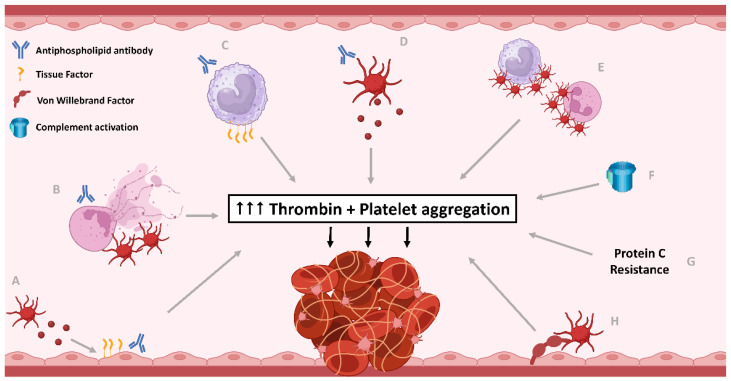
Figure 1.
The central role of excess thrombin generation and platelet activation in pathophysiological mechanisms contributing to thrombosis in antiphospholipid syndrome (APS). Antiphospholipid antibodies (aPL) have impact on many different cells and pathways leading to thrombosis. (A) Endothelial cells are directly impacted by aPL causing increased tissue factor (TF) expression, as well as indirectly with aPL-related platelet microparticle-induced endothelial pyroptosis, resulting in thrombin generation. (B) aPL induce neutrophils to release extracellular traps (NETs), as well as reduce NETs clearance and activate platelets which also lead to NET formation, which in turn activates platelets. Neutrophils also expose phosphatidylserine (PS) to increase thrombin generation. (C) aPL lead to increased tissue factor expression by monocytes, causing increased thrombin generation. (D) aPL induce platelet activation, aggregation, and PS exposure, releasing platelet microparticles, generating bursts of thrombin for fibrin clot stabilisation. (E) aPL-related platelet and leukocyte activation leads to platelet-leukocyte aggregate formation, which potentiates further platelet activation and thrombin generation. (F) The classical and alternative pathways of complement activation are upregulated in APS, with some evidence of lectin pathway also being involved. Complement activation contributes to platelet activation and thrombin generation. (G) Protein C cleaves and inactivates coagulation factors V and VIII, necessary for thrombin generation. Protein C resistance is evident in APS, with anti-Protein C antibodies in APS observed in some studies. (H) The quantity and activity of von Willebrand Factor (vWF) is increased in APS, resulting in increased platelet adhesion, activation, and aggregation. Created with Biorender.com.