Abstract
Background:
Anxiety, a common symptom of Parkinson’s disease (PD), results in reduced life quality, reduced participation in meaningful roles and daily activities, and increased health burden. There are no evidence-based interventions to reduce the impact of anxiety in PD on participation.
Objective:
This study aimed to identify the key components required for the co-production of an occupation- and community-based intervention for people with PD-related anxiety.
Methods:
A participatory mixed-methods research study was conducted using online Group Concept Mapping methodology that included five stages: brainstorming, idea synthesis, sorting activity, rating activity, and analysis. A cluster map, pattern match, and ‘go-zone’ charts were created through multivariate statistical analysis based on participants’ responses. The stages were guided by questions generated by the research team working with stakeholders.
Results:
Eighty-three people participated, with 64 taking part in more than one activity. Participants included people with PD (n = 72), care partners (n = 6), and occupational therapists (n = 5). The final map contained 119 statements with eight clusters (stress value 0.252): exercise, lifestyle changes, self-help, coping, access to information, professional help, peers and groups, support from others. Significant agreement existed between the importance and feasibility rating activities (r = –0.07). ‘Go-zone’ charts highlighted the priority statements for intervention development.
Conclusions:
This novel participatory study highlighted priority components that provide starting points for future development of an occupation- and community-based intervention for people with PD-related anxiety.
Keywords: Parkinson’s disease, anxiety, occupational therapy, intervention development
INTRODUCTION
Parkinson’s disease (PD) is the second-most common neurodegenerative condition in the UK, affecting approximately 145,000 people [1]. In addition to the cardinal motor symptoms of bradykinesia, rigidity, and tremor, PD also results in a wide range of sensory, cognitive, and psychological non-motor symptoms [2]. These can cause significant disability, interfere with participation in everyday roles and activities, and reduce quality of life [2, 3].
Anxiety is a non-motor symptom that affects around 40–56% of people with PD [4]. People with PD fall more than age-matched controls, and risk factors for falling include fear of falling, which is influenced by anxiety [5, 6]. Reviews indicate no effective pharmacological interventions to reduce anxiety in people with PD [4]. Psychological interventions for anxiety in non-Parkinsonian populations, recommended in the UK as part of NICE guidelines and the Improving Access to Psychological Therapies (IAPTs) programme [7, 8], are cost-effective and have long-term financial and health benefits [9]. However, evidence for the effectiveness of mindfulness and cognitive behavioral therapy approaches is limited and inconclusive in people with PD [10–13]. Additional approaches are also warranted, given the shortage of clinical psychologists in the UK [14] and the central role of restricted participation in contributing to increased chronic anxiety [15, 16].
People with PD have expressed a desire for an intervention aimed at living well with the complex experience of anxiety with PD, focused on ‘doing’ (i.e., participation in meaningful occupation) as both a means and a goal of intervention rather than only talking about thoughts and feelings [17, 18]. With their dual training in physical and mental health and expertise in improving wellbeing through participation, occupational therapists are in an ideal position to support people with PD experiencing anxiety [19].
Occupational therapy focuses primarily on enabling participation in a person’s chosen meaningful roles and activities, such as getting dressed, cooking a family dinner, or playing the piano in a jazz band [20]. Access to occupational therapy is recommended in clinical guidelines to support symptom management, promote independence, and reduce hospital admissions [21]. Research suggests that occupational therapy focused on the person’s prioritized meaningful goals in activities in daily living and participation is an effective intervention for people with PD [22, 23]. No identified best-practice occupational therapy intervention exists for people with PD with anxiety-related participation problems.
With a high prevalence of anxiety in people with PD, but little research into its management, it is essential to establish a sound scientific basis for developing an intervention based on the Medical Research Council’s guidance for complex interventions [24]. As a first step in intervention development, this study involved all stakeholders as a precursor to a logic modeling process. It aimed to identify the components needed to co-produce a new occupation-based intervention to help people with PD live well with anxiety.
METHODS
Study design
Consensus methods, such as nominal group technique and the Delphi methodology, are commonly used to generate and/or validate the components of a health intervention [25]. However, these approaches struggle to engage diverse groups, particularly rarely heard groups [26]. In contrast, Group Concept Mapping (GCM):
“(1) generates group wisdom by creating consensus on key ideas and supports systems thinking by eliciting individual experiences to identify group conceptualization of an issue; (2) equalizes or lessens power differentials among participants; (3) engages patients as both study participants and collaborative decision makers throughout the research process; and (4) includes the availability of specific web-based software to engage participants, provide project management, and generate concept maps.” [26, page 2]
Therefore, GCM was used to identify the components needed for a new occupation-based complex intervention. It involved qualitative and quantitative methods in a structured, sequential process to organize the ideas of a group about a topic— people with PD living well with anxiety— and involved brainstorming, sorting, and rating (qualitative processes) combined with multivariate statistical analysis (quantitative) [27]. These ideas are then visually represented using two-dimensional concept maps [27]. This versatile method can be implemented in paper form or using a secure online platform called ‘Groupwisdomtrademark’ [28], enabling participants to contribute at their convenience [26].
Ethical approval was secured from the University of Plymouth Faculty of Health Staff Research Ethics and Integrity Committee (Reference 2473).
Participants and recruitment
Sample size in GCM studies varies depending on the question and data collection method [29]. The recruitment target of n = 40 was based on previous studies that have reported attrition of 10% between the GCM stages and reaching data saturation in stage 5 [29–31]. The sample was divided into three groups— people with PD, care partners, and occupational therapists (13–14 participants per group)— to avoid potential power differences between group participants. Occupational therapists were included based on feedback from patient and public involvement (PPI) stakeholders who contributed to the study design and felt that it was important to include therapists’ perspectives. Twelve weeks were allocated for recruitment.
Purposive sampling was used and was targeted to ensure a diverse range of respondents— recruitment materials targeted age (for all groups) and diagnosis duration (for people with PD). Inclusion criteria for our target sample were people with PD with a formal diagnosis of PD with self-reported PD-related anxiety, any care partner of a person with PD-related anxiety, and occupational therapists working with people with PD or with expertise in working with people with anxiety. Formal assessment of anxiety status was not used to avoid missing rich experiential data.
People with PD and care partners were recruited via the Parkinson’s UK Research Support Network and the Peninsula Parkinson’s Research Interest Group (PenPRIG). Occupational therapists were recruited via the Royal College of Occupational Therapists specialist sections for neurological practice (SSNP) and mental health (SSMH). A member of each organization acted as a gatekeeper and sent out email advertisements to their distribution lists. The gatekeeper protected the autonomy of prospective participants and allowed them to decide freely whether they wished to participate. The email invitations included a copy of the participant information sheet and the lead researcher’s (CL) contact details. Interested participants contacted the lead researcher, who answered any questions presented and then sent a weblink to ‘Groupwisdomtrademark’, which required participants to complete an informed consent form.
Participants were asked to engage in three out of five stages of the GCM: brainstorming, sorting, and rating (see below). Each stage was open for two to four weeks; an invitation and two email reminders were sent to participants at each stage.
Data collection
There were five specific stages: brainstorming ideas in response to the focus prompt, using open text (stage 1), idea synthesis by the research team (stage 2), participants sorting the brainstormed statements into groups that made sense to them (stage 3), participants rating each statement on its importance and feasibility (stage 4), and data analysis (stage 5) [27]. Participants could access ‘Groupwisdomtrademark’ at a convenient time and place during each stage and contribute as much data as they wished; no data limiters were used. Participants initially provided demographic information, including their role in the research (i.e., if they were a person with PD, care partner, or occupational therapist), gender, age, and how long they had been diagnosed with PD (if appropriate).
Stage 1: Brainstorming
Participants were asked to generate statements based on their thoughts and experiences in response to the focus prompt “one thing that would help a person with Parkinson’s to live well with anxiety might be . . . ”. There was a two-week window for participants to complete the brainstorming stage.
Stage 2: Idea Synthesis
The list of the participants’ raw statements was exported to a spreadsheet, interrogated, and edited for grammar and readability without changing the wording. Statements expressing multiple ideas were split into single-idea statements; these were the only edits performed. All statements were assigned a keyword generated from the participants’ language to express their meaning. Statements with similar keywords were scrutinized together, and duplicates were removed. The result was a final set of refined, unique statements for use in the later stages [27].
Stage 3: Sorting Activity
Each statement in the final set was assigned a number and listed in random order on the ‘Groupwisdomtrademark’ software. Each participant was asked to sort statements into groups that were meaningful to them by dragging and dropping them onto a blank workspace in the software. Participants were also asked to give each group a relevant name. For the data to be approved for further analysis, participants must have sorted≥75% of the statements into meaningful themes [27].
Stage 4: Rating Activity
Stage 4 ran simultaneously with stage 3 to reduce participant time burden. They were asked to rate each idea on a five-point ordinal scale for importance and feasibility to facilitate the identification of priority items. Importance ranged from 1 (‘not at all important’) to 5 (‘very important’), and feasibility from 1 (‘not realistic at all’) to 5 (‘very realistic’). Participants were asked to rate each statement with all the others to ensure that the full range of the scale was used. Similar rating questions have been used in other GCM studies [32]. Both activities were closed after three weeks.
Stage 5: Analysis
Qualitative and quantitative techniques were used to analyze the data. The ‘GroupwisdomTM’ software combined the sorted data into a similarity matrix, showing each statement as a position on an X-Y axis indicating how participants sorted statements. The similarity matrix produced a two-dimensional point map using a multidimensional scaling process. The closer points represented statements that were more often grouped together because the participants thought they were conceptually similar [27]. The software generated a stress value that indicated the degree to which the distances between each point on the map were representative of the sorting data. Lower stress values suggest greater stability and goodness-of-fit. Stress values below 0.365 are desirable for GCM research studies [27, 31].
Hierarchical cluster analysis was applied to the data using Ward’s method to group statements with similar meanings into clusters representing how participants grouped their ideas [33]. This statistical technique was performed in the ‘GroupwisdomTM’ software and involves drawing boundaries onto the point map to produce a cluster map. Clusters are successively merged, resulting in several viable cluster maps. A final cluster ‘solution’ is then selected through qualitative interpretative analysis [27]. In this research study, the first author (CL) consulted with the rest of the research team (KB, JM, IS) to evaluate maps of six to nine clusters to determine the final cluster solution. This process involved checking whether the statements within each cluster represented the overall theme and comparing the cluster maps to each other to check for similarities and discrepancies between cluster statements and titles.
Cluster labels were suggested by the software for the final cluster solution based on the verbatim statements made by the participants during the sorting activity. The research team refined the cluster labels for grammar and readability, but the wording was unchanged.
The rated data were then organized into a pattern match as a visual representation of the data. This allowed comparison of each cluster’s mean importance and feasibility [27] and helped highlight priority themes for future intervention development. Individual go-zone graphs were created for each cluster, indicating which statements within the cluster were the most important and feasible. Go-zones are bivariate graphs divided into four quadrants by the mean scores generated for importance and feasibility [27]. The upper right quadrant contained the statements that scored above the mean for importance and feasibility. Statements in the ‘go-zone’ were considered priority statements for intervention development (Supplementary Table 1). These visual representations of the data are intended to aid in the appraisal and subsequent use of the results in a future intervention development study.
Rigor and validity
The participatory approach of the GCM methodology promoted both the credibility and real-world applicability of the findings by ensuring that the results directly represented the participants’ experiences and ideas. A senior researcher (KB) peer-reviewed the cluster map to ensure that the headings represented the participants’ language.
RESULTS
Study population
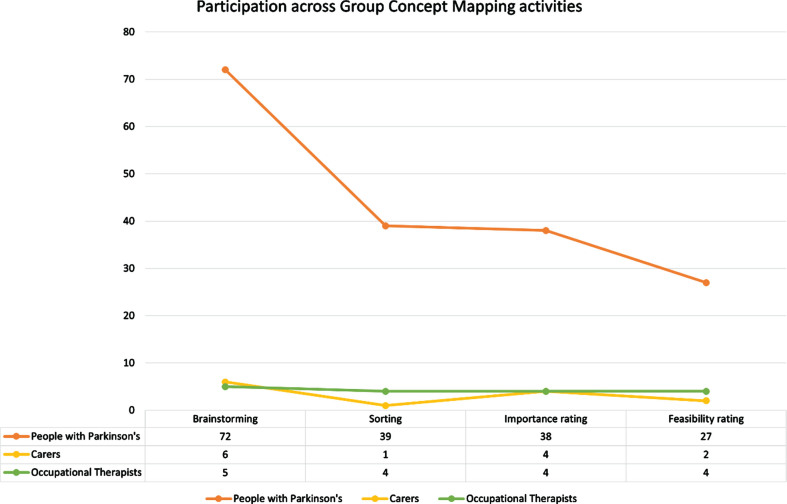
The final sample consisted of 83 who participated in at least one activity and 64 who participated in more than one activity. The final sample was predominantly female. The recruitment target for people with PD was exceeded (n = 72). The care partner (n = 6) and occupational therapist (n = 5) groups were under-recruited. There was attrition between the study phases (Fig. 1) with 38% (n = 27) of people with PD, 33% (n = 2) of care partners, and 80% (n = 4) participating in the final phase.
Fig. 1.
Line graph summarizing participation across each GCM activity.
Figure 1 shows how many participants from each sample group took part in each activity. During brainstorming, participants provided 198 ideas in response to the focus prompt, which were synthesized into a list of 119 unique statements (Supplementary Table 1). One participant’s sorting data was rejected because less than 75% of statements were sorted. Forty-four data sets from the sorting activity were approved for analysis. From the rating activity, one participant’s feasibility rating data set was rejected due to rating less than 75% of the statements, with 33 approved for analysis.
Because the participants used the ‘GroupwisdomTM’ software at different times for the activities open for specified periods, some participants skipped, did not have the opportunity, or chose not to answer the demographic questions (n = 12). Participant characteristics of respondents to demographic questions are shown in Table 1.
Table 1.
Participant characteristics of respondents to demographic questions
| Characteristic | All participants | People with | Care Partners | Occupational | |
| (n = 83) | Parkinson’s (n = 72) | (n = 6) | Therapists (n = 5) | ||
| Gender | Male | 34 (41%) | 32 (44%) | 1 (17%) | 1 (20%) |
| Female | 46 (55%) | 37 (52%) | 5 (83%) | 4 (80%) | |
| Other (including transgender) | 3 (4%) | 3 (4%) | 0 | 0 | |
| 35–44* y | 3 (4%) | 1 (1%) | 0 | 2 (40%) | |
| 45–64 y | 34 (41%) | 28 (39%) | 3 (51%) | 3 (60%) | |
| 65–74 y | 34 (41%) | 33 (46%) | 1 (17%) | 0 | |
| 75+ | 12 (14%) | 10 (14%) | 2 (34%) | 0 | |
| Median years PD diagnosis duration (range) | n/a | 5 (1.0–21.0) | n/a | n/a |
*No participants younger than this were involved in the study.
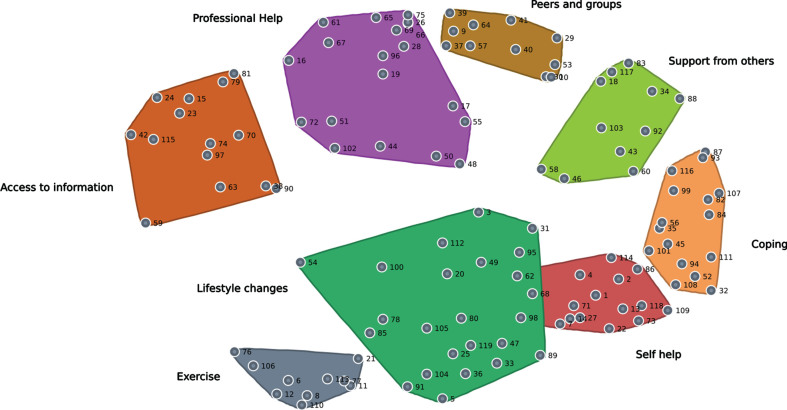
Concept map
Multidimensional scaling of the data from all participant groups resulted in a point map with a stress value of 0.252. This score indicates the goodness of fit of the sorting data, i.e., the sample data are likely to represent the data that would be expected in the actual population [34]. After the hierarchical cluster analysis, several cluster maps were generated and reviewed by the research team and a patient and public involvement (PPI) representative. Consensus was reached on an eight-cluster solution with the following cluster names taken directly from the participants’ contributions: Access to information, Professional help, Peers and groups, Support from others, Coping, Self-help, Lifestyle changes, and Exercise. The cluster map is shown in Fig. 2. A point on the map represents each numbered statement (see Supplementary Table 1).
Fig. 2.
Cluster map showing eight priority themes for intervention development. The map shows the distribution of each statement as a numbered point.
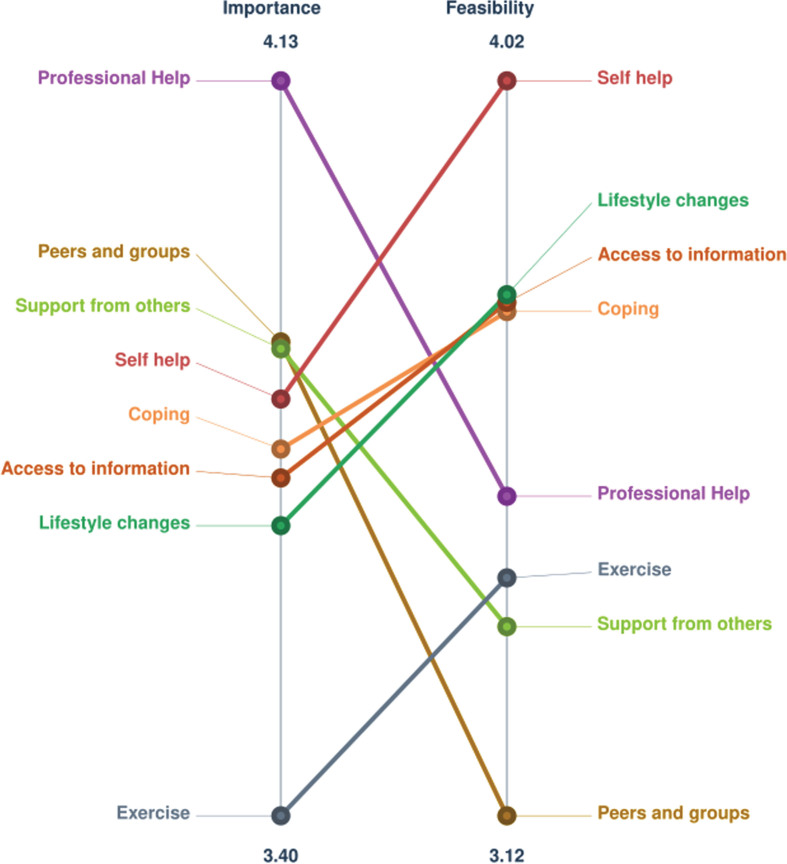
Pattern match
A pattern match compares the eight clusters’ mean rating scores for importance and feasibility (Fig. 3). The clusters are ranked along the vertical lines representing importance (left) and feasibility (right). The pattern match shows that three clusters were rated higher for importance than feasibility (Professional Help, Peers and groups, Support from others). The remaining clusters were rated higher for feasibility than importance (Self-help, Lifestyle changes, Access to information, Coping, Exercise). The overall correlation between the two rating patterns shows no to negligible relationship between importance and feasibility ratings across clusters (r = –0.07).
Fig. 3.
Pattern match comparing the mean importance and feasibility rating scores at the cluster level (upper limit = 5). Higher mean scores are closer to the pattern match’s top (r = –0.07). Importance (n = 46); feasibility (n = 33).
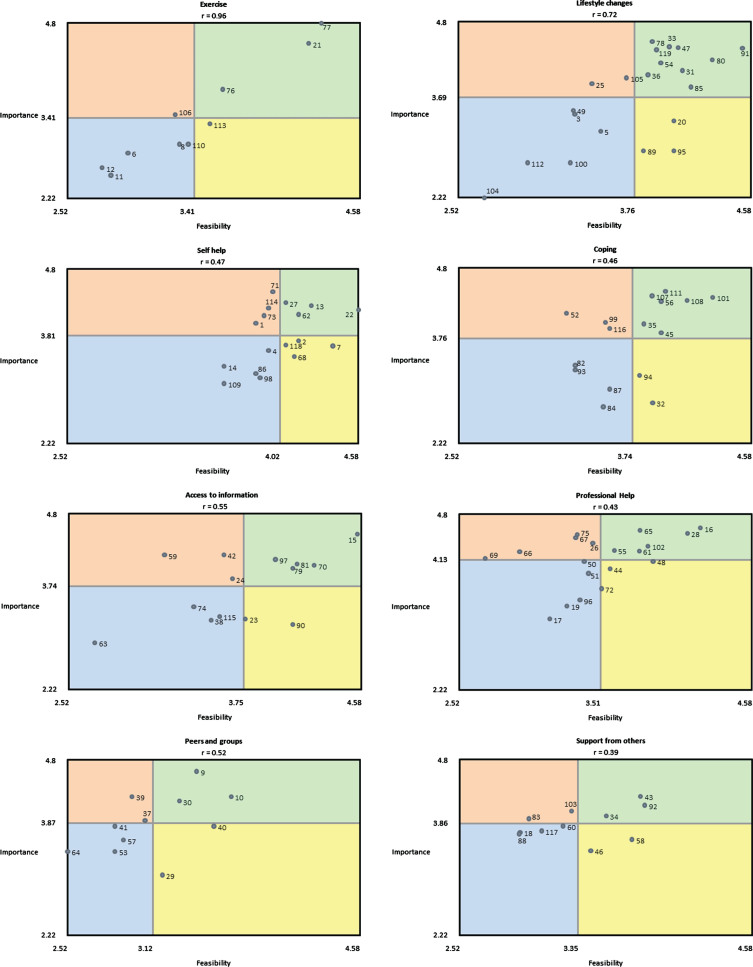
Go-zone graphs and statements
Go-zone graphs that were generated for each cluster are presented in Fig. 4. Statements in the go-zones are identified as actionable priorities. Those with high importance and high feasibility were of particular interest, as they are considered priority themes for intervention development. Those with high importance but slightly lower feasibility are areas for future intervention development but are not immediate priorities.
Fig. 4.
Go-zone plots for each of the eight clusters. Statements are shown as numbered points (see Supplementary Table 1). The upper right quadrant of each plot represents statements considered priorities for intervention development. The upper left quadrant represents areas for future development. Importance (n = 46); feasibility (n = 33).
The eight clusters represent a common understanding among participants of the key components for future intervention development.
“Professional help”
This cluster was rated as the most important (Fig. 3). There are 18 statements in this cluster. A common theme within this cluster is increasing clinicians’ condition-specific knowledge, such as:
“Understanding how PD anxiety is different from other anxiety.” (Statement 102)
Participants felt it was important and feasible for clinicians to understand anxiety in PD, which is consistent with previous research on clinical expertise in care teams and observational data [35].
“Peers and groups”
This cluster was ranked second for importance but last for feasibility (Fig. 3) and consists of 11 statements. Access to people and groups with experience of PD-related anxiety was a common theme:
“A matched and paired “Buddy” to discuss developments with.” (Statement 57)
“Having a structured support network with a list of who is responsible for what.” (Statement 40)
“Support from others”
While superficially like the previous cluster, the 11 statements in this cluster highlight the specific qualities that people with PD would like to see people, in their social context, exhibit to support them in their anxiety:
“Encouragement to share anxiety with partners and close friends.” (Statement 92)
“One to one support to improve self-confidence.” (Statement 18)
The participants identified this cluster as important and feasible (Fig. 3), which suggests that educating people in their social context about people with PD living with anxiety should be a core component of the intervention.
“Self help”
The 17 statements in this cluster relate to ways in which people with PD can help themselves to manage their anxiety so that they can live well with anxiety and PD. This cluster was rated fourth in importance and first in feasibility (Fig. 3), suggesting that the intervention should include a substantial self-help component in order to:
“To simplify your life.” (Statement 1)
“Exploring different ways to relax.” (Statement 13)
Relaxation techniques that are easy and quick to implement were identified in the go-zone. These findings suggest that relaxation techniques commonly used for anxiety (e.g., box breathing exercises) should be central to the new intervention [36].
“Coping”
The concept of coping as a strategy for reducing the unpleasant feelings associated with anxiety is embodied in this cluster. The 16 statements in this cluster focused on coping with the emotional impact of anxiety, for example:
“Finding out what triggers your anxiety.” (Statement 107)
“Accepting my condition rather than being frustrated by what I can’t do.” (Statement 111)
Addressing these pressures may provide a viable method of coping with anxiety for people with PD. Several statements in this cluster (statements 45, 108, 111) highlight learning to accept living with a long-term incurable illness as an important and feasible component of the proposed intervention (Fig. 3).
“Access to information”
Statements in this cluster relate to people with PD not only having access to information about their condition when they need it but also being educated about the condition that they are living with, for example:
“Access to up to date research.” (Statement 79)
“Better information and support regarding the later stages of Parkinson’s disease.” (Statement 81)
Statements in this cluster suggest the provision of written information as important and feasible (Fig. 4).
“Lifestyle changes”
This cluster ranked seventh in importance and second in feasibility (Fig. 3) and contains 21 statements. The importance of engaging in meaningful activities coupled with lifestyle adjustments (such as improving diet and increasing physical activity) to manage anxiety is woven throughout the cluster, for example:
“Maintaining social interests e.g. sports.” (Statement 78)
“Having a balanced diet.” (Statement 80)
“Exercise”
The 10 statements in this cluster relate to physical exercise such as dancing (statement 6), yoga (statement 113), and tai chi (statement 8). However, exercise was rated the least important and sixth most feasible for an intervention to support people with PD with anxiety (Fig. 3).
DISCUSSION
It could be argued that all clusters generated in this study are essential components of the new intervention, as no clusters or individual statements were rated lower than 3 (slightly important) on importance. The inclusion of feasibility ratings, therefore, highlighted clusters that should be targeted as a priority. Participation in meaningful roles and activities is included in several clusters (“Exercise”, “Lifestyle changes”, “Self help”) but not in clusters such as “Coping” and “Support from others”. These clusters highlight broader individual and social factors that support participation in meaningful occupation and will need to be considered in intervention development.
“Professional Help” was rated as the most important cluster by participants. People with PD identify a lack of understanding among professionals about PD and PD-related anxiety as a barrier to quality healthcare, which has been reflected in national campaigns in the UK [1, 37]. This reinforces the notion that there is still much work to be done in this area and that clinician training in PD will be critical to the success of the new intervention. Improving clinicians’ understanding of PD-related anxiety would likely strengthen a positive therapeutic relationship [38]. Establishing positive relationships with healthcare providers, in this case occupational therapists, can support maintaining a degree of normality and identity for people with PD [37]. This improvement in the relationship with healthcare providers may also reduce the ‘treatment burden’ for people with PD by optimizing treatment to work toward individual goals and minimize disruptions [39]. This is consistent with research exploring patient-centered management of people with PD [40].
The cluster “Peers and groups” highlights that participants consider timely access to peer support important, consistent with research exploring patient-centered management of PD [40]. Peer support can enhance social connectedness and help people with PD lead meaningful and satisfying lives. This is reflected in research exploring the lived experience of anxiety in PD and will be an important consideration for the next stage of intervention development [17]. Other research has identified that people with PD value support from people who understand what triggers their problems [17, 18]. Fostering a ‘partnership’ between people with PD and their peers will help to create a safe environment for people with PD to share their experiences [17, 18]. This partnership approach has been used in other interventions for long-term conditions [41].
Peer support offers unique benefits from shared lived experiences [42]. Nevertheless, several potential barriers exist to accessing peer support [42]. This is possibly reflected in the participant’s low feasibility rating of the cluster. Similar findings were highlighted in the “Support from others” cluster. This cluster focuses on fostering partnerships with people without PD who understand the triggers of people with PD, which is consistent with studies highlighting the need for emotional support [43]. It will be important to explore how such barriers to accessing peer support and support from others can be mitigated for individuals developing a new intervention.
“Self help” and “Coping” were identified as separate clusters by participants but are closely related. This is evidenced by the physical proximity and similar size of the clusters on the map (Fig. 2) and similar importance ratings (Fig. 3). Both clusters include self-management statements. Self-management strategies are effective in PD, but many focus primarily on motor symptoms [44]. Although this may not seem applicable to a new intervention focusing on anxiety, several studies report that motor symptoms are closely related to anxiety in people with PD [17, 45]. Time pressure has been associated with increased anxiety, increased motor symptoms such as freezing of gait, and decreased quality of life in PD [3, 17]. Self-management techniques can provide a sense of empowerment through mechanisms such as participation in decision-making [46]. Including self-management techniques addressing anxiety related to motor symptoms, and vice versa, in a new intervention may be valuable. While people with PD have expressed that they do not want another psychological therapy, a new intervention based on a collaborative relationship with a healthcare professional may include psychological therapy concepts [17, 18]. Acceptance and commitment therapy is a form of psychotherapy that enables people to focus on the present moment and accept their thoughts and feelings without judgment; it can be included under the umbrella term ‘talking therapies’ [47]. This therapy has promising evidence of initial effectiveness in the self-management of long-term conditions, including PD, and provides an underlying concept for intervention development [47].
People with PD use fewer coping strategies than people with other long-term conditions [48, 49]. Many tend to use “self-control” [48, 49]. Women with PD tend to have more problem-focused coping strategies than men, but people with PD generally use both problem-focused and emotion-focused coping strategies [50]. In addition, cognitive impairments, common in PD, are associated with decreased use of task-related coping [51, 52]. Feelings of shame related to having PD can negatively affect coping and self-management and exacerbate anxiety symptoms [53]. Any new intervention will need to incorporate tailoring and individualization of treatment to account for these variations in coping strategies and the impact of cognitive impairment and emotional state [54].
Participants rated having “Access to information” as a feasible component to include in the new intervention. This is consistent with previous research highlighting this need for education [43, 55]. Disease-specific education interventions have evidenced improvement in the quality of life of people with PD, potentially through patient empowerment [56]. Ensuring that patient education is delivered in a way that is both culturally and individually specific will be crucial to the successful delivery of the intervention and will likely involve a range of media [57]. Any information provided in a new intervention will need to be concise, approachable, and non-threatening to promote engagement, particularly as people with PD report “wanting to know but not wanting to know” [58].
“Lifestyle changes” were similarly highlighted as feasible by participants, including maintaining social interests, engaging with hobbies, and integrating daily exercise and physical activity (Fig. 4). The value of using preventative lifestyle programs has been demonstrated to be a cost-effective way to improve health and wellbeing in myriad studies, including occupational therapy and provides a concept for future intervention [59]. Similar concepts have been used in other lifestyle management interventions [60, 61]. Participants also reported that maintaining a healthy diet is both important and feasible for living well with anxiety, which was also reported in other studies [61, 62]. This links closely with the cluster “Exercise”.
Exercise was rated the least important and sixth most feasible for an intervention supporting people with anxiety with PD (Fig. 3). As previously discussed, this may reflect a lack of understanding and education about PD. Exercise is an evidence-based intervention in PD that has demonstrated benefits on the motor symptoms of PD, but there is only emerging evidence on the effect on non-motor symptoms such as anxiety [63]. Exercise has been shown to decrease anxiety in people with PD and is not restricted to a specific type of exercise [64, 65]. Despite this, many barriers prevent sustained engagement in exercise and physical activity despite people with PD recognizing its importance [66]. Given the benefits of exercise on quality of life and anxiety in non-Parkinsonian populations, incorporating regular exercise into the daily routine may be a helpful component of the new intervention [67]. The new intervention will likely need to integrate these wider lifestyle components to promote sustained engagement in meaningful roles and activities to promote living well with anxiety.
In the next stage of intervention development, we will consider to what extent and in what way the key components can be included in a community- and occupation-based occupational therapy intervention. This will require a suitable method to meaningfully involve stakeholders (people with PD, care partners, and occupational therapists) in a co-production process.
Strengths and limitations
A strength of the GCM methodology is its structured and systematic procedure for data collection that places the voice of the participants, most of whom were people with PD with anxiety, at the center. The eight clusters portray what the participants feel is important to include in a new intervention to help people with PD live well with anxiety. In addition, the large number of statements suggests a range of thoughts among the participants, not just those of dominant group members. Online delivery using the ‘GroupwisdomTM’ platform allowed participants to contribute to the study at their convenience, thus facilitating participation.
This study is not without limitations. The sample size exceeded our target (n = 40) and was heavily weighted towards people with PD (n = 72). Attrition occurred despite the research team’s efforts to maintain study participation, such as automated email and text message reminders when requested by participants. This likely resulted in additional attrition bias that skewed the results and compromised the study’s external validity.
Anxiety tends to occur earlier in PD and may be an early symptom of neurodegeneration [68]. This is reflected in the average disease duration of the participants (median 5 years). Evidence suggests that people living with young-onset PD (YOPD, diagnosed before 50 years) are more likely to experience anxiety than people with a late-onset of the disease [69]. It would be reasonable to expect this to be reflected in the characteristics of the participants. However, we can only be confident that 1% of participants with PD meet the YOPD criterion (Table 1). The next age group (45–64) accounted for 39% of the sample. As these age groups are based on the UK census, we cannot determine how many participants would be considered YOPD. Although our sample would still represent those aged 65 and above (60%), it would be helpful to use adjusted age groups in future research to distinguish between early and late-onset PD.
Small numbers of care partners and occupational therapists participated compared to people with PD. Thus, we cannot be confident that our findings represent all the groups included in this GCM study as they are likely weighted towards the views and experiences of people with PD. The under-recruitment in both care partner and occupational therapist groups may partly be attributed to the COVID-19 pandemic, which has had a noted impact on non-COVID-19 research due to increased service demands [70, 71]. Our sample was predominantly female, including for the group of people with PD. This finding was unexpected, particularly as PD tends to be more prevalent in men and men are over-represented in most research [72]. Resultantly, our findings may not fully represent the views of male people with PD, care partners, or occupational therapists. Future research will likely need to change its recruitment strategy and sampling frame to address this imbalance.
Moreover, GCM does not claim to be a definitive methodology, so studies using different methods may be needed. Although accounted for in the design of this study and the GCM methodology, the loss of participants between stages means that potential data was lost. Finally, we only collected basic demographic data to identify gender, age, and diagnosis duration (if applicable). As we lack data on areas such as cultural background and socioeconomic status, we cannot be confident any one group was not over-represented, limiting the external validity of this study to the UK population, including those from seldom-heard groups.
While digital delivery provided a convenient means of conducting this research, the impact on potential participant engagement in this study cannot be ignored, as it is likely that those who are less digitally literate will not have participated [73].
Future research directions
The findings highlight eight priority components, presented as clusters, for consideration in the future intervention. Individual ideas from within the clusters rated highly on importance and feasibility are suggested as starting points for future intervention development. Clusters, such as “Coping” and “Support from others”, highlight broader individual and social factors that support participation in meaningful roles and activities and need to be considered in intervention development. The ability to access timely support from peers and the development of individual coping strategies will be important considerations for the next stage of intervention development [17]. Future research, such as co-producing the intervention with stakeholders, is needed to integrate the components identified in this study into a new intervention to help people with PD to live well with anxiety. Future studies should seek to remove barriers to research participation for care partners and occupational therapists, as providing convenient data collection is unlikely to be sufficient.
Conclusion
This novel participatory study used an online GCM methodology to ask people with PD, care partners, and occupational therapists to highlight priority components that provide starting points for the future development of an occupation- and community-based intervention for people with PD-related anxiety. The eight clusters identified in the findings are exercise, lifestyle changes, self-help, coping, access to information, professional help, peers and groups, and support from others. Statements in each cluster rated highly on importance and feasibility will be prioritized in intervention development. We plan to use these findings to co-produce an occupation-based intervention for living well with anxiety in PD.
Supplementary Material
ACKNOWLEDGMENTS
We thank the people with PD, care partners, and occupational therapists who participated in this study for their invaluable contribution to this important work. In addition, we also thank our patient and public involvement and engagement contributors for helping shape this research study’s design.
SUPPLEMENTARY MATERIAL
The supplementary material is available in the electronic version of this article: https://dx.doi.org/10.3233/JPD-230150.
FUNDING
NIHR Clinical Doctoral Research Fellowship (ID number NIHR301565) to Mr. Christopher J Lovegrove. Publication fees were funded as part of this grant.
Training in Group Concept Mapping using ‘GroupwisdomTM’ and the associated software fees was provided through a learning grant through the Royal Devon University Healthcare NHS Foundation Trust (Community Division) to Mr. Christopher J Lovegrove.
CONFLICT OF INTEREST
CL: Salary: Royal Devon University Healthcare NHS Foundation Trust. Nonexecutive board member: Cornerstone Housing. Grant funding: NIHR, Cure Parkinson’s Trust (travel grant).
IS: Salary: Radboud University Medical Center. Grant funding: RAPP project with grant received from ZonMw, Development of Expertiseplatform Parkinson & work with grant received from ParkinsonNL & Bike for Parkinson, Abbvie, Ellen Parkinson Project, COPIED study with grant from Parkinson Vereniging.
JM: Salary: University of Plymouth. Commercial: Commercial study with Roche Hoffman limited investigating the validity of a phone-based app in people with Multiple Sclerosis. Grant funding: 2018–2022 A novel interactive training device to improve walking Ability and quality of life for Children with CErebral Palsy Trial (ACCEPT study): A multi-centred feasibility RCT with an embedded qualitative study Personal NIHR fellowship for Rachel Rapson £354,245. 1st supervisor B Kent UoP lead, Jon Marsden Co-applicant: Tulong, Ugnayan ng Lingap At gabaY (TULAY): Designing Community Physical Rehabilitation in the Philippines. NIHR £1,600,000 2023–2027. P Taylor Salisbury FES centre lead, Jon Marsden Co-applicant. The Efficacy of Peroneal Nerve Functional Electrical Stimulation (FES) for the Reduction of Bradykinesia in Parkinson’s Disease: An Assessor Blinded Randomised Controlled Trial (STEPS II). NIHR £1,500,000, 2022–2027
KB: Salary: Glasgow Caledonian University. Royalties & fee: Elsevier. Honorarium PhD Examination: Wrexham Glyndŵr University and Auckland University of Technology. Research assessor for Elizabeth Casson Fellowship.
The authors have no conflict of interest to report.
DATA AVAILABILITY
The data supporting the results of this study are available from the corresponding author upon reasonable request.
REFERENCES
- [1]. Parkinson’s UK (2014) Parkinson’s and You. https://s3-eu-west-1.amazonaws.com/puk-live-1-d8-ie/2017-03/Parkinson%27s%20and%20you.pdf, Accessed February 2022. [Google Scholar]
- [2]. Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386, 896–912. [DOI] [PubMed] [Google Scholar]
- [3]. Duncan GW, Khoo TK, Yarnall AJ, O’Brien JT, Coleman SY, Brooks DJ, Barker RA, Burn DJ (2014) Health-related quality of life in early Parkinson’s disease: The impact of nonmotor symptoms. Mov Disord 29, 195–202. [DOI] [PubMed] [Google Scholar]
- [4]. Pontone GM, Mills KA (2021) Optimal treatment of depression and anxiety in Parkinson’s disease. Am J Geriatr Psychiatry 29, 530–540. [DOI] [PubMed] [Google Scholar]
- [5]. Dissanayaka NN, White E, O’Sullivan JD, Marsh R, Pachana NA, Byrne GJ (2014) The clinical spectrum of anxiety in Parkinson’s disease. Mov Disord 29, 967–975. [DOI] [PubMed] [Google Scholar]
- [6]. Farombi TH, Owolabi MO, Ogunniyi A (2016) Falls and their associated risks in Parkinson’s disease patients in Nigeria. J Mov Disord 9, 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7]. National Collaborating Centre for Mental Health (2018) The Improving Access to Psychological Therapies Manual.
- [8]. National Institute for Health and Care Excellence (2011) Generalised anxiety disorder and panic disorder in adults: Management (NICE clinical guideline 113). [PubMed]
- [9]. Heuzenroeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, Andrews G, Vos T (2004) Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Aust N Z J Psychiatry 38, 602–612. [DOI] [PubMed] [Google Scholar]
- [10]. Biundo R, Weis L, Antonini A (2016) Cognitive decline in Parkinson’s disease: The complex picture. NPJ Parkinsons Dis 2, 16018–16018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11]. Hofmann S, Sawyer A, Witt A, Oh D (2010) The effect of mindfulness- based therapy on anxiety and depression: A meta-analytic review. J Consult Clin Psychol 78, 169–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Johnsen TJ, Friborg O (2015) The effects of cognitive behavioral therapy as an anti-depressive treatment is falling: A meta-analysis. Psychol Bull 141, 747–768. [DOI] [PubMed] [Google Scholar]
- [13]. McLean G, Lawrence M, Simpson R, Mercer SW (2017) Mindfulness-based stress reduction in Parkinson’s disease: A systematic review. BMC Neurol 17, 92–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14]. The King’s Fund (2015) Mental Health Under Pressure.
- [15]. Coventry PA, Dickens C, Todd C (2014) How does mental-physical multimorbidity express itself in lived time and space? A phenomenological analysis of encounters with depression and chronic physical illness. Soc Sci Med 118, 108–118. [DOI] [PubMed] [Google Scholar]
- [16]. CSDH (2008) Closing the gap in a generation: Health equity through action on the social determinants of health. Final Report of the Commission on Social Determinants of Health.
- [17]. Lovegrove CJ, Bannigan K (2021) What is the lived experience of anxiety for people with Parkinson’s? A phenomenological study. PLoS One 16, e0249390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Lovegrove CJ, Bannigan K, Cheeseman D, Latour JM (2017) The involvement of people with Parkinson’s in designing a study of the lived experience of anxiety. Br J Occup Ther 80, 494–501. [Google Scholar]
- [19]. Christine AM (1990) A philosophy unique to occupational therapy. Br J Occup Ther 53, 379–380. [Google Scholar]
- [20]. World Federation of Occupational Therapists (2019) About Occupational Therapy, https://www.wfot.org/aboutoccupational-therapy,
- [21]. National Institute for Health and Care Excellence (2018) Parkinson’s Disease Quality Standard. NICE guidelines (QS164).
- [22]. Radder DLM, Sturkenboom IH, van Nimwegen M, Keus SH, Bloem BR, de Vries NM (2016) Physical therapy and occupational therapy in Parkinson’s disease. Int J Neurosci 7454, 1–42. [DOI] [PubMed] [Google Scholar]
- [23]. Sturkenboom IH, Graff MJ, Hendriks JC, Veenhuizen Y, Munneke M, Bloem BR, Nijhuis-van der Sanden MW OTiP study group (2014) Efficacy of occupational therapy for patients with Parkinson’s disease: A randomised controlled trial. Lancet Neurol 13, 557–566. [DOI] [PubMed] [Google Scholar]
- [24]. Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, Boyd KA, Craig N, French DP, McIntosh E, Petticrew M, Rycroft-Malone J, White M, Moore L (2021) A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance.n. Br Med J 374, 2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25]. Cantrill JA, Sibbald B, Buetow S (1996) The Delphi and nominal group techniques in health services research. Int J Pharm Pract 4, 7. [Google Scholar]
- [26]. Cook K, Bergeron K (2019) Using group concept mapping to engage a hard-to-reach population in research: Young adults with life-limiting conditions. Int J Qual Methods 18, doi: 10.1177/1609406919891315. [DOI] [Google Scholar]
- [27]. Kane M, Trochim WM (2007) Concept Mapping for Planning and Evaluation. SAGE Publications, Inc., Thousand Oaks, CA.
- [28]. Concept Systems, Incorporated (2020) The Concept System® Global MAX™ (Build 2016.046.12) [Web-based Platform]. Ithaca, NY.
- [29]. Nielsen KT, Klokker L, Guidetti S, Waehrens EE (2018) Identifying, organizing and prioritizing ideas on how to enhance ADL ability. Scand J Occup Ther 26, 382–393. [DOI] [PubMed] [Google Scholar]
- [30]. Sjodahl Hammarlund C, Nilsson MH, Idvall M, Rosas SR, Hagell P (2014) Conceptualizing and prioritizing clinical trial outcomes from the perspectives of people with Parkinson’s disease versus health care professionals: A concept mapping study. Qual Life Res 23, 1687–1700. [DOI] [PubMed] [Google Scholar]
- [31]. Trochim WM, McLinden D (2017) Introduction to a special issue on concept mapping. Eval Program Plann 60, 166–175. [DOI] [PubMed] [Google Scholar]
- [32]. Murray-Mendes S, Martinez AR, Hackett KL (2021) Identifying occupational therapy research priorities in Trinidad and Tobago: A group concept mapping study. Occup Ther Int 2021, 9970566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33]. Ward JH (1963) Hierarchical grouping to optimize an objective function. J Am Stat Assoc 58, 236–244. [Google Scholar]
- [34]. Maydeu-Olivares A, Garcia-Forero C (2010) Goodness-of-fit testing. International Encyclopedia of Education 7, 190–196. [Google Scholar]
- [35]. Talebi AH, Ypinga JHL, De Vries NM, Nonnekes J, Munneke M, Bloem BR, Heskes T, Ben-Shlomo Y, Darweesh SKL (2023) Specialized versus generic allied health therapy and the risk of Parkinson’s disease complications. Mov Disord 38, 223–231. [DOI] [PubMed] [Google Scholar]
- [36]. Manzoni GM, Pagnini F, Castelnuovo G, Molinari E (2008) Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry 8, 41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37]. Read J, Cable S, Löfqvist C, Iwarsson S, Bartl G, Schrag A (2019) Experiences of health services and unmet care needs of people with late-stage Parkinson’s in England: A qualitative study. PLoS One 14, e0226916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38]. Horton A, Hebson G, Holman D (2021) A longitudinal study of the turning points and trajectories of therapeutic relationship development in occupational and physical therapy. BMC Health Serv Res 21, 97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39]. Tan QY, Roberts HC, Fraser SDS, Amar K, Ibrahim K (2023) What are the modifiable factors of treatment burden and capacity among people with Parkinson’s disease and their caregivers: A qualitative study. PLoS One 18, e0283713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40]. Bloem BR, Henderson EJ, Dorsey ER, Okun MS, Okubadejo N, Chan P, Andrejack J, Darweesh SKL, Munneke M (2020) Integrated and patient-centred management of Parkinson’s disease: A network model for reshaping chronic neurological care. Lancet Neurology 19, 623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41]. Apostol C, Cranwell K, Hitch D (2021) Evaluating a multidimensional strategy to improve the professional self-care of occupational therapists working with people with life limiting illness. BMC Palliat Care 20, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42]. Gerritzen EV, Lee AR, McDermott O, Coulson N, Orrell M (2022) Online peer support for people with Parkinson disease: Narrative synthesis systematic review. JMIR Aging 5, e35425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43]. Uebelacker LA, Epstein-Lubow G, Lewis T, Broughton MK, Friedman JH (2014) A survey of Parkinson’s disease patients: Most bothersome symptoms and coping preferences. J Parkinsons Dis 4, 717–723. [DOI] [PubMed] [Google Scholar]
- [44]. Milne-Ives M, Carroll C, Meinert E (2022) Self-management interventions for people with Parkinson disease: Scoping review. J Med Internet Res 24, e40181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45]. Blundell EK, Grover LE, Stott J, Schrag A (2023) The experience of anxiety for people with Parkinson’s disease. NPJ Parkinsons Dis 9, 75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46]. Kang E, Friz D, Lipsey K, Foster ER (2022) Empowerment in people with Parkinson’s disease: A scoping review and qualitative interview study. Patient Educ Couns 105, 3123–3133. [DOI] [PubMed] [Google Scholar]
- [47]. Graham CD, Gouick J, Krahé C, Gillanders D (2016) A systematic review of the use of Acceptance and Commitment Therapy (ACT) in chronic disease and long-term conditions. Clin Psychol Rev 46, 46–58. [DOI] [PubMed] [Google Scholar]
- [48]. Costa FP, Diaferia G, Behlau M (2016) Communicative aspects and coping strategies in patients with Parkinson’s disease. Codas 28, 46–52. [DOI] [PubMed] [Google Scholar]
- [49]. Pusswald G, Fleck M, Lehrner J, Haubenberger D, Weber G, Auff E (2012) The “Sense of Coherence” and the coping capacity of patients with Parkinson disease. Int Psychogeriatr 24, 1972–1979. [DOI] [PubMed] [Google Scholar]
- [50]. Anzaldi K, Shifren K (2019) Optimism, pessimism, coping, and depression: A study on individuals with Parkinson’s disease. Int J Aging Hum Dev 88, 231–249. [DOI] [PubMed] [Google Scholar]
- [51]. Hurt CS, Landau S, Burn DJ, Hindle JV, Samuel M, Wilson K, Brown RG (2012) Cognition, coping, and outcome in Parkinson’s disease. Int Psychogeriatr 24, 1656–1663. [DOI] [PubMed] [Google Scholar]
- [52]. Fang C, Lv L, Mao S, Dong H, Liu B (2020) Cognition deficits in Parkinson’s disease: Mechanisms and treatment. Parkinsons Dis 2020, 2076942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53]. Angulo J, Fleury V, Peron JA, Penzenstadler L, Zullino D, Krack P (2019) Shame in Parkinson’s disease: A review. J Parkinsons Dis 9, 489–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54]. Ambrosio L, Navarta-Sanchez MV, Portillo MC (2014) Living with Parkinson’s disease in the community: Improving assessments and interventions. Prim Health Care 24, 26–29. [Google Scholar]
- [55]. McLaughlin D, Hasson F, George Kernohan W, Waldron M, McLaughlin M, Cochrane B, Chambers H (2011) Living and coping with Parkinson’s disease: Perceptions of informal carers. Palliat Med 25, 177–182. [DOI] [PubMed] [Google Scholar]
- [56]. Rajan R, Brennan L, Bloem BR, Dahodwala N, Gardner J, Goldman JG, Grimes DA, Iansek R, Kovács N, McGinley J, Parashos SA, Piemonte MEP, Eggers C (2020) Integrated care in Parkinson’s disease: A systematic review and meta-analysis. Mov Disord 35, 1509–1531. [DOI] [PubMed] [Google Scholar]
- [57]. Friedman AJ, Cosby R, Boyko S, Hatton-Bauer J, Turnbull G (2011) Effective teaching strategies and methods of delivery for patient education: A systematic review and practice guideline recommendations. J Cancer Educ 26, 12–21. [DOI] [PubMed] [Google Scholar]
- [58]. Read J, Frost R, Walters K, Tuijt R, Manthorpe J, Maydon B, Pigott J, Schrag A, Davies N (2022) Transitions and challenges for people with Parkinson’s and their family members: A qualitative study.. PLoS One 17, e0268588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59]. Clark F, Jackson J, Carlson M, Chou C-P, Cherry BJ, Jordan-Marsh M, Knight BG, Mandel D, Blanchard J, Granger DA, Wilcox RR, Lai MY, White B, Hay J, Lam C, Marterella A, Azen SP (2012) Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: Results of the Well Elderly 2 Randomised Controlled Trial. J Epidemiol Community Health 66, 782–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60]. Forsyth A, Deane FP, Williams P (2015) A lifestyle intervention for primary care patients with depression and anxiety: A randomised controlled trial. Psychiatry Res 230, 537–544. [DOI] [PubMed] [Google Scholar]
- [61]. Piotrowski MC, Lunsford J, Gaynes BN (2021) Lifestyle psychiatry for depression and anxiety: Beyond diet and exercise. Lifestyle Med 2, e21. [Google Scholar]
- [62]. Pyatak EA, Carandang K, Rice Collins C, Carlson M (2022) Optimizing occupations, habits, and routines for health and well-being with Lifestyle Redesign(R): A synthesis and scoping review. Am J Occup Ther 76, 7605205050. [DOI] [PubMed] [Google Scholar]
- [63]. Ng SY-E, Chia NS-Y, Abbas MM, Saffari ES, Choi X, Heng DL, Xu Z, Tay K-Y, Au W-L, Tan E-K, Tan LC-S (2021) Physical activity improves anxiety and apathy in early Parkinson’s disease: A longitudinal follow-up study. Front Neurol 11, 625897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64]. Ferreira RM, Alves WMGdC, Lima TA, Alves TGG, Filho PAMA, Pimentel CP, Sousa EC, Cortinhas-Alves EA (2018) The effect of resistance training on the anxiety symptoms and quality of life in elderly people with Parkinson’s disease: A randomized controlled trial. Arq Neuropsiquiatr 76, 499–506. [DOI] [PubMed] [Google Scholar]
- [65]. Kwok JYY, Kwan JCY, Auyeung M, Mok VC, Lau CKY, Choi KC, Chan HYL (2019) Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with Parkinson disease. JAMA Neurol 76, 755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66]. Ellis T, Boudreau JK, DeAngelis TR, Brown LE, Cavanaugh JT, Earhart GM, Ford MP, Foreman KB, Dibble LE (2013) Barriers to exercise in people with Parkinson disease. Phys Ther 93, 628–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67]. Kandola A, Stubbs B (2020) Exercise and anxiety. In Physical Exercise for Human Health, Xiao J, ed. Springer Singapore, Singapore, pp. 345-352.
- [68]. Seritan AL, Rienas C, Duong T, Delucchi K, Ostrem JL (2019) Ages at onset of anxiety and depressive disorders in Parkinson’s disease. J Neuropsychiatry Clin Neurosci 31, 346–352. [DOI] [PubMed] [Google Scholar]
- [69]. Dissanayaka NN, Sellbach A, Matheson S, O’Sullivan JD, Silburn PA, Byrne GJ, Marsh R, Mellick GD (2010) Anxiety disorders in Parkinson’s disease: Prevalence and risk factors. Mov Disord 25, 838–845. [DOI] [PubMed] [Google Scholar]
- [70]. Bratan T, Aichinger H, Brkic N, Rueter J, Apfelbacher C, Boyer L, Loss J (2021) Impact of the COVID-19 pandemic on ongoing health research: An ad hoc survey among investigators in Germany. BMJ Open 11, e049086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71]. Park JJH, Mogg R, Smith GE, Nakimuli-Mpungu E, Jehan F, Rayner CR, Condo J, Decloedt EH, Nachega JB, Reis G, Mills EJ (2021) How COVID-19 has fundamentally changed clinical research in global health. Lancet Glob Health 9, e711–e720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72]. Baldereschi M, Di Carlo A, Rocca WA, Vanni P, Maggi S, Perissinotto E, Grigoletto F, Amaducci L, Inzitari D (2000) Parkinson’s disease and parkinsonism in a longitudinal study: Two-fold higher incidence in men. ILSA Working Group. Italian Longitudinal Study on Aging. Neurology 55, 1358–1363. [DOI] [PubMed] [Google Scholar]
- [73]. Office for National Statistics (2019) Exploring the UK’s digital divide. https://www.ons.gov.uk/peoplepopulationandcommunity/householdcharacteristics/homeinternetandsocialmediausage/articles/exploringtheuksdigitaldivide/2019-03-04
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data supporting the results of this study are available from the corresponding author upon reasonable request.