Abstract
Various infective complications can be seen after a dental procedure. They are rarely resistant to standard therapy. In the case we present, a case of preseptal cellulitis caused by pseudomonas oryzihabitans after tooth extraction in a male patient who did not have any underlying cause. As in our case, evaluation of the cases resistant to standard treatment in terms of drainage and multidisciplinary management of culture results together with infectious diseases will increase the treatment success rate.
Keywords: Pseudomonas oryzihabitans, preseptal cellulitis, infectious disease, dental procedure, nosocomial infection
Background
Pseudomonas oryzihabitans formerly known as flavimonas oryzihabitans is a non-fermentative, oxidase-negative, catalase-positive, motile gram-negative bacillus that is unusual and rarely causes disease in humans. The majority of cases are immunocompromised, post-operative patients, or dialysis patients with a catheter1. In this case, pseudomonas oryzihabitans, which is normally very rare, was detected in a patient who did not have a known immunodeficiency and presented with resistant periorbital cellulitis.
Case Report
A previously healthy 49-year-old male presented to the emergency department with a complaint of swelling around the left eye. According to patient history, it was learned that a tooth was extracted from the left-upper jaw 15 days ago.
After the procedure, the patient was given prophylactic amoxicillin-clavulanate and nonsteroidal anti-inflammatory drugs, but the patient states that he did not use them properly. His first admission to the hospital was ten days after the procedure with the complaint of swelling around the left eye. His antibiotherapy was extended to second-generation cephalosporin and antifungals. As he didn't get any cure with this treatment he admitted to our hospital. Physical examination revealed only left periorbital swelling and redness (Figure 1). In the eye examination of the patient, it was observed that the eye movements were normal and painless in all directions, and no discharge or redness was observed in the eye. No visual impairment was detected. Even though he received proper antibiotic therapy there wasn't any improvement therefore magnetic resonance imaging (MRI) was performed. According to this scan periorbital edema, increased soft tissue density, and collection were observed (Figure 2). Culture samples were taken from the collection area. No organism was found in direct microscopy, and intense leukocyte content was seen. The patient was discharged with the condition of following his culture results and getting clindamycin (3 times a day, 300 mg) and ceftriaxone (one time a day, 2 gr) empiric treatment by infectious diseases. Many oral regimen-resistant pseudomonas oryzihabitans have grown in the culture taken from the collection (Table 1). The patient was hospitalized in order to receive effective treatment. Intravenous meropenem treatment was started in doses of 1 gram, 3 times a day. After receiving intravenous-treatment for 12-days, all complaints of the patient regressed.
Figure 1.
Left periorbital swelling and redness
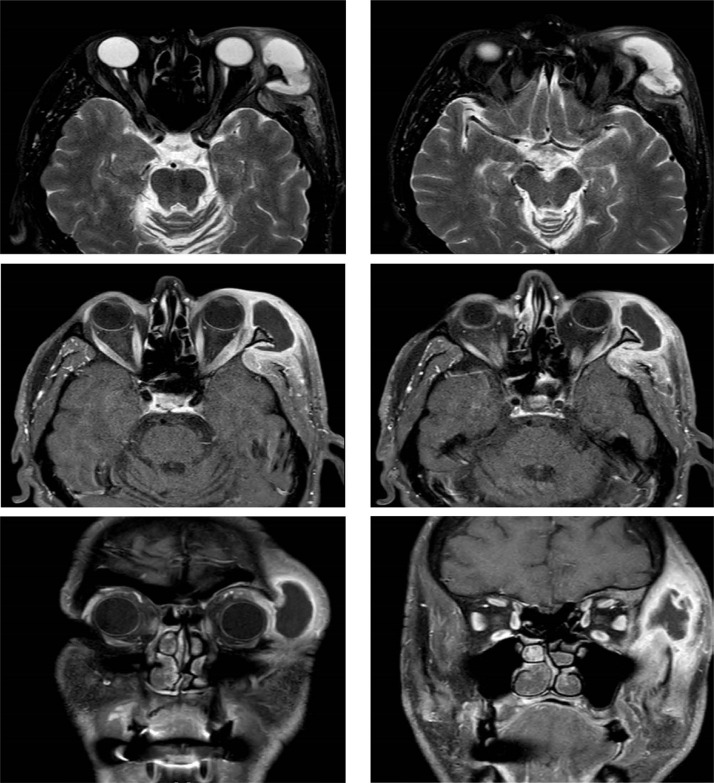
Figure 2.
Magnetic Resonance Imaging Showing Collection: A-B: T2 Axial View C-D: T1 Axial View E-F:T1 Coronal View
Table 1.
Culture antibiogram result of the sample taken from the collection
| Antibiotic | |
| Ampicillin | Resistant |
| Cefepime | Resistant |
| Ciprofloxacin | Resistant |
| Imipenem | Resistant |
| Meropenem | Sensitive |
| Piperacillin | Resistant |
Discussion
Various complications have been reported after dental procedures. These are often dental abscesses and respond well to antibiotics. In cases involving complex procedures, infections may progress to eye due to bone destruction2. Progression of the infection to the eye can cause significant morbidity and prompt diagnosis and treatment is required, therefore in such cases it is essential to check whether the infection has spread to the eye. Involvement in the extraocular muscles and adipose tissue around the eyes can often cause painful eye movements, proptosis and diplopia, and is very useful in diagnosing orbital cellulitis3. The absence of any of these conditions in our patient and the absence of any eye involvement on imaging allowed us to exclude the diagnosis of orbital cellulitis.
Preorbital cellulitis is a more benign diagnosis and often responds to oral antibiotics and non-steroidal therapy. Although various antibiotic regimens were tried to treat this condition in our patient, no response was obtained. The patient had to have repeated admissions for the same reason. The failure of our case to respond to various antibiotic regimens and the development of abscess formation required further investigation and treatment4. Drainage was provided, and culture tests were performed for microbiological factor analysis. There was a growth of pseudomonas oryzihabitans in culture. In cases that are resistant to treatment, the patient's condition should be followed closely. In addition, it should be remembered that multidisciplinary management with infectious diseases will increase the effectiveness of treatment. This is in the interest of both the patient and the physician.
Pseudomonas oryzihabitans often colonize in humid environments, so affected patients often have a history of prolonged exposure to water or a job where they worked in humid environments such as a cotton field. When the story of our patient was detailed, no exposure to a humid environment was detected and it was learned that he was working in the office. Also, pseudomonas oryzihabitans colonizes in humid materials in hospitals, such as sink drains, respiratory devices, and mechanical ventilators. Although it rarely infects humans, it is considered a potential pathogen of nosocomial infection, often seen in immunocompromised individuals or those with a device such as a catheter that may increase susceptibility to infection1. Our patient did not have any condition that increased the predisposition.
Another condition that increases the susceptibility to pseudomonas oryzihabitans is the history of previous surgery5. Although tooth extraction causes trauma, as far as we know, no case of Pseudomonas oryzihabitans has been reported after tooth extraction.
Pseudomonas oryzihabitans bacteremia was reported in the emergency department of a tertiary hospital in Korea in 2013. It was stated that this was caused by faulty aseptic preparation of a saline gauze canister6. The fact that our patient had a recent history of tooth extraction suggests that one of this equipment or materials may be contaminated with pseudomonas oryzihabitans. In addition, the fact that the bacteria in the antibiogram is more resistant than normal strengthens the thought that it may be of nosocomial origin. In our case, periorbital cellulitis developed after the dental procedure. Some features make this case remarkable. First, periorbital cellulitis was caused by pseudomonas oryzihabitans and normally occurs rarely in humans as a pathogen. Secondly, contrary to the literature, pseudomonas, seen in our case, is resistant to many oral treatments. Therefore, our patient was unsuccessful despite oral treatments, and many hospital admissions were made. Eventually, he was hospitalized and required intravenous treatment.
Declaration of competing interest
The authors report no conflicts of interest relevant to this article
Ethical statement
Informed consent was obtained from the patient to share his information and photograph.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authorship Contribution Statement
Emre Kudu: Investigation, Data curation, Writing- Original draft preparation. Faruk Danış: Investigation, Data curation, Writing – Original draft preparation. Sinan Karacabey: Investigation, Data curation, Writing – review & editing.
All authors contributed to the writing of the final manuscript.
References
- 1.Chaudhry HJ, Schoch PE, Cunha BA. Flavimonas oryzihabitans (CDC group Ve-2) Infect Control Hosp Epidemiol. 1992;13(8):485–488. doi: 10.1086/646578. [DOI] [PubMed] [Google Scholar]
- 2.Youssef OH, Stefanyszyn MA, Bilyk JR. Odontogenic orbital cellulitis. Ophthal Plast Reconstr Surg. 2008;24(1):29–35. doi: 10.1097/IOP.0b013e318160c950. [DOI] [PubMed] [Google Scholar]
- 3.Uzcátegui N, Warman R, Smith A, Howard CW. Clinical practice guidelines for the management of orbital cellulitis. Thorofare, NJ: SLACK Incorporated; 1998. pp. 73–79. [DOI] [PubMed] [Google Scholar]
- 4.Rudloe TF, Harper MB, Prabhu SP, Rahbar R, VanderVeen D, Kimia AA. Acute periorbital infections: who needs emergent imaging? Pediatrics. 2010;125(4):e719–e726. doi: 10.1542/peds.2009-1709. [DOI] [PubMed] [Google Scholar]
- 5.Panagopoulos GN, Megaloikonomos PD, Liontos M, et al. Pseudomonas oryzihabitans infected total hip arthroplasty. Journal of Bone and Joint Infection. 2016;1(1):54–58. doi: 10.7150/jbji.16967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woo K-S, Choi J-L, Kim B-R, et al. Outbreak of Pseudomonas oryzihabitans pseudobacteremia related to contaminated equipment in an emergency room of a tertiary hospital in Korea. Infection & chemotherapy. 2014;46(1):42–44. doi: 10.3947/ic.2014.46.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]