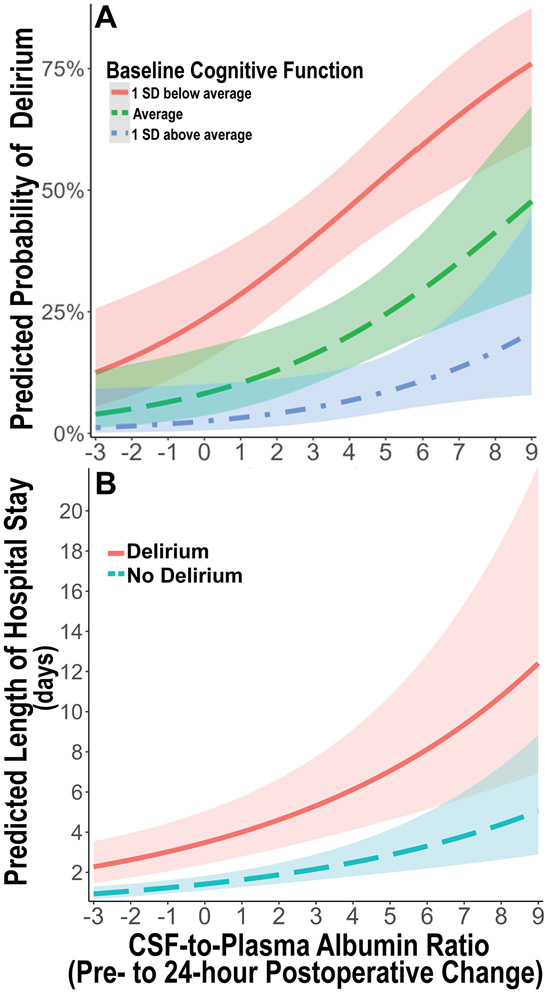
Figure 3: Predicted probability of postoperative delirium and hospital length of stay based on 24-hour change in cerebrospinal fluid-to-plasma ratio of albumin.
A. Predicted probability of postoperative delirium over the observed range of 24-hour postoperative cerebrospinal fluid-to-plasma ratio of albumin (CPAR) change according to baseline global cognitive function in our multivariable logistic regression model adjusted for age, baseline global cognitive function (continuous cognitive index), and surgery type. There is an additive dose-dependent association of increased 24-hour postoperative CPAR change with increased postoperative delirium rates, independent of baseline cognition. Baseline cognition is stratified as average (green ─ ─ ─), 1 standard deviation (SD) below average (red ───), and 1 SD above average (blue - ─ -). B. Predicted length of postoperative hospital length of stay over the observed range of 24 hour postoperative CPAR change according to postoperative delirium presence (red ───) or absence (blue ─ ─), in a multivariable negative binomial regression model adjusted for age, baseline global cognitive function, surgery type, and postoperative delirium status. Independent of postoperative delirium status, there is an additive dose-dependent association of increased 24-hour postoperative CPAR change with increased postoperative hospital length of stay. Shaded areas represent mean prediction error.