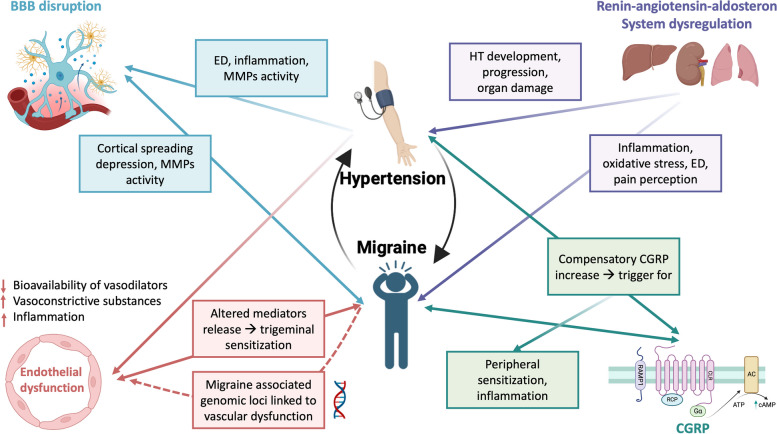
Fig. 1.
Possible pathophysiological mechanisms linking migraine and hypertension (HT). Endothelial dysfunction (ED) is a condition characterized by reduced vasodilator bioavailability, and a proinflammatory and procoagulant state. It may be a cause and a worsening factor of HT. ED is also associated with migraine but is still unclear whether it is a consequence or a cause of migraine attacks. Migraine-related genomic loci were found to be linked to vascular function. ED and MMPs activation could also lead to blood brain barrier disruption, with consequent neuroinflammation. These conditions are present in both HT and migraine patients, where MMPs activation could be determined by cortical spreading depression. RAAS dysregulation is associated with neurogenic inflammation, oxidative stress, ED and it is strictly related to HT development and progression. RAAS regulatory sites are expressed in areas involved in nociception and pain modulation, as the PAG, an endogenous analgesic network which is now considered as a possible migraine generator. CGRP is a key factor in migraine pathogenesis leading to peripheral sensitization. As a compensatory mechanism it was also found to be chronically elevated in HT patients, possibly triggering sensitization and inflammation in migraine. Abbreviations: BBB blood brain barrier, CGRP calcitonin gene related peptide, CSD: cortical spreading depression, ED endothelial dysfunction, HT hypertension, MMPs metalloproteinases, RAAS renin–angiotensin–aldosterone system. Created with biorender.com