Abstract
A 2-month-old, female cat was presented for abdomen dilation. The patient was undernourished, and severe left hydronephrosis was diagnosed after clinical, ultrasonographical and radiographical examination. Although pyelography was performed in order to visualise the ureteral course, surgery was necessary to reach a final aetiological diagnosis and treatment. At gross examination, the left ureter crossed the renal capsula at the level of the caudal renal pole, and the subcapsular ureteral segment was markedly dilated. Distal to the renal capsula, the left ureter was very thin when compared to the right. The parenchyma of the left kidney, as suggested by ultrasonographical evaluation, was extremely reduced in thickness. An ureteronephrectomy was performed. Histopathological evaluation revealed glomerular sclerosis and diffuse parenchymal fibrosis. Severe hydronephrosis derived from an altered renal pelvic anatomy and abnormal ureteral course determining functional stenosis. Diagnosis of congenital anomaly before development of complications such as hydronephrosis could have allowed a surgical renal capsulectomy and obstruction relief. To the author's knowledge, this is the first report of severe hydronephrosis associated to altered renal pelvic anatomy and proximal ureteral ectopia in cat.
A 2-month-old, 510 g, female cat, was referred for abdomen dilation of 4 weeks duration. On physical examination, the cat was undernourished. On abdominal palpation, a large smooth mass occupying most of the abdomen was identified; kidneys were not detected. Lateral and ventro-dorsal abdominal radiographs identified, in the medium and caudal abdomen, a mass with homogenous fluid opacity displacing cranially the abdominal viscera. During ultrasonographic evaluation, performed with a 10 MHz linear transducer, the right kidney was identified and considered normal for echogenicity, shape, dimension and anatomical position. The left kidney was severely hydronephrotic and at Color Doppler and Pulsed Doppler evaluation, interlobar arteries were identified. Echo-contrast study performed with 0.5 ml of second-generation compound made of an aqueous suspension of stabilised sulphur hexafluoride (SF6) micro-bubbles (Sonovue; Bracco) given intravenously revealed poor renal parenchymal perfusion and non-perfused areas compatible with cystic lesions. In order to identify the cause of hydronephrosis, a radiological contrast study was performed by ultrasonographically guided percutaneous antegrade pyelography (Rivers et al 1997). Severe hydronephrosis of left kidney was confirmed but the ureter was not identified. Complete blood count (CBC) and serum biochemistry were within reference ranges. Urinalysis revealed urine specific gravity of 1014; several erythrocytes and renal epithelial cells were observed in the urine sediment.
The cat was placed under general anaesthesia and induction was obtained using midazolam 0.2 mg/kg IV (Ipnovel; Roche) followed by propofol given intravenously to effect (Rapinovet; Schering-Plough). A 1.5 mm endotracheal tube (Veterinary straight endotracheal tube; Cook) was placed and anaesthesia maintained by isoflurane (Isoba; Schering-Plough). Analgesic plan was instituted using buprenorphine 10 μg/kg IM (Temgesic; Schering-Plough).
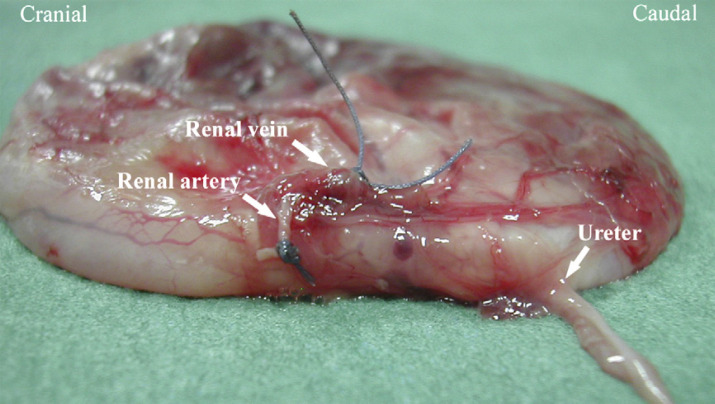
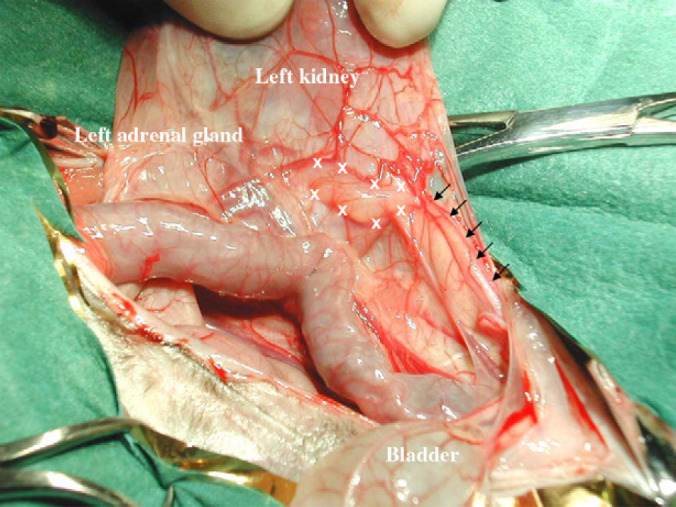
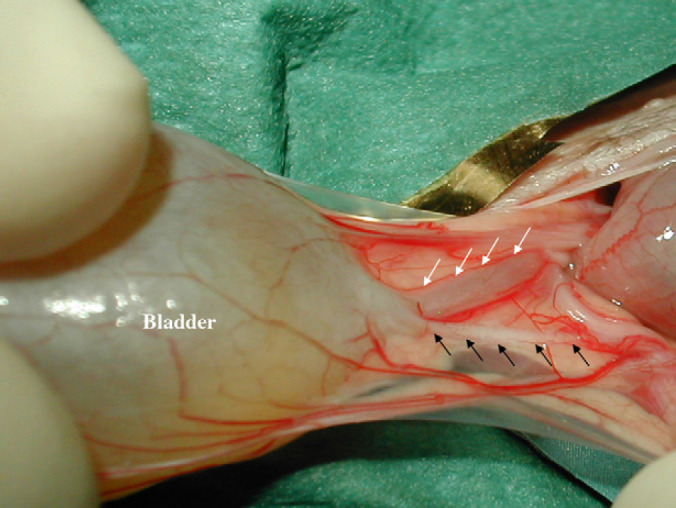
A standard ventral midline surgical approach was performed. The left kidney appeared severely enlarged occupying the central and caudal abdomen; 180 cc fluid were drained from the hydronephrotic kidney using a 60 cc syringe connected to a 23 gauge needle. Samples were collected and underwent cytological examination and bacterial culture. The affected kidney was exteriorised and the ureter was identified in order to visualise shape and/or location abnormalities. At gross examination, the left ureter crossed the renal capsula at the level of the caudal renal pole and the subcapsular ureteral segment was markedly dilated for 14 mm of its length (Fig 1). Distal to the renal capsula, the left ureter was very thin compared to the right (Fig 2). The parenchyma of the left kidney, according with previous ultrasonographical evaluation, was extremely reduced in thickness. A left ureteronephrectomy was performed. Left kidney isolation was performed with care in identifying and protecting close structures. Left adrenal gland was identified cranial to the enlarged kidney and left in site together with the phrenicoabdominal vein. Bleeding from the capsular vessels was easily controlled. Both the renal vein and artery were isolated and ligated separately; the left ureter was ligated close to the bladder. Because of the thinness of subcutaneous tissue, the surgical suture consisted only of two different planes (fascia and skin). At gross appearance, the renal pelvis was altered in structure, location and, at the level of renal hylum, ureter was caudal to renal vessels (Fig 3). Left kidney and ureter were fixed in 10% neutral buffered formalin with respect to a sample:formalin ratio of 1:10. The patient had a successful recovery from anaesthesia. Cytological evaluation of the drained fluid revealed erythrocytes and renal epithelial cells. The bacterial culture was negative. Histopathology of the resected hydronephrotic kidney and ipsilateral proximal ureter revealed diffuse fibrosis of the tubulointerstitial compartment, pelvic and proximal ureter fibrosis, and glomerular sclerosis (Fig 4).
Fig 1.
Surgical view of left ureter crossing renal capsula at the level of the caudal renal pole. It is possible to observe the dilated proximal ureteral segment (between white calipers) and the thin distal one (black arrows).
Fig 2.
Surgical view of bladder trygone area showing comparison between left and right ureters. Left ureter (black arrows) appears severely reduced in diameter with respect to the controlateral (white arrows).
Fig 3.
Gross appearance of left renal pelvis showing ureteral ectopia. The ureter arises from the caudal pole of the left pelvis.
Fig 4.
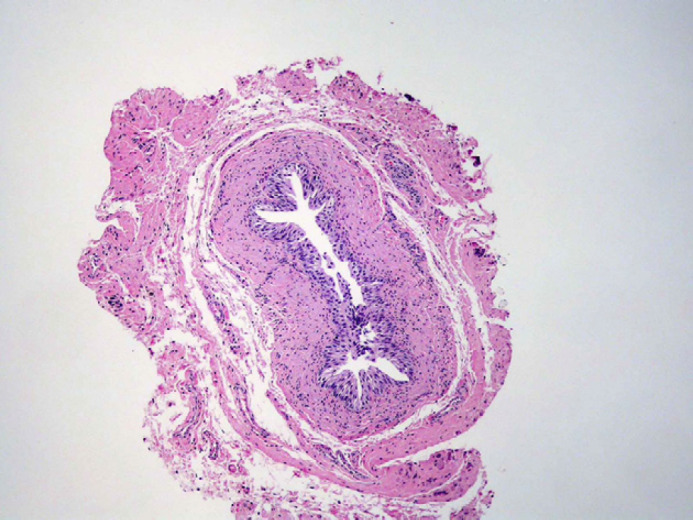
Transverse section of the left ureter at the level crossing renal capsula. It is possible to observe tissue fibrosis. Haematoxylin–eosin (20×).
The cat was re-examined 14 days postoperatively. The owner reported normal behaviour and activity and, at clinical examination, weight gain and better body condition were observed. CBC and serum biochemistry were within the reference ranges.
Discussion
Unilateral hydronephrosis has been reported in 8-week- to 8-year-old cats without breed predilection; patients most often affected are females (DiBartola and Rutgers 1994). Unilateral renal enlargement can be asymptomatic, and progressive abdominal distention can be detected at physical examination (Finco 1995). Bacterial infection of the hydronephrotic kidney can occur resulting in pyonephrosis and associated clinical signs are lethargy, anorexia, pyrexia, haematuria, pyuria, bacteriuria and leukocytosis (DiBartola and Rutgers 1994). As in our case, some authors' report that cats with uncomplicated unilateral hydronephrosis show a usually normal CBC, blood urea nitrogen and serum creatinine concentrations (DiBartola and Rutgers 1994). Detection of concentrated urine is a common finding on urinalysis. Reported causes of unilateral hydronephrosis include uroliths or blood clots in the ureter or renal pelvis, unilateral ectopic ureter, accidental ligation of a ureter during ovariohysterectomy, ureteral stricture or stenosis, ureterocele, ureteral or renal pelvic neoplasia, and retroperitoneal tumour causing extraluminal ureteral compression (DiBartola and Rutgers 1994, Cuypers et al 1997, Rawlings et al 2002).
Only one case of hydronephrosis and hydroureter in a kitten deriving from ureteral stenosis was previously reported (North 1978) and, to the author's knowledge, this is the first case of severe unilateral hydronephrosis associated with altered renal pelvic anatomy and proximal ureteral ectopia in a cat. The caudal location of the left ureter associated with a subcapsular course towards the caudal renal pole caused a functional stenosis where the ureter crossed the renal capsula (Figs 1 and 3). The congenital anomaly in the ureteral location was associated with an abnormal development of the ureter that appeared severely reduced in diameter, when compared to the controlateral ureter, distally to the stenosic segment and till the entrance into the bladder trygone (Fig 2). The diagnosis of a congenital anomaly before development of complications such as hydronephrosis could have allowed a conservative treatment of the left kidney by surgical capsulectomy. Infact, if the cause of hydronephrosis is removed within 1 week from beginning, renal damage is reversible and up to 25% of normal renal function can return if obstruction relief is carried out after 4 weeks of total obstruction (Rawlings et al 2002). But, ureteral obstruction of several weeks duration may also result in complete loss of renal function and the affected kidney may present as a fibrous sac with no residual function (DiBartola and Rutgers 1994, Rawlings et al 2002, Klahr and Morrissey 2002). In our case, a preoperative aetiological diagnosis by ultrasonographical and pyelographical evaluation, was not possible. Although other authors have previously reported percutaneous antegrade pyelography as diagnostic in all cases evaluated (Rivers et al 1997), in our patient this examination was not diagnostic perhaps because of the severe dilation of the renal pelvis and the collecting system that determined abdominal organ displacement and kidney and ureter summation during X-ray examination. The summation shadow created by overlapping of the hydronephrotic kidney and dilated ureter resulted in loss of ureteral visualisation in spite of contrast medium administration. In our patient, perhaps because of severe renal enlargement due to hydronephrosis and ureter–kidney overimpression, pyelography examination provided no advantage in identifying the cause of urinary tract obstruction and the surgical approach was necessary in order to visualise congenital structure anomaly.
References
- Cuypers M.D., Grooters A.M., Williams J., Partington B.P. Renomegaly in Dogs and Cats. Part I. Differential diagnoses, Compendium on Continuing Education 19 (9), 1997, 1019–1032. [Google Scholar]
- DiBartola S.P., Rutgers H.C. Diseases of the kidney. Hydronephrosis. Sherding R.G. The Cat Diseases and Clinical Management, 2nd edn, 1994, Churchill Livingstone: New York, 1725–1727. [Google Scholar]
- Finco D.R. Obstructive uropathy and hydronephrosis. Osborne C.A., Finco D.R. Canine and Feline Nephrology and Urology, 1995, Williams & Wilkins: Philadelphia, 889–894. [Google Scholar]
- Klahr S., Morrissey J. Obstructive nephropathy and renal fibrosis, American Journal of Physiology. Renal Physiology 283, 2002, F861–F875. [DOI] [PubMed] [Google Scholar]
- North D.C. Hydronephrosis and hydroureter in a kitten – a case report, The Journal of Small Animal Practice 19 (4), 1978, 237–240. [DOI] [PubMed] [Google Scholar]
- Rawlings C.A., Bjorling D.E., Christie B.A. Kidneys. Nephrectomy/hydronephrosis. Slatter D. Textbook of Small Animal Surgery, 3rd edn, 2002, Saunders: Philadelphia, 1608–1609/pp. 1614–1615. [Google Scholar]
- Rivers B.J., Walter P.A., Polzin D.J. Ultrasonographic-guided, percutaneous antegrade pyelography: technique and clinical application in the dog and cat, Journal of the American Animal Hospital Association 33 (1), 1997, 61–68. [DOI] [PubMed] [Google Scholar]