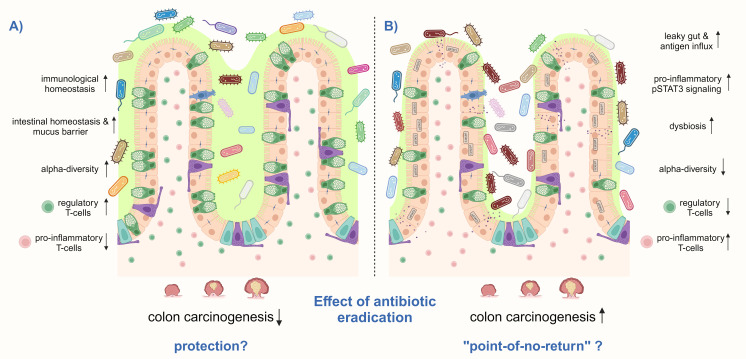
Figure 4.
H. pylori eradication treatment can have different effects on the risk for CRC. (A) H. pylori eradication may prevent CRC by increasing and decrease the detrimental effects of the infection, particularly by reducing pro-inflammatory CD3+ T-cells and pSTAT3 signaling and increasing regulatory T-cells, thereby inducing immunological homeostasis in the small intestine and colon. In addition, the number of mucus-producing goblet cells may be restored, as well as the intestinal epithelial barrier function. Antibiotic treatment might only induce short-term intestinal dysbiosis, which finally recovers to a healthy composition with high microbial diversity. (B) However, there may also be a “point-of-no-return” in infected hosts, in which H. pylori-induced changes in the intestinal and colonic immune response and microbiome get imprinted and remain after antibiotic eradication. High levels of pro-inflammatory T-cells together with a low number of regulatory Treg cells may remain, as well as persistent activation of pSTAT3 signaling. Furthermore, antibiotic therapy leads to microbial dysbiosis and a reduction of alpha-diversity. These changes contribute to a leaky gut with antigen influx leading to a vicious pro-inflammatory cycle. Thus, colon carcinogenesis can not anymore be prevented by H. pylori eradication. Shown is a schematic representation of the intestinal epithelium.