Summary
To investigate underlying mechanisms for cancer metastasis and promising therapies in animal models, spontaneous metastasis models can be used to recreate metastasis development. Here, we present three mouse models of spontaneous lung and/or liver metastasis induction. We describe steps for cancer cell preparation, mouse analgesia, and three injection techniques (subcutaneous, intracecal, and intramucosal). We then detail procedures for evaluating metastasis. Most of these models generate metastasis in a time span of 4 weeks in the majority of injected mice.
For complete details on the use and execution of this protocol, please refer to Giannou et al.1
Subject areas: Cancer, Immunology, Model Organisms
Graphical abstract

Highlights
-
•
Detailed protocol for three spontaneous metastasis mouse models
-
•
Detailed steps for preparing cancer cells and mouse analgesia
-
•
Steps for subcutaneous, intracecal, and intramucosal injections
Publisher’s note: Undertaking any experimental protocol requires adherence to local institutional guidelines for laboratory safety and ethics.
To investigate underlying mechanisms for cancer metastasis and promising therapies in animal models, spontaneous metastasis models can be used to recreate metastasis development. Here, we present three mouse models of spontaneous lung and/or liver metastasis induction. We describe steps for cancer cell preparation, mouse analgesia, and three injection techniques (subcutaneous, intracecal, and intramucosal). We then detail procedures for evaluating metastasis. Most of these models generate metastasis in a time span of 4 weeks in the majority of injected mice.
Before you begin
Metastasis is a multistep process beginning with intravasation. In this step, cancer cells disseminate from their primary site into the blood stream.2 In a consecutive step, cancer cells extravasate from the bloodstream into other organs, adapt to their new microenvironment, and grow to form metastasis.3 Depending on the location of the primary tumor, different metastatic sites can be distinguished. For colorectal carcinoma, the two most common sites are the lung and the liver.4
In general, two different types of animal models for the investigation of metastasis can be used. During forced models, cancer cells are injected directly into the blood stream resulting in extravasation into the nearest organ. Although these models possess some major advantages, their main caveat is that they bypass the step of intravasation, thus only allowing a partial investigation of the metastatic process.
In this collection of protocols, we will focus on our three most commonly used models for spontaneous liver and lung metastasis, namely a flank injection and subsequent removal of the primary tumor, an intramucosal injection, and an intracecal injection. Although these models are slightly more difficult to perform, they enable us to study the full metastatic process. We optimized these protocols so that they are easy to follow, and result in a high percentage of mice that develop metastasis.
Institutional permissions
These models describe experiments on living mice. All of these experiments must be performed in accordance with local and/or national guidelines and must follow appropriate regulations. All experiments for this protocol were approved by the Institutional Review Board “Behörde für Justiz und Verbraucherschutz (Veterinärwesen/Lebensmittelsicherheit)” (Hamburg, Germany) under the sanction numbers N088/19, G056/16 and N016/21.
Animal housing
Timing: 2 weeks
-
1.
Acquire 6- to 8-week-old mice and let them get used to your experimental area for 2 weeks. Both sexes can be used for all subsequent experiments. However, as the sex may influence the subsequent immune response, we recommend to always use sex-matched control groups or only use mice with the same sex for all experiments.
CRITICAL: Make sure to use the right background mouse strain for your tumor cells of choice. For the following, we will describe all further steps using the murine colorectal cancer cell line, MC38, for C57BL/6 mice. Alternatively, the murine colorectal cancer cell line, CT26, can be used equally when doing experiments with BALB/c mice.
CRITICAL: Make sure to always use sex- and age-matched experimental groups, since these factors may influence the outcome. Moreover, when using genetically modified mice, use wild-type littermates as control groups to minimize effects of different genetic backgrounds as a reason for observed differences between experimental groups.
Cell preparation
Timing: 1 week
-
2.
Bring 1 mL of cryopreserved MC38 cells that have been stored in a concentration of 1 million cells/mL in 10% DMSO/90% FBS to room temperature using a water bath.
-
3.
Transfer the solution of cells in 9 mL cell culture medium (see section “materials and equipment”; temperature 4°C and maximum storage 1–2 weeks) and centrifuge at 300 × g for 5 min in order to remove the DMSO.
-
4.
Seed cells onto a 100 mm petri dish by diluting the MC38 cells with 10 mL of cell culture medium.
-
5.
Incubate cells for 24 h in an incubator (5% CO2) at 37°C.
-
6.
Replace medium with 10 mL fresh cell culture medium and incubate cells for another 24 h in an incubator (5% CO2) at 37°C.
-
7.
Check cells daily under a microscope and proceed only when a confluence of 70% is reached.
-
8.Split cells.
-
a.Remove and discard the medium completely. Since the cancer cells are adherent, they should stick to the bottom of the plate.
-
b.Rinse the plate with 10 mL PBS (1X, without calcium and magnesium) and discard what has been washed off.
-
c.Add 1 mL of 0.05% Trypsin-EDTA to the cells and incubate the cells for 3 min in an incubator (5% CO2) at 37°C.
-
d.Add 19 mL fresh cell culture medium and resuspend the cells.
-
e.Centrifuge the cells and resuspend the pellet in 20 mL medium.
-
f.Divide the 20 mL medium with the cells onto two fresh 100 mm culture plates.
-
g.Incubate cells for further 24 h in an incubator (5% CO2) at 37°C.
-
a.
-
9.
Cells should be split at least 2–3 times before using for in vivo experiments.
-
10.
Split cells 24 h before conducting the rodent surgery 1:2.
-
11.
Before harvesting, check that a confluence of 50%–70% is reached.
CRITICAL: Cells have to be confluent around 50%–70% to ensure that they are in their exponential growth phase. Otherwise, mice might not develop any metastasis.
-
12.Harvest cells.
-
a.Discard the medium completely.
-
b.Rinse the plate with 10 mL PBS and remove what has been washed off.
-
c.Add 1 mL of Trypsin to the cells and incubate the cells for 3 min in an incubator (5% CO2) at 37°C.
-
d.Add 9 mL fresh cell culture medium and resuspend the cells.
 CRITICAL: Cell culture medium (see section “materials and equipment”) has to be added at this point since the FBS included stops the enzymatic activity of Trypsin.
CRITICAL: Cell culture medium (see section “materials and equipment”) has to be added at this point since the FBS included stops the enzymatic activity of Trypsin. -
e.Transfer cells with cell culture medium to a 50 mL Falcon tube and add 40 mL PBS.
-
f.Spin down at 300 × g for 5 min at room temperature.
-
g.Dispose of the supernatant.
-
h.Resuspend the pellet in 1 mL PBS.
-
i.Take a 10 μL aliquot of the cells and dilute it with 80 μL PBS and 10 μL Trypan blue.
-
j.Count cells.Note: A general yield of 5–10 million cells per plate should be expected.
 CRITICAL: Ensure a viability of >90% of counted cancer cells.
CRITICAL: Ensure a viability of >90% of counted cancer cells. -
k.Dilute cells with PBS to a concentration of 5 million cells per mL for the flank model, 5–10 million cells per mL for the cecum model, and a concentration of 1–6 million cells per mL for intramucosal injections.Note: Alternative cancer cell lines might require different cell concentrations for appropriate metastatic yield.
-
l.Aliquot cells in 1 mL aliquots. Transport and store them subsequently on ice.
 CRITICAL: Do not store cancer cells on ice for more than 2 h. If more mice are desired to be injected, harvest cells multiple times.
CRITICAL: Do not store cancer cells on ice for more than 2 h. If more mice are desired to be injected, harvest cells multiple times.
-
a.
Key resources table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Chemicals, peptides, and recombinant proteins | ||
| PBS | Dirk Hindorf Anprotec | AC-BS-0002 |
| FBS | Capricorn | CS-HI-1A |
| EDTA | Carl Roth GmbH | 8043.2 |
| DMEM (GlutaMAX) | Gibco | 31966047 |
| Penicillin/Streptomycin | Gibco | 15070-063 |
| Metamizole | Ratiopharm GmbH | 9051799 |
| Buprenorphine | Temgesic | 00345928 |
| 0.05% Trypsin-EDTA | Gibco | 25300-054 |
| Experimental models: Cell lines | ||
| MC38 | Giannou et al.1 | N/A |
| Experimental models: Organisms/strains | ||
| C57BL/6J mice, wild type, adult, both sexes | The Jackson Laboratory | N/A |
| Other | ||
| Induction chamber for small animals | ||
| Ventilator for small animal use, e.g., UMV-03 UNO Microventilator | UNO Roestvaststaal BV | 180000023 |
| Isoflurane vaporizer | UNO Roestvaststaal BV | 180000008 |
| Flowmeter CM2 | UNO Roestvaststaal BV | 180000002 |
| Heating plate | UNO Roestvaststaal BV | 180000028 |
| Laboratory stand with clamp | Zeiss | KL1500 LCD |
| Small surgical scissors | Fine Science Tools | 14060-09 |
| Student Adson forceps 1 × 2 teeth | Fine Science Tools | 91127-12 |
| Semken forceps curved 15 cm | Fine Science Tools | 11009-15 |
| Hand shaver machine | Aesculap | GT420 |
| Needle holder | Aesculap | BMO22R |
| Metal suture clips, 11 × 2 mm | Aesculap | BN511R |
| Metal suture clips applier | Aesculap | BN750R |
| Prolene 3-0 | Ethicon, Inc. | VCP311H |
| Injekt F, 1 mL syringe | B. Braun | 9166017V |
| 21-gauge needle, 0.80 × 40 mm | B. Braun | 4657527 |
| 26-gauge needle, 0.45 × 13 mm | B. Braun | 303800 |
| 32-gauge needle, 0.23 × 12 mm | Mesoram | 712306 |
| Gauze compresses, 5 × 5 cm | Fink & Walter | 731021 |
| Cotton swabs, wood, 15 cm | NOBA Verbandmittel | 10859 |
| Betaisodona solution | Mundipharma GmbH | 6108022.00.01 |
| Isofluran-Piramal (Isoflurane) 250 mL | Piramal Critical Care BV | N/A |
| Temgesic Ampullen (buprenorphine hydrochloride, 0.3 mg/mL) | Indivior Europe Ltd. | N/A |
| Operating sheath | Karl Storz | 61029D |
| Small hub RN needle, 33-gauge | Hamilton | 7803-05 |
| Removable needle syringe, 100 μL | Hamilton | 7656-01 |
| HOPKINS straight forward telescope 0° (endoscope) | Karl Storz | 28731AWA |
| Neubauer hemocytometer (cell counting) | Neubauer | 68052-14, 68052-15 |
Materials and equipment
Analgetic drinking water
| Reagent | Final concentration | Amount |
|---|---|---|
| Autoclaved drinking water | 95% | 200 mL |
| Glucose | 5% | 10 g |
| Metamizole | <1% | 1000 mg |
The analgetic drinking water should be prepared and replaced daily (temperature 22°C–23°C and maximum storage 24 h).
Cell culture medium
| Reagent | Final concentration | Amount |
|---|---|---|
| DMEM medium | 90% | 450 mL |
| FBS | 10% | 50 mL |
| Penicillin/Streptomycin (5000 unit/mL Pen and 5000 μg/mL Strep) | <1% | 5 mL |
The cell culture medium has to be prepared and stored under sterile conditions (temperature 4°C and maximum storage 1–2 weeks).
Step-by-step method details
Flank model
Timing: 15 min per mouse
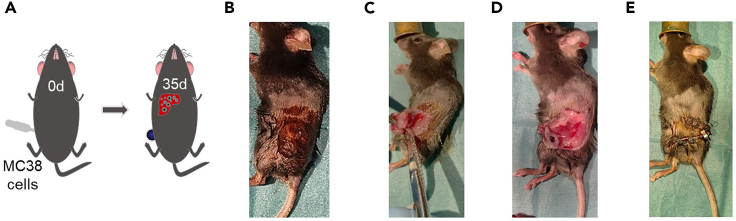
This part of the protocol describes a variation of the commonly used flank model (Figure 1A) as a spontaneous model for lung and liver metastasis. To limit primary tumor growth and suffering of the experimental mice, a resection of the primary tumor is performed 2 weeks after injection of the primary tumor.
-
1.
24 h before starting rodent surgery, replace the drinking water of mice with analgetic drinking water (see section “materials and equipment”).
CRITICAL: Change this analgetic drinking water daily.
-
2.Prepare cancer cells.
-
a.Resuspend aliquoted cancer cells by aspirating them thrice with a 21-gauge needle and a 1 mL syringe.
 CRITICAL: A 21-gauge needle for cell-resuspension should be used to minimize shear forces and to enhance cell viability. Cells need to be resuspended multiple times as they sink to the bottom of the tube quickly.
CRITICAL: A 21-gauge needle for cell-resuspension should be used to minimize shear forces and to enhance cell viability. Cells need to be resuspended multiple times as they sink to the bottom of the tube quickly. CRITICAL: Avoid air bubbles.
CRITICAL: Avoid air bubbles. -
b.Carefully aspirate 100 μL of the resuspended cancer cells with a 26-gauge needle.
 CRITICAL: Keep and store the cancer cells on ice. Before aspiration of cancer cells always mix the cells well in order to have the same amount of cancer cells/100 μL.
CRITICAL: Keep and store the cancer cells on ice. Before aspiration of cancer cells always mix the cells well in order to have the same amount of cancer cells/100 μL.
-
a.
-
3.
Anesthetize one mouse by using an appropriate induction chamber with an oxygen flow of 500 mL/min with 5% nebulized isoflurane until a respiratory rate of 1/s is achieved and the inter-toe reflex is lost.
-
4.
Shave the left lower back part of the mouse starting from the spine until the lateral abdominal wall.
-
5.
Maintain anesthesia by using the same oxygen flow with 2%–3% isoflurane provided via a mask.
-
6.
Position the mouse on its right side with the shaved part facing upwards (Figure 1B).
-
7.
Apply betaisodona-solution on the shaved part thrice and let it dry for 3 min.
-
8.
Carefully inject the 100 μL containing the cancer cells into the flank of the mouse with a 26-gauge needle (Figure 1C).
CRITICAL: A subcutaneous bubble should form during injection. Otherwise, the injection is accidentally performed in a deeper tissue layer and the mouse needs to be sacrificed.
-
9.
After injection, wait 30 s with the needle still inside the flank (Figure 1D).
-
10.
Quickly remove the needle and immediately press a sterile gauge on the flank for 20 s.
-
11.
Remove the gauge and check that no further bleeding or leaking from the injected part occurs.
-
12.
Place the mouse back into its cage and monitor it until it is fully awake.
-
13.
Check the mice daily for complications. Measure the growth of the primary tumor daily by measuring its three dimensions.
Note: Tumor volume (in mm3) can be calculated by the volume formula pi/6 x L x W x H.
-
14.
Once the primary tumor with or without a macroscopic ulceration is visible, proceed to the operative resection of the tumor.
-
15.
24 h before starting this surgery, replace the drinking water of mice with analgetic drinking water.
-
16.
On the day of the operation, perform additional analgesia by injecting 0.2 mg metamizole per g bodyweight dissolved in PBS subcutaneously. Wait 15–30 min.
Note: Alternatively, buprenorphine can also be used. We recommend a subcutaneous injection of 0.1 μg buprenorphine per g bodyweight dissolved in PBS.
-
17.
Then, anesthetize one mouse again by using an appropriate induction chamber with an oxygen flow of 500 mL/min with 5% nebulized isoflurane until a respiratory rate of 1/s is achieved and the inter-toe reflex is lost.
-
18.
Re-shave the left lower back part of the mouse starting from the spine until the lateral abdominal wall.
-
19.
Maintain anesthesia by using the same oxygen flow with 2%–3% isoflurane provided via a mask.
-
20.
Position the mouse on its back with the shaved part facing upwards.
-
21.
Use Bepanthen ointment to protect the eyes from drying out.
-
22.
Keep the mouse on a warming plate during the entire operation to prevent hypothermia.
-
23.
Apply betaisodona-solution on the shaved part thrice and let it dry for 3 min.
-
24.
Perform an incision starting at the cranial part of the tumor and ending at the caudal part of the tumor (Figure 2B).
-
25.
Using a pair of scissors in your dominant hand and a forceps holding the skin of the mouse in your non-dominant hand, gently dissect the skin from the tumor (Figure 2C).
-
26.
Now, gently dissect the tumor from the surrounding subcutaneous tissue.
-
27.
Once the tumor is fully resected, carefully check that no parts of the tumor are left inside (Figure 2D).
-
28.
Check that no bleeding occurs. If significant bleeding occurs, sacrifice the mouse.
-
29.
Perform a lavage with 2 mL PBS at body temperature.
-
30.
Close the opened skin with 3–5 metal clips (Figure 2E).
-
31.
Place the mouse back into its cage and monitor it until it is fully awake.
-
32.
Mice may be transferred into a heating rack for up to 24 h after surgery.
-
33.
Check the mice daily for complications, unwanted regrowth of primary tumor or too fast growth of metastasis.
-
34.
The analgetic drinking water can be changed into normal drinking water 48 h after surgery.
-
35.
Normal wound healing implied, metal clamps should be removed 10–14 days after surgery.
-
36.
Mice should be euthanized 28 days after primary surgery.
Figure 1.
Flank injection of cancer cells
(A) Schematic view of flank injection of cancer cells.
(B) Disinfecting shaved area.
(C) Carefully inserting the needle into the flank.
(D) Injection of cancer cells and waiting for 30 s.
Figure 2.
Flank tumor resection
(A) Schematic view of flank injection of cancer cells.
(B) Disinfecting shaved area.
(C) Carefully resecting the flank tumor.
(D) Removal of flank tumor by maintaining the skin.
(E) After removal of flank tumor skin adaptation with metal clips.
Intracecal injection
Timing: 20 min per mouse
This part of the protocol describes a method for an intracecal injection (Figure 3A) as another model for spontaneous liver metastasis. After developing a primary tumor on the outer cecal wall, the majority of these mice will also develop liver metastasis (Methods video S1).
-
37.
24 h before starting rodent surgery, replace the drinking water of mice with analgetic drinking water (see section “materials and equipment”).
CRITICAL: Change this analgetic drinking water daily.
-
38.
Perform additional analgesia by injecting 0.2 mg metamizole per g bodyweight dissolved in PBS subcutaneously. Wait 15–30 min.
Note: Alternatively, buprenorphine can also be used. We recommend a subcutaneous injection of 0.1 μg buprenorphine per g bodyweight dissolved in PBS.
-
39.Prepare cancer cells.
-
a.Resuspend aliquoted cancer cells by aspirating them thrice with a 21 -gauge needle and a 1 mL syringe.
 CRITICAL: A 21-gauge needle for cell-resuspension should be used to minimize shear forces and to enhance cell viability. Cells need to be resuspended multiple times as they sink to the bottom of the tube quickly.
CRITICAL: A 21-gauge needle for cell-resuspension should be used to minimize shear forces and to enhance cell viability. Cells need to be resuspended multiple times as they sink to the bottom of the tube quickly. -
b.Carefully aspirate 50 μL of the resuspended cancer cells with a 32-gauge needle.
 CRITICAL: The small gauge-size of the needle is of critical importance, since it greatly reduces perforation of the needle into the cecal lumen.
CRITICAL: The small gauge-size of the needle is of critical importance, since it greatly reduces perforation of the needle into the cecal lumen. CRITICAL: Avoid air bubbles.
CRITICAL: Avoid air bubbles.
-
a.
-
40.
Anesthetize one mouse by using an appropriate induction chamber with an oxygen flow of 500 mL/min with 5% nebulized isoflurane until a respiratory rate of 1/s is achieved and the inter-toe reflex is lost.
-
41.
Shave the frontal abdominal part of the mouse.
-
42.
Maintain anesthesia by using the same oxygen flow with 2%–3% isoflurane provided via a mask.
-
43.
Position the mouse on its back with the shaved part facing upwards.
-
44.
Use Bepanthen ointment to protect the eyes from drying out.
-
45.
Keep the mouse on a warming plate during the entire operation to prevent hypothermia.
-
46.
Apply betaisodona-solution on the shaved part thrice and let it dry for 3 min.
-
47.
Perform a 2 cm midline-incision with sharp scissors from the middle abdominal part until the pubic bone (Figure 3B). The muscle layer should become visible.
-
48.
Lift the muscle layer up using a blunt forceps and perform a 2 cm incision into the muscle layer so that the abdominal cavity is opened.
CRITICAL: Perform this step with care to avoid damaging the small intestine during this step. If the intestine is damaged, mice will present themselves with symptoms of peritonitis or ileus and a general reduction in their general condition.
-
49.
The cecum should become visible in the lower left part of the opened abdomen. Grab it with blunt forceps and gently pull it out of the abdominal cavity so that the whole cecum becomes visible (Figure 3C).
-
50.
Using a very sharp angle of injection of 10°–20°, inject all of the 50 μL of prepared cell-suspension into the outer wall of the cecum (Figure 3D).
CRITICAL: The formation of a bubble of the injected cecum wall should be immediately visible upon injection. If this is not the case, the injection was likely performed intraluminally, and the mouse needs to be euthanized.
-
51.
After injection, wait 1 min with the needle still inside the wall.
-
52.
Quickly remove the needle.
-
53.
Remove the swab and check that no further leaking or bleeding occurs.
-
54.
Relocate the cecum back inside the abdomen.
-
55.
Perform a continuous suture of the abdominal wall using Vicryl 3-0.
-
56.
Close the opened skin with 3–5 metal clips (Figure 3E).
-
57.
Place the mouse back into its cage and monitor it until it is fully awake.
-
58.
Mice may be transferred into a heating rack for up to 24 h after surgery.
-
59.
Check the mice daily for complications, for example, growth of the primary tumor may be too fast, growth of liver metastasis may be too fast or the development of peritoneal metastasis. From our experience, it is sufficient to evaluate the mice for a tense abdomen, palpable peritoneal metastasis or a general reduction in their general condition. However, regular MRI- or CT-scans might also present a possibility for evaluation of complications.
-
60.
The analgetic drinking water can be changed into normal drinking water 48 h after surgery.
-
61.
Normal wound healing implied, metal clamps should be removed 10–14 days after surgery.
-
62.
Mice should be euthanized 28 days after surgery.
Figure 3.
Intracecal injection of cancer cells
(A) Schematic view of intracecal injection of cancer cells.
(B) 2 cm midline-incision from the middle abdominal part until the public bone.
(C) Exposure of cecum.
(D) Carefully inserting the needle into the outer wall of the cecum and injecting cancer cells.
(E) Skin closure using metal clips.
Intramucosal injection
Timing: 5 min per mouse
This part of the protocol describes the intramucosal injection (Figure 4A) of cancer cells into the rectum for the development of a rectal primary tumor (Methods video S2). Compared to the intracecal-injection-model, the advantages lie within the fact that this is a fully orthotopic model for rectal or distal colon cancer, the most common location for CRC. Moreover, the tumor grows physiologically from the mucosa to the other layers of the colon, whereas the cecum-injection-model primarily leads to a tumor growth from the colonic serosa. In some cases, micrometastasis in the liver might be observed. However, the majority of mice need to be euthanized before the development of metastasis, due to the fast growth of the primary tumor, and subsequent complications such as bowel obstructions, bleeding, or infiltrations in surrounding tissues such as the ureter or the bladder. Of note, this model requires the availability of an endoscope for small animals with a special working channel for cancer cell injection as well as profound experience in small animal endoscopy. This model must be performed by two researchers.
-
63.
24 h before starting rodent surgery, replace the drinking water of mice with analgetic drinking water (see section “materials and equipment”).
CRITICAL: Change this analgetic drinking water daily.
-
64.Researcher 1: Prepare cancer cells.
-
a.Resuspend aliquoted cancer cells by aspirating them thrice with a 21-gauge needle and a 1 mL syringe.
-
b.Carefully aspirate 50 μL of the resuspended cancer cells in a Hamilton syringe. Carefully store the Hamilton syringe until injection.
-
a.
CRITICAL: Avoid air bubbles.
-
65.
Researcher 2: Prepare the endoscope according to the manufacturer’s instructions.
-
66.
Researcher 1 and 2: Prepare the endoscope by inserting the injection-needle through the second channel of the endoscope. A Luer lock is screwed on the second channel (yellow color) to avoid air leakage (Figure 4B).
-
67.
Researcher 1 and 2: Anesthetize one mouse by using an appropriate induction chamber with an oxygen flow of 500 mL / min with 5% nebulized isoflurane until a respiratory rate of 1 / s is achieved and the inter-toe reflex is lost.
-
68.
Researcher 1 and 2: Maintain anesthesia by using the same oxygen flow with 2%–3% isoflurane provided via a mask.
-
69.
Researcher 2: Carefully apply pressure from both sides of the anus to remove stool pellets from the rectum.
-
70.
Researcher 2: Insert the endoscope through the anus of the mouse and gently push it until the flexura colica sinistra approximately 3–4 cm into the anus (Figure 4C). Carefully and slowly retract the endoscope. Select a suitable position for injection. Such a position can usually be found at 5 o'clock approximately 2–3 cm into the colon.
Note: Vaseline can be applied to the endoscope to enhance lubricity.
CRITICAL: Avoid pushing the endoscope against any resistance since it might lead to perforation of the colon.
CRITICAL: Make sure that no big vessel is near the injection site, since injection into vessels might lead to uncontrollable bleeding.
-
71.
Researcher 1: Now gently move the injection needle forward until it becomes visible on the screen.
-
72.
Researcher 2: Gently tilt the endoscope to the site of injection so that the needle tip and colon wall are as close together as possible.
Note: Researcher 2 can apply gentle pressure on the left lower part of the abdomen from outside with the hand not holding the endoscope. This maneuver brings the colonic wall and the endoscope even closer together.
CRITICAL: Although the colonic wall and endoscope should be as close together as possible, the angle of injection must not exceed 20°. Otherwise, the colon might be perforated, and the cancer cells are injected into the peritoneum.
-
73.
Researcher 1: Move the needle even further forward until it penetrates the colonic wall in an angle of maximal 20°. Then carefully move the needle 1 mm further until the lumen of the needle is completely inserted into the colonic wall (Figure 4D).
CRITICAL: The lumen of the injection needle should always face upwards.
-
74.
Researcher 2: Gently move the endoscope upwards to perform a lift-up-test and control the correct position of the needle.
Note: The lift-up-test is positive if the needle stays into the colonic wall and repositioning of the endoscope leads to an uplifting of the mucosal layer.
-
75.
Researcher 1: Carefully inject 50 μL of the cancer cell suspension via the connected Hamilton-syringe.
CRITICAL: A mucosal bubble should form immediately after injection. If this is not the case, the injection has been performed in the peritoneum (Figure 4E).
-
76.
Wait 30 s with the needle inside the colonic wall.
-
77.
Remove the needle completely and ensure that no bleeding from the injection site or leaking of injected fluid occurs.
-
78.
Remove the endoscope from the anus.
-
79.
Place the mouse back into its cage and monitor it until it is fully awake.
-
80.
Check the mice daily for complications such as peritonitis, ileus, or peritoneal metastasis. These complications can be diagnosed by evaluating the mice for a tense abdomen, palpable peritoneal metastasis or a general reduction in their general condition. However, regular MRI- or CT-scans might also present a possibility for evaluation of complications.
-
81.
Endoscopy should be performed regularly to monitor the growth of the primary tumor.
-
82.
Normally, mice should be euthanized 7–14 days after cell injection.
Figure 4.
Intramucosal injection of cancer cells
(A) Schematic view of intramucosal injection of cancer cells.
(B) Preparation of endoscope (the needle was set through the yellow cap as marked).
(C) Inserting endoscope into the anus of the mouse.
(D) Carefully inserting the needle into the colonic wall.
(E) After injection, a mucosal bubble should form.
Expected outcomes
Depending on the model used, different outcomes are expected. With the flank model and the cecum model, the development of metastasis is observed in the majority of mice. Of course, the number of mice without metastasis and the average yield of metastasis is significantly lower, approximately 70% than with forced models of metastasis. Nonetheless, intra-, and postoperative mortality of these models are very low and lie between 0.5% and 1%. From the 14th postoperative or postinterventional day onwards, mice have to be monitored very closely to detect complications regarding accelerated growth of the primary tumor.
Regarding the intrarectal injection, macroscopic metastases do not develop normally. However, in some cases, micrometastasis can be detectable. After a training interval of approximately 50 mice, intra- and postinterventional mortality is low. As already mentioned above, the growth of the primary tumor has to be monitored closely. In some cases, mice have to be sacrificed prematurely due to an aggravated growth of the primary tumor with bleeding or obstruction of the colonic lumen.
Quantification and statistical analysis
After euthanasia, we recommend a specific method for post-mortem tissue harvest to ensure the highest quality for macroscopic and microscopic assessment of metastatic lesion number. Macroscopic counting of metastasis should always be carried out in a blinded fashion. Inspect every organ from each accessible side in a structured fashion. For microscopic counting of metastasis, use a representative histological slide after H&E staining.1 The percentage of the metastatic area of the organ can be assessed using common software.
Limitations
Limitations of these methods are mainly based on the fact that cancer cell lines are injected. These cell lines mimic central aspects of cancer development, but are far less heterogeneous than naturally evolving cancer. However, the described models can also be carried out using tumor organoids that are characteristically closer to cancer development than cancer cell lines. Second, although these models are spontaneous models of metastasis in a sense that they have to metastasize from a distant primary tumor site, the flank model and the cecum model are not fully orthotopic. Although the intrarectal injection model mimics cancer development at the correct anatomical site, its growth is too fast to fully develop liver metastasis. Whether it is possible to slow down tumor development by injecting less cancer cells needs to be addressed in future studies.
Troubleshooting
Problem 1
High intra- or postinterventional mortality (related to step 2–12 in before you begin; related to step 37–82).
Potential solution
-
•
Re-evaluate anesthetic protocol, reduce duration of operation, reduce exposure to isoflurane.
-
•
Increase duration of recovery phase in heating cages.
-
•
Reduce concentration of cancer cells.
-
•
Change out buffers to exclude contamination of reagents used.
Problem 2
No metastasis after the end of the experiment (related to step 2–12 in before you begin).
Potential solution
-
•
Make sure that cancer cells were harvested during their exponential growth phase.
-
•
Make sure that the genetic background of cancer cell matches the genetic background of the injected mice.
-
•
Exclude genetic contamination of mouse strains used.
-
•
Exclude contamination of cancer cells and/or mycoplasma infection.
-
•
Confirm sufficiently high viability of cancer cells before injection.
-
•
Increase concentration of cancer cells.
Problem 3
Regrowth of primary tumor after resection in the flank model (related to step 14–35).
Potential solution
-
•
Ensure that the primary tumor was fully resected during the first operation.
-
•
Reduce amount of injected cancer cells.
Problem 4
Intraperitoneal cancer growth in the intramucosal model or cecum model (related to step 50–55; related to step 71–82).
Potential solution
-
•
Ensure that cells were injected in the colonic/cecal wall by watching the formation of a bubble.
-
•
Reduce amount of injected cancer cells.
Problem 5
Too many metastases (related to step 2–12 in before you begin; related to step 50–82).
Potential solution
-
•
Sacrifice future mice at an earlier time point.
-
•
Reduce concentration of cancer cells.
Resource availability
Lead contact
Further information and requests for resources and reagents should be directed to and will be fulfilled by the lead contact, Anastasios Giannou (a.giannou@uke.de).
Technical contact
For any technical inquiries or additional information regarding the methods used in this study, please contact Feijing Wu (fw2345@cumc.columbia.edu).
Materials availability
This study did not generate new unique reagents.
Data and code availability
This study generated neither datasets nor code.
Acknowledgments
The authors thank Tom Blankenburg, Sandra Wende, and Cathleen Haueis for their excellent technical assistance. The graphical abstract was in part created with BioRender.com. This work was supported in part by the Deutsche Forschungsgemeinschaft (grant SFB841 to S.H.), the Deutsche Krebshilfe (nr. 70114853, to A.D.G.), Else Kröner Memorial Stipendium (to A.D.G.), Erich und Gertrud Roggenbuck-Stiftung (to A.D.G.), Hamburger Krebsgesellschaft Stiftung (to A.D.G.), and the Jung Foundation for Science and Research (to A.D.G.). S.H. has an endowed Heisenberg Professorship awarded by the Deutsche Forschungsgemeinschaft.
Author contributions
J.L., T.Z., and A.D.G. performed all rodent surgeries and prepared the figures. J.L., B.M., and T.Z. wrote the manuscript. D.E.Z. and P.S. created the videos and edited the manuscript. E.Z. showed us the intramucosal injection in mice and helped us to establish this method. O.M., J.R.I., and T.H. edited the manuscript and provided intellectual input. S.H. and A.D.G. provided scientific supervision and revised and finalized the manuscript.
Declaration of interests
The authors declare no competing interests.
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.xpro.2023.102811.
Contributor Information
Jöran Lücke, Email: j.luecke@uke.de.
Anastasios D. Giannou, Email: a.giannou@uke.de.
References
- 1.Giannou A.D., Kempski J., Shiri A.M., Lücke J., Zhang T., Zhao L., Zazara D.E., Cortesi F., Riecken K., Amezcua Vesely M.C., et al. Tissue resident iNKT17 cells facilitate cancer cell extravasation in liver metastasis via interleukin-22. Immunity. 2023;56:125–142.e12. doi: 10.1016/j.immuni.2022.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fares J., Fares M.Y., Khachfe H.H., Salhab H.A., Fares Y. Molecular principles of metastasis: a hallmark of cancer revisited. Signal Transduct. Target. Ther. 2020;5:28. doi: 10.1038/s41392-020-0134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Welch D.R., Hurst D.R. Defining the Hallmarks of Metastasis. Cancer Res. 2019;79:3011–3027. doi: 10.1158/0008-5472.CAN-19-0458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hess K.R., Varadhachary G.R., Taylor S.H., Wei W., Raber M.N., Lenzi R., Abbruzzese J.L. Metastatic patterns in adenocarcinoma. Cancer. 2006;106:1624–1633. doi: 10.1002/cncr.21778. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This study generated neither datasets nor code.