI] [PubMed] [Google Scholar]
- 107.Allareddy V, Martinez-Schlurmann N, Rampa S, et al. . Predictors of complications of tonsillectomy with or without adenoidectomy in hospitalized children and adolescents in the United States, 2001–2010: a population-based study. Clin Pediatr 2016; 55: 593–602. doi: 10.1177/0009922815616885 [DOI] [PubMed] [Google Scholar]
- 108.Edmonson MB, Zhao Q, Francis DO, et al. . Association of patient characteristics with postoperative mortality in children undergoing tonsillectomy in 5 US states. JAMA 2022; 327: 2317–2325. doi: 10.1001/jama.2022.8679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lee CF, Hsu WC, Lee CH, et al. . Treatment outcomes of supraglottoplasty for pediatric obstructive sleep apnea: a meta-analysis . Int J Pediatr Otorhinolaryngol 2016; 87: 18–27. doi: 10.1016/j.ijporl.2016.05.015 [DOI] [PubMed] [Google Scholar]
- 110.Farhood Z, Ong AA, Nguyen SA, et al. . Objective outcomes of supraglottoplasty for children with laryngomalacia and obstructive sleep apnea: a meta-analysis. JAMA Otolaryngol Head Neck Surg 2016; 142: 665–671. doi: 10.1001/jamaoto.2016.0830 [DOI] [PubMed] [Google Scholar]
- 111.Bhushan B, Schroeder JW, Billings KR, et al. . Polysomnography outcomes after supraglottoplasty in children with obstructive sleep apnea . Otolaryngol Head Neck Surg 2019; 161: 694–698. doi: 10.1177/0194599819844512 [DOI] [PubMed] [Google Scholar]
- 112.Cockerill CC, Frisch CD, Rein SE, et al. . Supraglottoplasty outcomes in children with Down syndrome. Int J Pediatr Otorhinolaryngol 2016; 87: 87–90. doi: 10.1016/j.ijporl.2016.05.022 [DOI] [PubMed] [Google Scholar]