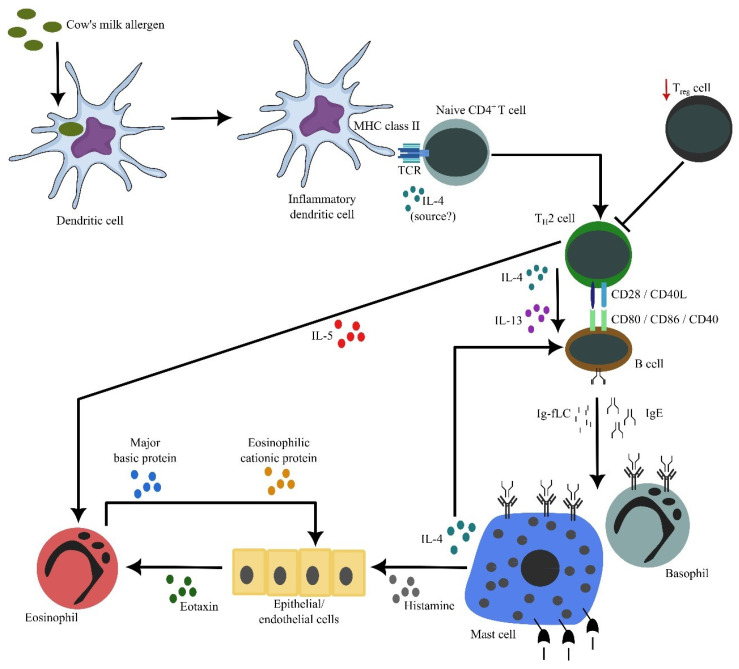
Figure 2.
The cascade of inflammation in cow’s milk allergy. Allergens’ exposure to inflammatory dendritic cells allow these cells to process and present allergen-derived peptides to naïve CD4+ T cells. In the presence of IL-4 (from an unknown source), naïve CD4+ T cells differentiate into proallergic TH2 cells. Concurrently, it appears that there is an impairment of TReg cell frequency and/or activity, resulting in a lack of suppression of TH2 cell activity. Subsequently, TH2 cells will drive B cells, via cell contact as well as secreted IL-4 and IL-13, to undergo immunoglobulin class switch recombination, in which they eventually produce IgE. Along with antibody production, B cells also secrete significant amounts of κ and λ Ig-free light chains (Ig-fLCs). IgE and Ig-fLCs will then bind to mast cells and basophils, causing sensitization. Following subsequent exposure to allergens, cross-linking of surface-bound antibodies occurs, causing mast cells and basophils to degranulate and release their biologically active substances, including histamine, IL-4 and IL-5. Secreted IL-4 amplifies the differentiation between TH2 and IgE-producing B cells, while secreted IL-5 by TH2 cells causes accumulation and activation of eosinophils in the affected tissues. Similarly, histamine causes epithelial or endothelial cells to release eotaxin that attracts eosinophils into the tissues. Activated eosinophils release active substances, including major basic and eosinophilic cationic proteins that are toxic to the surrounding cells, contributing to further inflammation. This figure is reproduced with permission from reference [32].