Abstract
Background.
Work is a social determinant of health that is often overlooked. There are major work-related differences in the risk of SARS-CoV-2 infection and death, but there have been few analyses of infection rates across industry groups. To date, only one national assessment of SARS-CoV-2 infection prevalence by industry based on self-report has been completed. No study has looked at seroprevalence of COVID-19 by industry.
Methods.
During May–December 2021, blood donors with SARS-CoV-2 anti-nucleocapsid testing were sent an electronic survey about their work. Free-text industry responses were classified using the North American Industry Classification System. We estimated seroprevalence and 95% confidence intervals (CIs) of SARS-CoV-2 infection by industry.
Results.
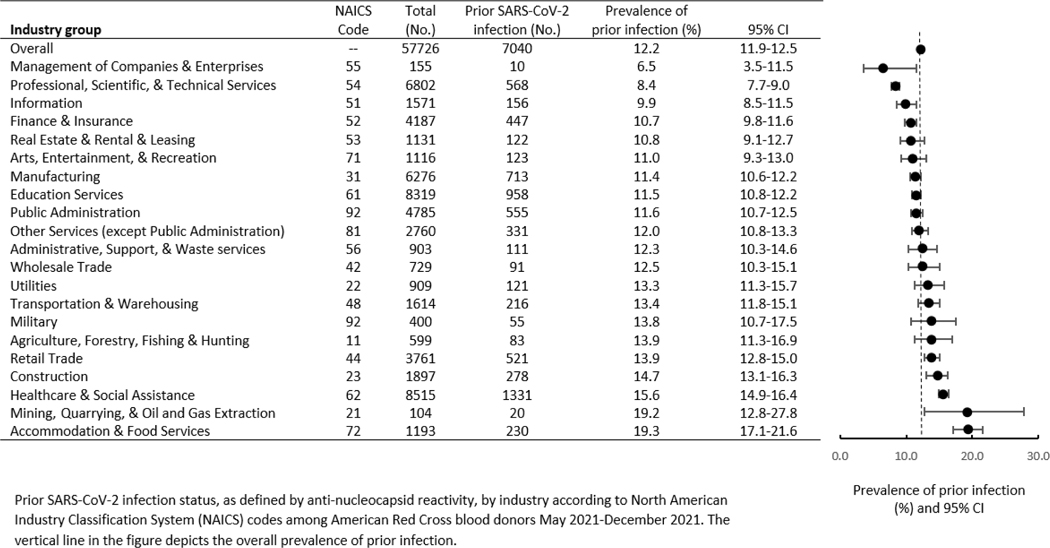
Of 57,726 donors, 7,040 (12%, 95% CI: 11.9%, 12.5%) had prior SARS-CoV-2 infection. Seroprevalence was highest among Accommodation & Food Services (19.3%, 95% CI: 17.1%, 21.6%), Mining, Quarrying, and Oil and Gas Extraction (19.2%, 95% CI: 12.8%, 27.8%), Healthcare & Social Assistance (15.6%, 95% CI: 14.9%, 16.4%), and Construction (14.7%, 95% CI: 13.1%, 16.3%). Seroprevalence was lowest among Management of Companies & Enterprises (6.5%, 95% CI: 3.5%, 11.5%), Professional Scientific & Technical Services (8.4%, 95% CI: 7.7%, 9.0%), and Information (9.9%, 95% CI: 8.5%, 11.5%).
Conclusions.
While workers in all industries had serologic evidence of SARS-CoV-2 infection, certain sectors were disproportionately impacted. Disease surveillance systems should routinely collect work characteristics so public health and industry leaders can address health disparities using sector-specific policies.
Keywords: COVID-19, SARS-CoV-2, seroprevalence, industry, work, blood donors
Introduction:
The World Health Organization declared the 2019 novel coronavirus (COVID-19) a public health emergency of international concern on January 30, 2020.1 By May 1, 2021, SARS-CoV-2 had infected over 32 million people in the United States and resulted in almost 600,000 deaths.2 To improve our ability to reduce the burden of COVID-19, we must understand how social determinants of health influence SARS-CoV-2 transmission and outcomes.3
Work is a social determinant of health that is often overlooked. There are major work-related differences in the risk of SARS-CoV-2 infection and death, but there have been few analyses of infection rates across industry groups.4,5 Industry is the type of business in which a person works while occupation is the kind of work a person does. Although industry differences in the risk of symptomatic COVID-19 and death among workers have been documented, 6–8 reports of infection rates by industry are lacking. In workplaces where people work near others, such as manufacturing, transportation, and education, clusters of COVID-19 were commonly reported.9 A higher risk was also found among healthcare workers and other public-facing worker groups.5,8,10 Individual states have published data on work-related incidence of COVID-19,11,12 and a national analysis reported seroprevalence of SARS-CoV-2 by occupation.13 To date, only one national assessment of SARS-CoV-2 infection prevalence by industry based on self-report has been completed.5 While informative, data on self-reported infections have limitations, including recall bias, incomplete testing, and inability to detect asymptomatic infections. No study has looked at seroprevalence of COVID-19 by industry. Examining industries can provide valuable insights alongside occupation-based analyses, as they encompass workers in various occupations who may share common risk factors for work-related infections. Here, we leverage infection-induced antibody testing and survey data from U.S. blood donors to estimate the seroprevalence of SARS-CoV-2 infection by industry. We aimed to identify industries that were disproportionately impacted and where sector-specific policies and tailored guidance may be warranted.
Methods:
A cohort of American Red Cross (ARC) blood donors received SARS-CoV-2 serological testing during May–December 2021.13 Blood donations underwent testing for anti-nucleocapsid (N) antibodies. Anti-N reactivity is a specific indicator of prior infection since existing vaccines do not contain nucleocapsid antigens. Anti-N reactivity was assessed with the Roche Elecsys anti-N assay (sensitivity, 100% (range, 88.3–100%); specificity, 99.8% (range, 99.7–99.9%)) or ORTHO anti-N assay (sensitivity, 90.0% (range, 80.8–95.1%); specificity, 99.1% (range, 98.4–99.5%)).14–17 An electronic survey was sent 2–6 weeks following blood donation to individuals aged ≥18 years who were accessible by email and spoke English. The survey included questions on employment status and work characteristics. Survey responses about industry were captured using free text. Responses were coded to 2012 North American Industry Classification System (NAICS) codes using the NIOSH Industry and Occupation Computerized Coding System and cross-walked to 2017 NAICS codes.18 Industry codes were analyzed using 2-digit sector groups.
Overall, 347,337 donors were eligible for the electronic survey, and 86,131 completed it (24.8% response rate). We excluded 145 discordant responses (survey answers about vaccination that did not match serological data); 24,483 donors who reported less than 30 days of paid employment since March 2020; 2,493 missing or uncodable industry responses; and 284 duplicate surveys. We estimated seroprevalence of prior SARS-CoV-2 infection and 95% confidence intervals (CIs) by industry. All analyses were conducted using R statistical software (version 4.0.3; R Foundation for Statistical Computing). The ARC institutional review board approved survey procedures (IRB 2020–015) with waiver of cosent. This study was also reviewed and approved by the author’s agency (0900f3eb81d52cce) and conducted consistent with applicable federal law.*
Results:
Overall, 57,726 blood donors were included in this analysis (Table). Healthcare & Social Assistance (n = 8,515) and Education Services (n = 8,319) sectors represented the largest number of participants. Few respondents worked in Mining, Quarrying, and Oil and Gas Extraction (n = 104) and Management of Companies and Enterprises (n = 155).
Table.
Seroprevalence of prior SARS-CoV-12 infection by industry group, U.S. Blood Donors, May 2021–December 2021
|
Of the 57,726 donors, 7,040 (12.2%, 95% CI: 11.9%, 12.5%) had antibody evidence of prior SARS-CoV-2 infection (Table). The highest seroprevalence occurred in Accommodation & Food Services (19.3%, 95% CI: 17.1%, 21.6%) followed by Mining, Quarrying, and Oil and Gas Extraction (19.2%, 95% CI: 12.8%, 27.8%), Healthcare & Social Assistance (15.6%, 95% CI: 14.9%, 16.4%), and Construction (14.7%, 95% CI: 13.1%, 16.3%). Sectors with the lowest seroprevalence included Management of Companies and Enterprises (6.5%, 95% CI: 3.5%, 11.5%), Professional Scientific & Technical Services (8.4%, 95% CI: 7.7%, 9.0%), and Information (9.9%, 95% CI: 8.5%, 11.5%).
Discussion
Although many epidemiologic studies on COVID-19 risk have focused on healthcare, education, and manufacturing workers, workers in all industry sectors are at risk of SARS-CoV-2 infection and COVID-19 disease. Seroprevalence by industry during May–December 2021 covered the end of the pre-Delta period (March 1, 2020–June 26, 2021) and the Delta period (June 27–December 18, 2021); providing a snapshot of working populations disproportionately affected by the first two waves of the pandemic.
Overall, our findings were consistent with those of previous studies despite different methodologies, samples, and time frames. Similar to previous studies, we report high frequency of SARS-CoV-2 infection among Accommodation & Food Services and Healthcare & Social Assistance workers. 5,9,11 We also found high seroprevalence among Mining, Quarrying, and Oil and Gas Extraction workers and Construction workers. The high seroprevalence of prior SARS-CoV-2 infections in the Construction industry is interesting given early focus and concern on more traditional indoor workplaces.19 However, the study period covered a time when COVID-19 vaccines were recommended for persons >12 years of age and were more widely available. Therefore, this finding may be related to vaccination uptake or other behaviors outside of the workplace. More work is needed to understand the most effective mitigation measures for preventing transmission among workers who work outdoors or in a combination of outdoor and indoor settings.
Discrepancies between our results and those of other studies discussed above may be from lack of standardization in the collection and reporting of work-related data among U.S. public health systems or difficulties in measuring and tracking SARS-CoV-2 infection rates, especially nationally. Work is an important social determinant of health3 and, as such, occupation and industry data should be included in public health surveillance systems. Discrepancies may also be due to differences in methodology. While we examined SARS-CoV-2 infection rates based on serological data, others relied on self-reported outcome data.5 This may explain why workers in Agriculture, Forestry, Fishing, and Hunting had lower prevalence in the previous study compared with our findings.
A strength of our study is the measurement of prior SARS-CoV-2 infection using serological data from participants across the United States. Limitations to this analysis also exist. The blood donor population may not be representative of the general U.S. working population or each industry group. It is also possible that the 25% of blood donors who participated differed from those who did not. Infection prevention measures, particularly for healthcare personnel, changed rapidly during the beginning of the pandemic so occupational risks for infection likely evolved over time. Because of the use of serologic data during a single period, this analysis could not account for the effects of mitigation changes over time. A proportion of individuals infected with SARS-CoV-2 may not develop anti-N antibodies, which may result in an underestimate of seroprevalence in our study. Serologic testing is a proxy for prior infection. Although waning of antibodies occurs, the assays selected for this study maintain high sensitivity in detecting infections more than 1 year prior to testing.15–17 Finally, this analysis cannot determine the source of infection or separate community from workplace transmission.
Considering the effect of risk factors such as demographics, vaccination status, or adoption of mitigation strategies on industry-specific seroprevalence was outside the scope of this analysis. Future work can build on these findings by considering the effects of those factors on infection rates by industry.
Our findings highlight the disproportionate impact of SARS-CoV-2 among workers across industry sectors, supporting the knowledge that work is an important determinant of health. Industries at increased risk of workplace exposure to SARS-CoV-2 or other respiratory viruses could benefit from continued efforts to evaluate the work environment to identify the most effective setting-specific combination of mitigation measures based on the hierarchy of controls. 20 More broadly, this analysis emphasizes an ongoing need for collecting industry and occupation data to better understand the relationship between work and health outcomes and take action more rapidly when outbreaks occur. These data can be valuable for public health and industry leaders to inform sector-specific policies, provide tailored guidance and mitigation measures, develop effective vaccine strategies, explain disease risk to workers, and reduce work-related health disparities.
This analysis represents one of the most complete national examinations to date of SARS-CoV-2 seroprevalence by industry. Our findings highlight work as a social determinant of the disproportionate SARS-CoV-2 seroprevalence and demonstrate the value of improving occupational data collection in public health surveillance systems. Industries with high prevalence of SARS-CoV-2 infection may benefit from sector-specific policy considerations and tailored guidance and mitigation measures.
Acknowledgements:
We acknowledge Marie De Perio, Stacey Marovich, Jeffrey Purdin, Pamela Schumacher, Jennifer Cornell, Elizabeth Smith, and Rebecca Purdin for their contributions to this project.
Funding:
The authors report that there was no funding source for the work that resulted in the article or the preparation of the article.
Institution and Ethics approval and informed consent: The American Red Cross institutional review board approved distribution of the survey (IRB 2020-015) and participants provided written informed consent. This activity was also reviewed by the Centers for Disease Control and Prevention (CDC 0900f3eb81d52cce) and was conducted consistent with applicable federal law and CDC policy.
Disclaimer:
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Footnotes
Disclosure: the authors declare no conflicts of interest
Institution at which the work was performed: National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention, Cincinnati, Ohio
45 C.F.R. part 46.102(l)(2), 21 C.F.R. part 56; 42 U.S.C. Sect. 241(d); 5 U.S.C. Sect. 552a; 44 U.S.C. Sect. 3501 et seq
References
- 1.Statement on the second meeting of the International Health Regulations. Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Accessed January 31, 2023. https://www.who.int/news/item/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov)
- 2.Trends in Number of COVID-19 Cases and Deaths in the US Reported to CDC, by State/Territory. Department of Health and Human Services. Accessed January 31, 2023. https://covid.cdc.gov/covid-data-tracker/#trends_totaldeaths_select_00
- 3.Alamilla SG, Cano M. COVID-19 and Adverse Social Determinants of Health. Behav Med. Apr-Jun 2022;48(2):67–71. doi: 10.1080/08964289.2022.2027859 [DOI] [PubMed] [Google Scholar]
- 4.Billock RM, Steege AL, Miniño A. COVID-19 Mortality by Usual Occupation and Industry:46 States and New York City, United States, 2020. Natl Vital Stat Rep. Oct 2022;71(6):1–33. [PubMed] [Google Scholar]
- 5.Gaffney A, Himmelstein DU, McCormick D, Woolhandler S. COVID-19 Risk by Workers’ Occupation and Industry in the United States, 2020‒2021. Am J Public Health. Jun 2023;113(6):647–656. doi: 10.2105/ajph.2023.307249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: A key factor in containing risk of COVID-19 infection. PLoS One. 2020;15(4):e0232452. doi: 10.1371/journal.pone.0232452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cox-Ganser JM, Henneberger PK, Weissman DN, Guthrie G, Groth CP. COVID-19 test positivity by occupation using the Delphi US COVID-19 trends and impact survey, September-November 2020. Am J Ind Med. Sep 2022;65(9):721–730. doi: 10.1002/ajim.23410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steege AL, Luckhaupt SE, Guerin RJ, et al. Characteristics Associated With a Previous COVID-19 Diagnosis, Vaccine Uptake, and Intention to Be Vaccinated Among Essential Workers in the US Household Pulse Survey. Am J Public Health. Nov 2022;112(11):1599–1610. doi: 10.2105/ajph.2022.307010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang M. Estimation of differential occupational risk of COVID-19 by comparing risk factors with case data by occupational group. Am J Ind Med. Jan 2021;64(1):39–47. doi: 10.1002/ajim.23199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Luckhaupt SE, Horter L, Groenewold MR, et al. COVID-19 Outbreaks Linked to Workplaces, 23 US Jurisdictions, August-October 2021. Public Health Rep. Dec 8 2022:333549221138294. doi: 10.1177/00333549221138294 [DOI] [PMC free article] [PubMed]
- 11.Pray IW, Grajewski B, Morris C, et al. Measuring Work-related Risk of Coronavirus Disease 2019 (COVID-19): Comparison of COVID-19 Incidence by Occupation and Industry—Wisconsin, September 2020 to May 2021. Clinical Infectious Diseases. 2022;doi: 10.1093/cid/ciac586 [DOI] [PMC free article] [PubMed]
- 12.Wuellner S. COVID-19 Case Rates by Industry and Occupation, January 10, 2020 to June 29, 2021. https://lni.wa.gov/safety-health/safety-research/files/2022/103_09_2022_IO_by_TimePeriod.pdf. Accessed 24 October 2023.
- 13.Shah MM, Spencer BR, Feldstein LR, et al. Occupations Associated With Severe Acute Respiratory Syndrome Coronavirus 2 Infection and Vaccination, US Blood Donors, May 2021–December 2021. Clinical Infectious Diseases. 2022;doi: 10.1093/cid/ciac883 [DOI] [PubMed]
- 14.EUA Authorized Serology Test Performance. Available at: https://www.fda.gov/medical-devices/coronavirus-disease-2019-covid-19-emergency-use-authorizations-medical-devices/eua-authorized-serology-test-performance. Accessed 24 October 2023.
- 15.Haynes JM, Dodd RY, Crowder LA, et al. Trajectory and Demographic Correlates of Antibodies to SARS-CoV-2 Nucleocapsid in Recently Infected Blood Donors, United States. Emerging Infectious Diseases. 2023;29(7):1323–1329. doi: 10.3201/eid2907.230173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sulaeman H, Grebe E, Dave H, et al. Evaluation of Ortho VITROS and Roche Elecsys S and NC Immunoassays for SARS-CoV-2 Serosurveillance Applications. Microbiol Spectr. 2023;11(4):e0323422. doi: 10.1128/spectrum.03234-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loesche M, Karlson EW, Talabi O, et al. Longitudinal SARS-CoV-2 Nucleocapsid Antibody Kinetics, Seroreversion, and Implications for Seroepidemiologic Studies. Emerging Infectious Diseases. 2022;28(9):1859–1862. doi: 10.3201/eid2809.220729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Collecting and Using Industry and Occupation Data. Centers for Disease Control and Prevention. Accessed January 31, 2023. https://www.cdc.gov/niosh/topics/coding/code.html
- 19.Protecting Workers: Guidance on Mitigating and Preventing the Spread of COVID-19 in the Workplace. United States Department of Labor. Accessed Janurary 31, 2023. https://www.osha.gov/coronavirus/safework
- 20.Tamers SL, Chosewood LC, Childress A, Hudson H, Nigam J, Chang CC. Total Worker Health(®) 2014⁻2018: The Novel Approach to Worker Safety, Health, and Well-Being Evolves. Int J Environ Res Public Health. Jan 24 2019;16(3)doi: 10.3390/ijerph16030321 [DOI] [PMC free article] [PubMed] [Google Scholar]


