Abstract
Practical relevance The clinical importance of feline hypertension has been recognised for many years and most feline practitioners are quite familiar with this syndrome. Once systemic hypertension is identified, long-term management of the patient is needed to avoid catastrophic (eg, blindness due to retinal detachment) or subtle (eg, accelerated renal damage) target organ damage.
Patient group Feline systemic hypertension is most commonly a complication of renal disease and hyperthyroidism, both diseases of older feline patients. By 15 years of age, the probability of having at least one of these two diseases is high. As well cared for cats are living longer, optimal long-term management of feline hypertension in patients with concurrent diseases is an issue of clinical importance.
Clinical challenges Obtaining accurate blood pressure measurements in patients that are anxious, fractious or just plain uncooperative remains a significant issue in feline medicine, as does confident analysis of results from these patients.
Diagnostics Careful measurement of systolic blood pressure using Doppler or oscillometric techniques in conjunction with evaluation for evidence of hypertensive choroidopathy (funduscopic examination) and hypertensive cardiac changes (thoracic auscultation) are essential to the diagnosis of systemic hypertension in cats. Other diagnostic techniques, including evaluation of renal and thyroid function, are needed to detect the underlying disease condition.
Evidence base Numerous well-designed clinical studies have greatly advanced our understanding of the most appropriate methods of diagnosis and therapy of feline hypertension.

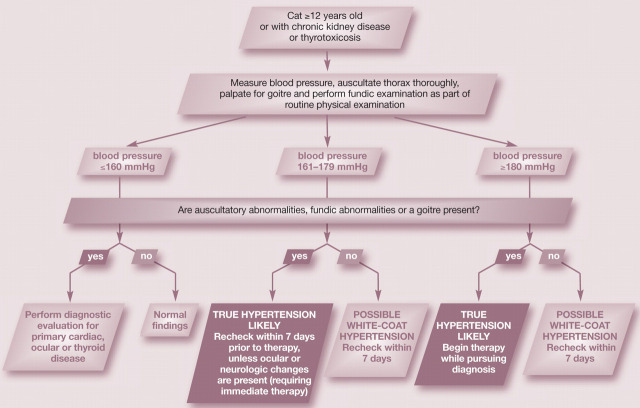
Accurate identification of feline patients with systemic hypertension is a multistep procedure, involving identification of the population to which the test should be applied, careful and accurate blood pressure measurement, and assessment of blood pressure measurement results in conjunction with results of examination for target organ damage (TOD). Once hypertension is diagnosed, a medical management and monitoring plan can be initiated.
Patient population
The feline population in which blood pressure assessment is recommended includes middle-aged to older cats (>9–12 years old), cats with diseases known to be associated with feline hypertension, and, most importantly, cats with evidence of TOD, including ocular, neurologic or cardiac abnormalities. 1
In feline patients, secondary hypertension (as a complication of another systemic disease) is the most common form of hypertension, but idiopathic hypertension (a condition in which background medical evaluation does not reveal an underlying disease likely to cause hypertension) may account for up to 20% of hypertensive patients. 2,3 In one study that included seven cats with idiopathic hypertension, 4 it appeared that most or all of these cats were >12 years of age. Such cases may be identified even in the absence of systemic illness if blood pressure screening of senior cats is routine.
Cats requiring blood pressure testing.
-
Cats with evidence of target organ damage:
– Ocular signs∗, including retinal haemorrhage, retinal detachment, subretinal oedema or hyphaema
– Intracranial neurologic signs∗, including obtundation, focal facial seizures and photophobia
– Auscultable cardiac abnormalities, including gallop rhythms and systolic heart murmurs
Cats with known or suspected chronic renal disease, hyperthyroidism or adrenal abnormalities, including cats treated for hyperthyroidism within the past 6 months
Middle-aged to older cats (>9–12 years old), as a routine screening measure
∗Cats with ocular or neurologic signs and elevated blood pressure should be treated immediately to limit damage and avoid progression
CLASSIFICATION AND PATHOGENESIS.
A sister article addressing the classification and pathogenesis of feline hypertension appears on pages 25–34 of this issue of J Feline Med Surg, and at: doi:10.1016/j.jfms.2010.11.007
Certain systemic illnesses (chronic kidney disease [CKD], hyperthyroidism, adrenal diseases) are repeatedly and closely associated with hypertension in cats. 1 Approximately 20–60% of feline CKD patients are hypertensive. 5–7 The reported prevalence of hypertension in hyperthyroid cats is likewise variable, but is considered to be approximately 10–20%. 7,8 Cats treated for hyperthyroidism remain at increased risk for the development of hypertension for up to 6 months; in one study, up to 30% of cats treated for hyperthyroidism became hypertensive within 6 months of successful thyroid therapy. 8 Adrenal disease, most frequently adrenal neoplasia, is a documented but relatively uncommon cause of secondary hypertension in cats. 3,9,10
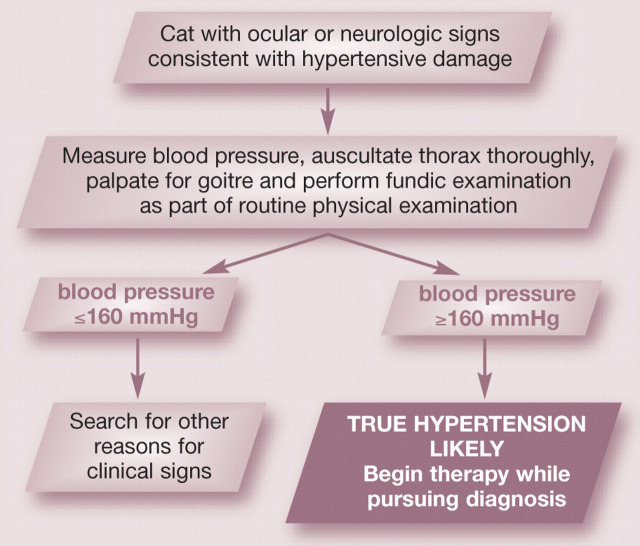
As is the case in dogs and people, the detection of evidence of TOD in a clinical patient should trigger immediate assessment of blood pressure. Target organ damage is common in hypertensive cats; ocular abnormalities are detected in about 40–60% of hypertensive cats, palpable goitre is present in 30–40%, auscultable cardiac abnormalities are detected in about 50–70% 4,7,11–13 and neurologic abnormalities in approximately 15%. 13
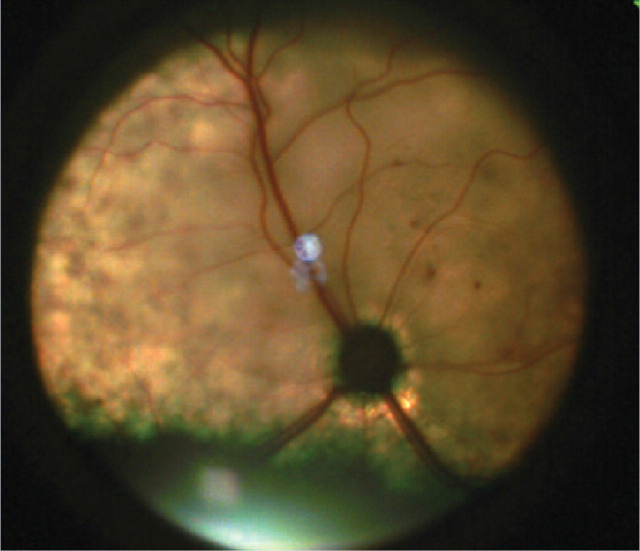
Hypertensive choroidopathy is the commonly detected form of TOD in cats. Hypertension is associated with abnormalities of the retina (including oedema, haemorrhage and partial or complete detachment that may associated with acute onset of vision loss), choroidal abnormalities (resulting in serous retinal detachment) and hyphaema. 3,7,14,15 Although papilloedema may be present, it may be difficult to appreciate due to concurrent retinal detachment or hyphaema. 15 Clinical signs associated with increased intracranial pressure (eg, dullness, obtundation, focal facial seizures or sensitivity to light) may be associated with neurologic TOD, and the presence of these signs should lead to blood pressure evaluation.
Lastly, although abnormalities in cardiac auscultation findings due to ventricular hypertrophy secondary to hypertension commonly include gallop rhythms and heart murmurs, congestive heart failure is an uncommon sequela of cardiac TOD. Although there are multiple possible causes of auscultable abnormalities in cats, blood pressure measurement is indicated when such changes are present, even if CKD, hyperthyroidism or ocular abnormalities are absent. In this type of patient, excluding a diagnosis of hypertension is an integral part of the evaluation of possible cardiomyopathy.
Choice of technique
Although other combinations of techniques and cuff placements 13,16,17 have been evaluated, the most commonly used methods for blood pressure measurement in cats are Doppler sphygmomanometry with the cuff placed at the mid-forelimb, and oscillometric techniques with the cuff placed at the tailhead. The technical aspects of these techniques have been well described 5,16,18–20 and either method may be used to accurately estimate systolic blood pressure (SBP) in a clinical patient.
If both techniques are available, the one most appropriate for the patient may be chosen based on the cat's level of anxiety and willingness to be gently restrained. Doppler methods may be preferred if the patient can be restrained in a sitting position and is willing to have its feet handled. If the patient is exceptionally fractious or prefers minimal restraint, the oscillometric method using a tail cuff allows manipulation away from the patient's head as well as the opportunity for the cat to be minimally handled during the measurement process. The Doppler technique is more labour intensive, but the oscillometric technique may take longer to acquire the measurements, especially if patient movement is an issue. 16,21
Signs of target organ damage.
Hypertensive choroidopathy
Evidence of subretinal oedema, subretinal haemorrhage, retinal detachment, hyphaema or tortuous retinal vessels
-
Increased intracranial pressure
Evidence of obtundation, mental dullness, focal facial seizures or sensitivity to light (photophobia)
-
Hypertensive cardiac hypertrophy
Evidence of new gallop rhythm or heart murmur
Doppler measurement.
Cats tend to be most comfortable in a sitting position with the chosen fore-limb gently extended by the restrainer such that the elbow is not acutely flexed and the cuff is approximately level with the cat's heart. Doppler measurement provides the best results in relaxed patients and those with rapid heart rates but the technique is dependent on the skill of the measurer and the willingness of the cat to have its feet handled.
Blood pressure measurement using Doppler sphygmomanometry. An appropriate-sized cuff is positioned at mid-radius level on the cat. Note the gentle restraint, comfortable position of the patient and positioning of the limb such that the cuff is at the level of the cat's heart
Oscillometric measurement.
Most cats settle into a sternal position and, as such, the tail cuff is naturally close to the level of the heart. Hyperthyroid cats can be especially irritable, and although use of oscillometric techniques with a tail cuff is recommended for especially fractious cats to reduce personnel exposure to teeth and claws, this specific technique may lead to false elevations of blood pressure in hyperthyroid cats and the evaluator should consider this information when interpreting results. 24
Blood pressure measurement using an oscillometric technique. An appropriate-sized cuff is positioned at the tailhead of the cat and, without requiring any patient manipulation, is approximately at the level of the heart. Note the comfortable position, and minimal restraint, of the patient
White-coat hypertension presents a significant problem because practitioners frequently question the ‘reality’ of elevated blood pressure measurements in fractious, nervous or uncooperative cats.
There is some evidence that the normal range of SBP in cats may vary between these techniques, with the upper end of the normal range being approximately 160 mmHg using Doppler methods with a forelimb cuff, and somewhat lower, at about 140 mmHg, using oscillometric methods with a tail cuff. 20,21
Avoiding errors in diagnostic testing
Measurement of SBP in cats has been integrated into the clinical routine in many veterinary clinics. It is important to be aware, however, that limitations in blood pressure measurement techniques can lead to inaccurate or confusing results. Clearly the aim must be to avoid errors in diagnostic testing as these, in turn, can lead to inappropriate over- or under-medication.
Doppler and oscillometric techniques rarely deliver a falsely low reading (false negative), 16 but so-called ‘white-coat’ hypertension (ie, blood pressure is increased as a result of the measurement process itself but is not elevated in a non-measurement situation) 1 may lead to a falsely elevated blood pressure in a normotensive patient (false positive). Although the exact prevalence of white-coat hypertension in clinical practice is unclear, it presents a significant problem in terms of blood pressure interpretation in cats, with practitioners frequently questioning the ‘reality’ of elevated blood pressure measurements in fractious, nervous or uncooperative patients. 22 This is frequently mentioned as being an issue in clinical studies of feline hypertension. 4,13,23
Minimising the problem of white-coat hypertension in clinical feline patients is best achieved using a multifaceted approach. Decreasing the stress of the clinic visit and blood pressure measurement to the degree possible in a normal clinic day (see box on page 38), interpreting the blood pressure findings in conjunction with noted demeanour in order to evaluate patient stress level, and careful patient screening for the presence/absence of ocular changes and auscultable changes compatible with hypertension provide additive information. A high heart rate does not appear to be a reliable indicator of white-coat hypertension in normal cats, 22 but may reflect systemic illness (eg, heart rates >220 bpm may be present in hyperthyroid patients). A cat with a fractious or anxious demeanour, blood pressure ≥160 mmHg and no evidence of TOD should have its blood pressure rechecked within a week under as optimal conditions as can be managed. True elevations in blood pressure appear to be stable week to week. 4
Based on presently available data, SBP values ≥180 mmHg are unlikely to reflect white-coat hypertension and should be treated as ‘real', with a full diagnostic evaluation for TOD and a search for underlying disease. 22 Blood pressure >160 mmHg in a cat with known CKD, hyperthyroidism, ocular changes or auscultable abnormalities is likely to represent true hypertension and the presence of neurologic or ocular abnormalities warrants immediate therapy.
Based on presently available data, SBP values ≥180 mmHg are unlikely to reflect white-coat hypertension and should be treated as ‘real', with a full diagnostic evaluation for TOD and a search for underlying disease.
Optimal management of blood pressure measurement.
The ideal management of blood pressure measurement requires conditions that are difficult to obtain in a busy clinic — namely, a calm and quiet approach to the patient, attention to the sequencing of events during the clinic visit and unrushed, methodical repeated measurements using the correct-sized cuff. However, efforts to optimise clinical organisation of blood pressure measurement will ensure results are more reliable, and patients and personnel are less beleaguered by the process. Client information should emphasise that time-intensive but reliable measurement is ultimately more cost-effective than repeated unreliable measurements.
Calm quiet approach
Blood pressure measurement should take place in a relatively quiet environment (eg, an examination room or another room away from loud, sudden noises and other animals); blood pressure measurement in a busy ward or common area should be avoided. Giving the cat an opportunity to rest quietly or wander around the room for a few minutes before measurement will allow it to become used to the surroundings. For particularly anxious patients, dimming of lights may be helpful. Ideally, the client may hold the cat in their lap or comfort it during the procedure. If this is not possible or desirable, gentle restraint by an experienced person provides the best results.
Sequencing of events
If the need to measure blood pressure is known prior to the physical examination, the accommodation period and measurement procedure should precede the physical examination and, especially, use of a rectal thermometer. 22 If it becomes clear based on the history, physical examination or other diagnostic test results that a feline patient requires blood pressure measurement in the course of the day, this should precede any sedation or anaesthesia, and should be separated from other clinical procedures (eg, blood sampling, catheter placement) by 30–60 mins to allow the cat to re adjust after any stress from these unfamiliar procedures. Hair clipping is not needed in the majority of patients (dampening the hair with spirits will suffice); either way, these should be regarded as stressful procedures (ie, the patient should be allowed to re-acclimate after hair dampening or clipping, if needed).
Methodical, repeated measurements
In all cases, the accuracy of results is increased when the average value of at least five individual blood pressure measurements is used as a representative value. 16 Heart rate should be recorded during the blood pressure measurement process as a possible indicator of underlying disease (eg, hyperthyroidism).
Irrespective of whether Doppler or oscillometric methods are used, the limb or tail circumference should be measured with a soft tape measure, and a cuff with a width approximately 40% of the circumference should be chosen for measurement. A ‘one size fits all’ approach should be avoided, as overly large cuffs will deliver falsely low values and overly small cuffs will deliver falsely elevated values.
Measurement of the tailhead circumference in a cat to determine the appropriate size of tail cuff for oscillometric blood pressure measurement
A diagnosis of hypertension should be strongly considered in a cat with Doppler forelimb SBP ≥160 mmHg or oscillometric tail cuff SBP ≥140–160 mmHg.
Interpreting an elevated blood pressure
Once a representative blood pressure measurement is obtained from a patient, diagnosis of hypertension involves integrating the measurement results with the history and results of a routine but complete physical examination. A recent consensus statement has emphasised the gradually increasing risk of TOD as SBP rises above 160 mmHg, 1 and most studies have concentrated on the use of SBP as offering the most accurate and consistently obtainable value for the diagnosis of hypertension in cats. Although some variability occurs in the literature, most studies have concluded that further consideration of a diagnosis of hypertension is strongly recommended with a Doppler fore-limb SBP ≥160 mmHg or oscillometric tail cuff SBP ≥140–160 mmHg.
Specific attention should be paid during the physical examination to identification of factors that reflect TOD (eg, funduscopic examination, gross neurologic evaluation, and thoracic auscultation including heart rate as a possible indicator of hyperthyroidism), evaluation of the patient's stress level, and physical evaluation for thyroid, renal or adrenal disease (eg, evaluation for a cervical thyroid nodule, palpable small and irregular kidneys, and palpation for abdominal masses). When elevated blood pressure results are found concurrent with appropriate abnormalities of any of these systems, the probability of the blood pressure reflecting ‘true’ hypertension is increased.
Diagnostic algorithm for senior cats
Ocular abnormalities
Funduscopic examinations are frequently overlooked in the course of a busy day of clinical evaluations, but the prevalence of ocular TOD in hypertensive cats is high (40–65%). 4,5,7,11 Detection of ocular abnormalities consistent with hypertensive choroidopathy will increase the confidence of a diagnosis in a questionable case, as well as triggering needed ophthalmological care and appropriate ancillary testing in affected animals. Funduscopic examination should be considered an integral part of evaluation for hypertension, and performed routinely in screening examinations.
Gross neurologic status
Neurologic abnormalities reflecting systemic hypertension in cats are typically those of intracranial disease, including changes in mentation (eg, dullness, obtundation), focal facial seizures and, in some cats, photophobia (usually seen as squinting). Although most intracranial signs are obvious during routine evaluation of the patient's mentation, optic nerve swelling in response to increased intracranial pressure may be seen via a funduscopic examination.

Hypertensive cat with ocular TOD including bilateral retinal detachment. The patient is also exhibiting photophobia (squinting and avoidance of bright light)
Diagnostic algorithm for cats with evidence of target organ damage
Patients with elevated blood pressure on two occasions are considered likely to have ‘true’ hypertension.
Auscultable abnormalities
Auscultable abnormalities, including heart murmurs, gallop rhythms and irregular heart rhythms, are more common in hypertensive cats than in normal cats 4,5,13 and reflect the secondary hypertrophy that occurs as a response to chronic hypertension. 13,25 Primary hypertrophic cardiac diseases are also common in cats (eg, hypertrophic cardiomyopathy [HCM]). Thus blood pressure measurement in cats with auscultatory abnormalities serves two purposes: as a screening test for hypertension and as a necessary diagnostic test to disprove hypertension as a cause of cardiac hypertrophy in cats with HCM.
Careful auscultation of ill cats of any age as well as overtly healthy geriatric cats will identify this important subgroup of cats with TOD.
Reconfirming an elevated blood pressure result
With the exception of patients displaying detectable TOD, a second, confirmatory blood pressure measurement can be scheduled for cats in which the blood pressure value is borderline or ambiguous when interpreted in conjunction with clinical findings. Elevated blood pressure appears to be a consistent finding in hypertensive cats if the blood pressure is remeasured within hours 26,27 or days. 4 If TOD is present, antihypertensive medications should be initiated prior to further evaluation. 1 Patients with elevated blood pressure on two occasions are considered likely to have ‘true’ hypertension. 4
Therapy of systemic hypertension in cats
Once hypertension is diagnosed in a feline patient, treatment and monitoring can begin. In cases where hyperthyroidism or CKD is present, optimal therapies for these problems should be initiated. Cats with hypertension related to CKD are likely to require lifelong therapy. For hyperthyroid cats, blood pressure should be closely monitored before and after therapy for hyperthyroidism. Cats that have blood pressure measurements >180 mmHg prior to therapy for hyperthyroidism are likely to remain hypertensive, while cats that are normotensive prior to therapy for hyperthyroidism should be monitored for approximately 6 months after therapy to detect development of hypertension after therapy. 8
Based on the currently accepted idea that the risk of TOD increases as blood pressure increases above normal for the patient, anti-hypertensive therapy should be administered with the initial goal of achieving an SBP of ≤160 mmHg, with maintenance of SBP around 140 mmHg without side effects as the optimal goal to minimise ongoing TOD. 1
The two most most commonly used medications for treating feline hypertension in an outpatient setting are amlodipine and angiotensin-converting enzyme inhibitors (ACEi).
Amlodipine
A body of literature exists suggesting that amlodipine besylate, a dihydropyridine calcium-channel blocking agent, is a safe and effective therapy for hypertension in cats. The drug has been evaluated in research cats 28 and clinical feline patients 4,11,27,29,30 and found to decrease SBP by an average of 30–50 mmHg. 4,11,28 Amlodipine also decreases the degree of proteinuria, 11 a clinical parameter that has been linked with survival. 31 Two studies of survival in hypertensive cats treated with amlodipine could find no direct survival benefit of effective amlodipine therapy, 11,31 but multiple research and anecdotal reports have documented improved quality of life in hypertensive cats treated with amlodipine. 4,29 In many senior cats, the link between quality of life and survival is direct; if amlodipine improves quality of life, it is likely to extend length of life in many patients.
Maintenance of appetite and weight, and avoidance of catastrophic TOD (eg, acute blindness due to retinal detachment, obtundation), are valuable endpoints for any anti-hypertensive therapy. Amlodipine therapy should begin immediately if evidence of ocular or neurological TOD is present at the time of diagnosis.
Angiotensin-converting enzyme inhibitors
Angiotensin-converting enzyme inhibitors (eg, enalapril, benazepril, ramipril) have systemic and glomerular antihypertensive effects, making this class of medication of particular interest for cats with any degree of proteinuria or albuminuria. Evidence of long-term efficacy of ACEi in the treatment of feline hypertension is variable and may depend on the type of ACEi used. In earlier studies, sustained antihypertensive efficacy was not seen in cats with CKD, 32 but a more recent study reported blood pressure returning to the normal range in 69% of cats treated with ramipril. 33 Another study reported a cumulative antihypertensive effect when benazepril was added to amlodipine therapy in hypertensive cats. 34 Benazepril has been shown to decrease renal protein loss in cats with naturally occurring CKD without documented survival benefit; 35 it also prevented or reversed glomerular hypertension and reduced SBP modestly (∼10 mmHg) in cats with induced renal failure. 36 The reason for these varied results may be that different hypertensive cats have different levels of RAAS activation — available research findings are conflicting. 20,32
Medications for outpatient management of chronic feline hypertension.
Amlodipine Initial dose 0.125 mg/kg PO q24h. Increase to 0.25 mg/kg PO q24h, if needed
Benazepril 0.5–1.0 mg/kg PO q12-24h
Ramipril Initial dose 0.125 mg/kg PO q24h. Increase to 0.25 mg/kg PO q24h, if needed
Notes: This information is based on Van Israel et al. 33 Concurrent benazepril and amlodipine use appears to be safe; renal function should be monitored. No clinical information is available regarding use of ramipril with amlodipine in cats.
In the author's clinic, amlodipine is the first-line therapy for cats with hypertension. Benazepril is typically added if proteinuria or albuminuria is present, or if hypertension remains uncontrolled after an increase in amlodipine dose from an initial 0.125 mg/kg to 0.25 mg/kg daily.
Case notes.
Pickle, a 15-year-old female spayed domestic shorthair cat, was presented for emergency examination with an increased respiratory rate of 2 days’ duration. She had no significant medical history prior to this presentation.
Physical examination Pickle was alert and quiet. Her rectal temperature was 37.6°C (99.7°F), her respiratory rate was elevated at 42 breaths/min and her ausculted heart rate was 200 bpm, with a gallop rhythm. Pickle's femoral pulse strength was normal and no pulse deficits were present. Her body weight was 3.8 kg. Lung sounds were increased in all fields and abdominal palpation revealed small, irregular kidneys and a palpable bladder. Pickle's lymph nodes were normal, but a thyroid mass (goitre) was noted.
A retinal examination revealed large multifocal areas of retinal elevation with petechial haemorrhages in each eye.
Initial diagnostics Unsedated radiographs were obtained, and revealed pleural effusion and cardiomegaly. Pertinent blood biochemistry and urinalysis results were: blood urea nitrogen 22.13 mmol/l (reference interval [RI] 5–8.92 mmol/l); creatinine 203.32 umol/l (RI 79.56–176.8 umol/l); packed cell volume 40% (RI 27–45%); total protein 85 g/l (RI 57–75 g/l); urine specific gravity 1.015 with quiet sediment and 1+ protein on a dipstick. A sample of the pleural fluid (35 cc), obtained by thoracocentesis, was slightly cloudy with a total protein of 39 g/l.
Diffuse elevation of the retina around the optic nerve is causing an ‘unfocused’ appearance, although retinal vessels remain in focus. Punctate intraretinal haemorrhages are noted in the upper right portion of the image. Courtesy of Dr Ellison Bentley
WHAT IS YOUR ASSESSMENT?
-
1
Possible aetiologies for Pickle's pleural effusion include all of the following except:
-
(a)
Hypertrophic cardiomyopathy with heart failure
-
(b)
Idiopathic chylothorax
-
(c)
Systemic hypertension
-
(d)
Thyrotoxic heart disease with heart failure
-
(e)
Pyothorax
-
(a)
-
2
What rational additional test(s) would you recommend performing immediately?
-
(a)
Additional thoracocentesis if dyspnoea is severe
-
(b)
Doppler blood pressure measurement
-
(c)
Serum thyroxine analysis
-
(d)
Echocardiography
-
(e)
All of the above tests
-
(a)
Left lateral radiograph of Pickle, showing generalised cardiomegaly and moderate pleural effusion
In the author's clinic, amlodipine continues to be the first-line therapy for cats with hypertension, and benazepril is typically added if proteinuria or albuminuria is present or if hypertension remains uncontrolled (SBP ≥160 mmHg) after an increase in amlodipine dose from an initial dose of approximately 0.125 mg/kg to 0.25 mg/kg daily.
Monitoring
If ocular or neurologic TOD is present at the time of diagnosis, close monitoring of blood pressure over the first 24 h of therapy is advisable. When this is not possible, rechecking of blood pressure within 24 h is recommended to ensure an adequate response to therapy. Other, more stable patients can have their blood pressure rechecked within 3–7 days of starting therapy. At the recheck examination, blood pressure and renal function should be evaluated, as well as urine protein content if proteinuria was diagnosed as part of the patient's illness.
Once blood pressure is stable on medications, blood pressure measurement should take place routinely at approximately 3-month intervals. These rechecks should include funduscopic examinations and thoracic auscultation, as animals with inadequate blood pressure control and no ocular lesions at initial diagnosis may subsequently develop ocular lesions. 4 Development of new auscultatory abnormalities may signal inadequate blood pressure control or development of concurrent, unrelated cardiovascular disease.
KEY POINTS.
Cats with evidence of target organ damage (ocular, neurologic or cardiovascular) and cats with renal, adrenal or thyroid disease are candidates for blood pressure assessment.
Routine screening of blood pressure at each exam is appropriate for middle-aged to older cats, even if overtly normal.
Time-intensive but reliable blood pressure measurements are more cost-effective than hurried measurements that must be repeated.
Systolic blood pressure ≥180 mmHg, with or without target organ damage, is unlikely to be due to ‘white-coat’ hypertension.
Patients with target organ damage and systemic hypertension should be treated with antihypertensive medications prior to further medical investigation.
Case notes continued.
Pickle did not require additional thoracocentesis. Her serum thyroxine was 72.07 nmol/l (RI 24.45–61.78 nmol/l), SBP (Doppler, forelimb) was 215 mmHg and heart rate 234 bpm. Echocardiography revealed moderate left atrial enlargement with no valvular insufficiencies. Mild global left ventricular wall thickening was present, with normal left ventricular diameter and normal systolic function. These findings were considered compatible with mild left ventricular hypertrophy secondary to systemic disease (eg, systemic hypertension and/or hyperthyroidism).
Final diagnoses
Partial retinal detachment and retinal haemorrhage secondary to systemic hypertension
Systemic hypertension, likely secondary to chronic renal disease and thyrotoxicosis
Congestive heart failure secondary to thyrotoxic heart disease
Initial therapy
Amlodipine (0.3 mg PO q24h for systemic hypertension)
Frusemide (3 mg PO q12h for heart failure)
Benazepril (1.25 mg PO q12h for heart failure and systemic hypertension)
Methimazole (5 mg PO q12h for medical therapy of hyperthyroidism)
Follow-up Pickle's systolic blood pressure on recheck examination 3 days later was 200 mmHg (improved but not in target range). The dose of amlodipine was increased to 0.625 mg PO q24h. A further 3 days later Pickle's SBP was 152 mmHg and her pleural effusion had resolved radiographically. Ophthalmologic examination 2 weeks later showed reattachment of the retina in each eye. Frusemide was discontinued when serum thyroxine had normalised. Pickle's most recent recheck was 9 months after her original presentation, at which time she was clinically stable. She continues to receive amlodipine, benazepril and methimazole.
References
- 1. Brown S, Atkins C, Bagley R, et al. Guidelines for the identification, evaluation, and management of systemic hypertension in dogs and cats. J Vet Intern Med 2007; 21: 542–58. [DOI] [PubMed] [Google Scholar]
- 2. Elliott J, Fletcher M, Syme HM. Idiopathic feline hypertension: epidemiologic study [abstract]. J Vet Intern Med 2003; 17: 754. [Google Scholar]
- 3. Maggio F, DeFrancesco TC, Atkins CE, Pizzirani S, Gilger BC, Davidson MG. Ocular lesions associated with systemic hypertension in cats: 69 cases (1985–1998). J Am Vet Med Assoc 2000; 217: 695–702. [DOI] [PubMed] [Google Scholar]
- 4. Elliott J, Barber PJ, Syme HM, Rawlings JM, Markwell PJ. Feline hypertension: clinical findings and response to anti-hypertensive treatment in 30 cases. J Small Anim Pract 2001; 42: 122–29. [DOI] [PubMed] [Google Scholar]
- 5. Syme HM, Barber PJ, Markwell PJ, Elliott J. Prevalence of systolic hypertension in cats with chronic renal failure at initial evaluation. J Am Vet Med Assoc 2002; 220: 1799–804. [DOI] [PubMed] [Google Scholar]
- 6. Kobayashi DL, Peterson ME, Graves TK, Lesser M, Nichols CE. Hypertension in cats with chronic renal failure or hyperthyroidism. J Vet Intern Med 1990; 4: 58–62. [DOI] [PubMed] [Google Scholar]
- 7. Stiles J, Polzin DJ, Bistner SI. The prevalence of retinopathy in cats with systemic hypertension and chronic renal failure or hyperthyroidism. J Am Anim Hosp Assoc 1994; 30: 564–72. [Google Scholar]
- 8. Syme HM, Elliott J. Prevalence of hypertension in hyperthyroid cats at diagnosis and following treatment [abstract]. Proceedings of the 13th ECVIM-CA Congress 2003: 754.
- 9. Ash RA, Harvey AM, Tasker S. Primary hyperaldosteronism in the cat: a series of 13 cases. J Feline Med Surg 2005; 7: 173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maher ER, Jr, McNiel EA. Pheochromocytoma in dogs and cats. Vet Clin North Am Small Anim Pract 1997; 27: 359–80. [DOI] [PubMed] [Google Scholar]
- 11. Jepson RE, Elliott J, Brodbelt D, Syme HM. Effect of control of systolic blood pressure on survival in cats with systemic hypertension. J Vet Intern Med 2007; 21: 402–9. [DOI] [PubMed] [Google Scholar]
- 12. Littman MP. Spontaneous systemic hypertension in 24 cats. J Vet Intern Med 1994; 8: 79–86. [DOI] [PubMed] [Google Scholar]
- 13. Chetboul V, Lefebvre HP, Pinhas C, Clerc B, Boussouf M, Pouchelon J-L. Spontaneous feline hypertension: clinical and echocardiographic abnormalities, and survival rate. J Vet Intern Med 2003; 17: 89–95. [DOI] [PubMed] [Google Scholar]
- 14. Sansom J, Barnett KC, Dunn KA, Smith KC, Dennis R. Ocular disease associated with hypertension in 16 cats. J Small Anim Pract 1994; 35: 604–11. [Google Scholar]
- 15. Crispin SA, Mould JRB. Systemic hypertensive disease and the feline fundus. Vet Ophthal 2001; 4: 131–40. [DOI] [PubMed] [Google Scholar]
- 16. Haberman CE, Morgan JD, Kang CW, Brown SA. Evaluation of Doppler ultrasonographic and oscillometric methods of indirect blood pressure measurement in cats. J Appl Res Vet Med 2004; 2: 279–89. [Google Scholar]
- 17. Jepson RE, Hartley V, Mendl M, Caney S, Gould DJ. A comparison of CAT Doppler and oscillometric Memoprint machines for non-invasive blood pressure measurement in conscious cats. J Feline Med Surg 2005; 7: 147–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Henik RA, Dolson MK, Wenholz LJ. How to obtain a blood pressure measurement. Clin Tech Small Anim Pract 2005; 20: 144–50. [DOI] [PubMed] [Google Scholar]
- 19. Stepien RL, Elliott J. Measurement of blood pressure. In: Elliott J, Grauer GF, eds. BSAVA manual of canine and feline nephrology and urology. Gloucester, UK: British Small Animal Veterinary Association, 2007: 178–91. [Google Scholar]
- 20. Mishina M, Watanabe T, Fujii K, Maeda H, Wakao Y, Takahashi M. Non-invasive blood pressure measurements in cats: clinical significance of hypertension associated with renal failure. J Vet Med Sci 1998; 60: 805–8. [DOI] [PubMed] [Google Scholar]
- 21. Bodey AR, Sansom J. Epidemiological study of blood pressure in domestic cats. J Small Anim Pract 1998; 39: 567–73. [DOI] [PubMed] [Google Scholar]
- 22. Belew AM, Barlett T, Brown SA. Evaluation of the white-coat effect in cats. J Vet Intern Med 1999; 13: 134–42. [DOI] [PubMed] [Google Scholar]
- 23. Sparkes AH, Caney SMA, King MCA, Gruffydd-Jones TJ. Inter- and intraindividual variation in Doppler ultrasonic indirect blood pressure measurements in healthy cats. J Vet Intern Med 1999; 13: 314–18. [DOI] [PubMed] [Google Scholar]
- 24. Stepien RL, Rapoport GS, Henik RA, Sartor LL. Effect of measurement method on blood pressure findings in cats before and after therapy for hyperthyroidism [abstract]. J Vet Intern Med 2003; 17: 754. [Google Scholar]
- 25. Sampendrano CC, Chetboul V, Gouni V, Nicolle AP, Pouchelon J-L, Tissier R. Systolic and diastolic myocardial dysfunction in cats with hypertrophic cardiomyopathy or systemic hypertension. J Vet Intern Med 2006; 20: 1106–15. [DOI] [PubMed] [Google Scholar]
- 26. Klevans LR, Hirkaler G, Kovacs JL. Indirect blood pressure determination by Doppler technique in renal hypertensive cats. Am J Physiol 1979; 237: H720–H3. [DOI] [PubMed] [Google Scholar]
- 27. Snyder P. Amlodipine: a randomized, blinded clinical trial in 9 cats with systemic hypertension. J Vet Intern Med 1998; 12: 157–62. [DOI] [PubMed] [Google Scholar]
- 28. Mathur S, Syme H, Brown CA, et al. Effects of the calcium channel antagonist amlodipine in cats with surgically induced hypertensive renal insufficiency. Am J Vet Res 2002; 63: 833–39. [DOI] [PubMed] [Google Scholar]
- 29. Henik RA, Snyder PS. Treatment of systemic hypertension in cats with amlodipine besylate. J Am Anim Hosp Assoc 1997; 33: 226–34. [DOI] [PubMed] [Google Scholar]
- 30. Snyder PS, Sadek D, Jones GL. Effect of amlodipine on echocardiographic variables in cats with systemic hypertension. J Vet Intern Med 2001; 15: 52–56. [DOI] [PubMed] [Google Scholar]
- 31. Syme HM, Markwell PJ, Pfeiffer D, Elliott J. Survival of cats with naturally occurring chronic renal failure is related to severity of proteinuria. J Vet Intern Med 2006; 20: 528–35. [DOI] [PubMed] [Google Scholar]
- 32. Jensen J, Henik RA, Brownfield M, Armstrong J. Plasma renin activity and angiotensin I and aldosterone concentrations in cats with hypertension associated with chronic renal disease. Am J Vet Res 1997; 58: 535–40. [PubMed] [Google Scholar]
- 33. Van Israel N, Desmoulins PO, Huyghe B, Burgaud S, Horspool LJI. Ramipril as a first line monotherapy for the control of feline hypertension and associated clinical signs [abstract]. J Vet Intern Med 2009; 23: 1331–32. [Google Scholar]
- 34. Elliott J, Fletcher MG, Souttar K, Cariese S, Syme HM. Effect of concomitant amlodipine and benazepril therapy in the management of feline hypertension [abstract]. J Vet Intern Med 2004; 18: 788. [Google Scholar]
- 35. King JN, Gunn-Moore DA, Tasker S, Gleadhill A, Strehlau G. Tolerability and efficacy of benazepril in cats with chronic kidney disease. J Vet Intern Med 2006; 20: 1054–64. [DOI] [PubMed] [Google Scholar]
- 36. Brown S, Haberman C, Morgan J. Evaluation of Doppler ultrasonic and oscillometric estimates of blood pressure in cats [abstract]. J Vet Intern Med 2001; 15: 281. [Google Scholar]