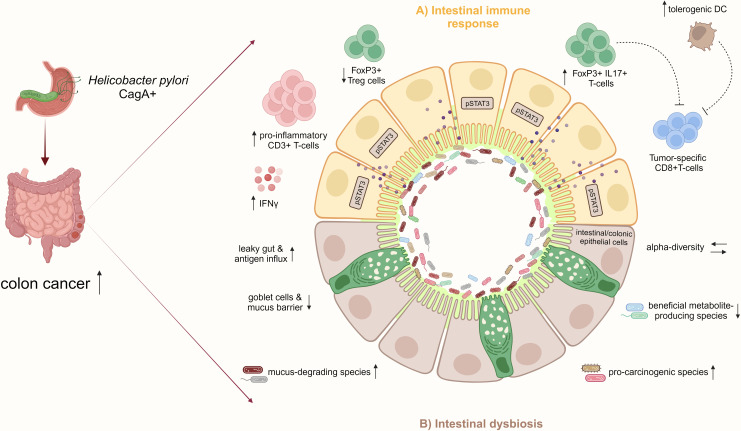
Figure 3.
H. pylori infection increases the risk for CRC by inducing pro-inflammatory immune responses and intestinal microbiome changes. (A) In the small and large intestinal epithelia, represented schematically in the illustration, H. pylori infection, particularly with CagA positive strains, promotes a pro-inflammatory immune response characterized by CD3+ T-cell infiltration and IFNγ secretion and activates pro-carcinogenic pSTAT3 signaling. Concomitant with the reduction of Treg cells, the infection induces pathogenic FoxP3+/IL-17+ T-cells, which may dampen tumor-specific CD8+ T-cells. Also, the increase of regulatory DCs by H. pylori may impair CD8+ T-cell effector functions contributing to colon cancer. (B) Furthermore, H. pylori infection indirectly affects the intestinal microbiota by increasing mucus-degrading and pro-carcinogenic species and reducing beneficial metabolite-producing bacteria. Together with the loss of mucus-producing goblet cells and intestinal barrier impairment, the infection results in a leaky gut and increased antigen influx, which further manifests as inflammation in the epithelium. These H. pylori-induced disturbances of the intestinal immunity and microbiome promote CRC development.